Abstract
Background and Objectives
Subjects and Methods
Results
Conclusion
Figures and Tables
 | Fig. 2Survival curve analysis describing the cumulative incidences of recurrent angina at 3 years. (A) Kaplan-Meyer curve analysis showed that in comparison to the non-CAS group, both the non-smoking CAS patient group and smoking CAS patient group showed cumulatively higher incidences of recurrent angina. (B) multivariable Cox proportional hazards regression showed that the smoking CAS patient group had a higher rate of recurrent angina than the non-CAS group, with smoking being the only difference (HR; 2.46, 95% CI; 1.46-4.13, p=0.001). CAS-: non-coronary artery spasm patient group, CAS+/Sm-: non-smoking CAS patient group, CAS+/Sm+: cigarette smoking CAS patient group, P1: p value by CAS- vs. CAS+/Sm-, P2: p value of CAS- vs. CAS+/Sm+, P3: p value by CAS+/Sm- vs. CAS+/Sm+, CAS: coronary artery spasm, HR: hazard ratio, CI: confidence interval, Ach: acetylcholine. |
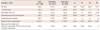
Table 1
Baseline clinical and angiographic clinical characteristics of the general study population

CAS-: non-coronary artery spasm patient group, CAS+/Sm-: "current" non-smoker CAS patient group, CAS+/Sm+: "current" smoker CAS patient group, P1: p value by CAS- vs. CAS+/Sm-, P2: p value of CAS- vs. CAS+/Sm+, P3: p value of CAS+/Sm- vs. CAS+/Sm+, CAS: coronary artery spasm, LVEF: left ventricular ejection fraction, ARB: angiotensin receptor blockers, ACEI: angiotensin converting enzyme inhibitors. *p values were expressed to be statistically significances among the three groups
Table 2
Cumulative clinical outcomes at 3 years
CAS-: non-coronary artery spasm patient group, CAS+/Sm-: "current" non-smoker CAS patient group, CAS+/Sm+: "current" smoker CAS patient group, P1: p value of CAS- vs. CAS+/Sm-, P2: p value of CAS- vs. CAS+/Sm+, P3: p value by CAS+/Sm- vs. CAS+/Sm+, CAS: coronary artery spasm, ns: not significant (p value >0.999). *p values were expressed to be statistically significances among the three groups




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download