Abstract
Background and Objectives
There is controversy surrounding whether or not high dose statin administration before percutaneous coronary intervention (PCI) decreases peri-procedural microvascular injury. We performed a prospective randomized study to investigate the mechanisms and effects of pre-treatment high dose atorvastatin on myocardial damage in patients with non-ST-segment elevation acute coronary syndrome (NSTE-ACS) undergoing PCI.
Subjects and Methods
Seventy seven patients with NSTE-ACS were randomly assigned to either the high dose group (atorvastatin 80 mg loading 12 to 24 h before PCI with a further 40 mg loading 2 h before PCI, n=39) or low dose group (atorvastatin 10 mg administration 12 to 24 h before PCI, n=38). Index of microcirculatory resistance (IMR) was measured after stent implantation. Creatine kinase-myocardial band (CK-MB) and high sensitivity C-reactive protein (CRP) levels were measured before and after PCI.
Results
The baseline characteristics were not different between the two patient groups. Compared to the low dose group, the high dose group had lower post PCI IMR (14.1±5.0 vs. 19.2±9.3 U, p=0.003). Post PCI CK-MB was also lower in the high dose group (median: 1.40 ng/mL (interquartile range [IQR: 0.75 to 3.45] vs. 4.00 [IQR: 1.70 to 7.37], p=0.002) as was the post-PCI CRP level (0.09 mg/dL [IQR: 0.04 to 0.16] vs. 0.22 [IQR: 0.08 to 0.60], p=0.001).
Percutaneous coronary intervention (PCI) with drug-eluting stents and pharmacological management such as antiplatelet agents and statins constitutes the therapeutic mainstay for patients with acute coronary syndrome.1) However, PCI may cause peri-procedural myocardial injury which is associated with adverse in-hospital outcomes and a worse overall prognosis.2)3) Previous studies suggest that even short-term administration of statins before PCI may provide clinical benefit and reduce the incidence of peri-procedural myocardial infarction (MI).4)5)6) However, its mechanism has not been clearly defined. Furthermore, recent studies have raised controversy over the effects of high dose statins in the prevention of peri-procedural myocardial injury and the improvement of clinical outcome.7)8)
The Index of microcirculatory resistance (IMR) is an invasive physiologic index which interrogates the status of coronary microvasculture.9) IMR can be reliably measured in a cardiac catheterization laboratory and is not influenced by hemodynamic conditions, unlike coronary flow reserve (CFR). Recent works have highlighted the clinical usefulness of this index in the evaluation of the coronary microvasculature.9)10) In patients with MI, IMR has been reported to have prognostic value.10)
We performed this study to evaluate the effects of pre-PCI loading of high dose atorvastatin on peri-procedural myocardial damage by measuring post-PCI IMR with serial measurement of cardiac enzymes and high sensitivity C-reactive protein levels (CRP) in patients with non-ST-segment elevation acute coronary syndrome (NSTE-ACS).
The RESIST-ACS (pRE-treatment with high dose atorvaStatIn for the prevention of microvaScular dysfunction after percutaneous coronary inTervention in patients with Acute Coronary Syndrome) study (ClinicalTrials.gov number, NCT01491256) is a multicenter, randomized, prospective clinical trial performed in four Korean University Hospitals (Kangwon National University Hospital, Keimyung University Dongsan Medical Center, Inje University Ilsan Paik Hospital, and Seoul National University Hospital). Patients who were scheduled for early coronary angiography (<48 hours) for suspicious NSTE-ACS (unstable angina or non-ST-segment elevation acute myocardial infarction) between 18 and 85 years old were consecutively included. Exclusion criteria were as follows: ST-segment elevation acute myocardial infarction, high-risk features needing emergency coronary angiography, any increase in liver enzymes (alanine aminotransferase and aspartate aminotransferase), left ventricular ejection fraction<30%, renal dysfunction with serum creatinine>2.0 mg/dL, total occlusion of culprit vessel, 3-vessel disease, left main stenosis, lesion at distal segments or branches, lesion with marked calcification, presence of definite thrombus or extreme tortuosity, contraindication to adenosine, a history of previous myocardial infarction, a history of coronary artery bypass surgery and a history of previous statin therapy within three months.
Between March 2010 and May 2012, 205 patients who underwent coronary angiography were screened according to clinical inclusion and exclusion criteria (Fig. 1). Eligible patients were randomized to receive high dose atorvastatin loading (80 mg loading given 12 to 24 h before coronary angiography, with a further 40 mg dose 2 h before PCI) or low dose atorvastatin (10 mg given 12 to 24 h before PCI). After coronary angiography, 128 patients (65 randomized to high dose arm and 63 to control arm) were additionally excluded; 82 patients for no significant stenosis, three for left main lesion, 11 for lesions at branch or distal segment, 10 for total occlusion, 12 for 3-vessel disease, three for failure to cross pressure wire, and seven for markedly calcified or thrombotic lesion. Therefore, 77 patients who underwent PCI immediately after diagnostic angiography represent the study population. According to the protocol, patients were pre-treated with aspirin (300 mg loading dose) and clopidogrel (600 mg loading dose at least three h before the procedure).11) Before PCI, patients received intravenous heparin with a target activated clotting time of >300 seconds. Glycoprotein IIb/IIIa inhibitors were used at the operator's discretion. Blood samples were collected before and at six and 12 hours after PCI to measure CRP, creatine kinase-myocardial band (CK-MB) and total creatine kinase (CK) levels. After PCI, the maintenance dose of atorvastatin was determined at the physician's discretion. The study complies with the Declaration of Helsinki and was approved by the institutional review board at each participating center. All patients provided written informed consent.
All procedures were performed using standard techniques. The fractional flow reserve (FFR) was measured before and after PCI, and CFR, IMR and wedge pressure (Pw) were measured after PCI by methods described previously.9)12) In brief, a pressure-temperature sensor guide wire (Certus Pressure Wire, St. Jude, St. Paul, MN, USA) was used for physiologic measurements. With the sensor positioned at the tip of the catheter, the pressure from the wire was equalized with that of the guiding catheter. The pressure sensor was positioned two thirds of the way down the culprit artery. After intracoronary nitroglycerin administration (100-200 µg), three injections of 3-4 mL of room-temperature saline were introduced into the coronary artery, and the resting mean transit time (Tmn) was measured. Intravenous infusion of adenosine (140 µg/kg/min) was then administered via the femoral vein or large peripheral vein to induce steady state maximal hyperemia. Then, three more injections of 3-4 mL of room temperature saline were administered, and the hyperemic Tmn was measured. Simultaneous measurements of mean aortic pressure (Pa, by guiding catheter) and mean distal coronary pressure (Pd, by pressure wire) were also made during maximal hyperemia. CFR was calculated as resting Tmn divided by hyperemic Tmn. IMR was calculated as the Pd at maximal hyperemia divided by the inverse of the hyperemic Tmn.9) FFR was calculated by the ratio of (mean Pd)/(mean Pa) at maximal hyperemia.12) The Pw was measured after 60-second balloon occlusion of the target lesion, as well as before and after stent deployment with concurrent measurement of Pa. In cases of significant stenosis (FFR≤0.75), an expanded formula (IMR=PaxTmnx[Pd-Pw]/[Pa-Pw]) was applied to calculate the true IMR that incorporates coronary Pw to account for collateral flow.13)
The mean post-PCI IMR value of patients in the low dose group was expected to be 26±12 according to previous study results.9)14)15) A 30% reduction of post-PCI IMR value was hypothesized in the high dose atorvastatin loading group. A total sample size of 76 patients would provide 80% power to detect this difference with a significance level of 0.05. The distributional assumption of normal populations required for the two sample t-statistic was justified by using the Kolmogorov-Smirnov test and was visually double-checked by using normal quantile-quantile plots. For categorical variables, chi-square tests were used to test homogeneity between populations.
For continuous variables, Student's t-tests or Wilcoxon rank-sum tests were used to test for mean differences between populations. The results of statistical tests were summarized as mean±standard deviation for the two sample t-test and median with inter-quartile range for the Wilcoxon rank-sum test. Multivariable logistic regression analysis was performed to determine the independent predictive factors of microcirculatory impairment after PCI. For a two-sided hypothesis test, p-value less than 0.05 is considered significant. Statistical analyses were performed using the SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA).
Clinical and procedural features in the high dose (39 patients) and low dose (38 patients) groups are shown in Table 1. There were no significant differences between the two groups in age, gender, prevalence of cardiovascular risk factors, current medications, metabolic profiles, left ventricular function, and clinical presentation. Angiographic and procedural characteristics were also comparable in both groups for coronary anatomy, lesion type, procedural characteristics, diameter and length of implanted stents, and the use of glycoprotein IIb/IIIa inhibitors (Table 2). Drug-eluting stents were used in all patients. Procedural success was obtained in all patients and there were no procedure-related complications in either group. No patient experienced statin-related adverse events, such as liver enzyme elevation or myopathy.
After PCI, physiological parameters such as FFR, CFR, IMR, and Pw were successfully obtained in all patients. Post PCI IMR value, the primary end point of this study, was significantly lower in the high dose group than in the low dose group (14.1±5.0 U vs. 19.2±9.3 U, p=0.003) (Fig. 2). Incidence of microcirculatory impairment was also lower in the high dose group (2.6% vs. 23.7%, p=0.007) (Table 3). Post-PCI FFR, CFR, and Pw values were similar between the two groups. Pre-PCI FFR, CFR, IMR, and Pw values were also comparable, but pre-PCI physiological values were measured in only 38 patients (17 in the study group and 21 in the low dose group) since measurement before PCI was not protocol-mandated.
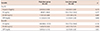
The baseline levels of total CK, CK-MB and CRP were comparable between the two groups. Post-PCI CK-MB (median 1.40 [interquartile range (IQR): 0.75 to 3.45] vs. 4.00 ng/mL [IQR: 1.70 to 7.37], p=0.002) and CRP (0.09 [IQR: 0.04 to 0.16] vs. 0.22 mg/dL [IQR: 0.08 to 0.60], p=0.001) were significantly lower in the high dose group (Table 4). When CK, CK-MB and CRP levels before and after PCI were compared, CK-MB (1.70 [IQR: 1.09 to 2.73] vs. 4.00 ng/mL [1.70 to 7.37], p=0.001) and CRP (0.12 [IQR: 0.04 to 0.30] vs. 0.22 [0.08 to 0.60], p<0.001) levels showed significant elevation after PCI in the low dose group, but not in the high dose group (Fig. 3). The CK-MB levels showed a weak positive correlation with post-PCI IMR values (r=0.238, p=0.041) (Fig. 4).
By univariate analyses, high dose atorvastatin loading (odd ratio [OR] 0.117, 95% confidence interval [CI] 0.014 to 0.999; p=0.050) and pre-dilatation balloon pressure (OR 1.353, 95% CI 0.945 to 1.938; p=0.099) were explored as potential predictors of post-PCI microcirculatory impairment. Multivariable logistic regression analysis identified pretreatment with high dose atorvastatin as the only independent predictor (OR 0.089, 95% CI 0.009 to 0.843; p=0.035) for post-PCI microcirculatory impairment.
The results of RESIST-ACS trial indicate that a short-term pre-treatment with high-dose atorvastatin loading before PCI can reduce peri-procedural myocardial injury verified by post-PCI IMR in patients with NSTE-ACS compared to low dose statin therapy. As the high dose group had lower IMR and lower CRP than the low dose group, this effect seems to be mediated improved microvascular function and less inflammation.
Microcirculatory impairment is closely related with myocardial damage and adverse outcomes in various clinical situations. Gibson et al. demonstrated that patients with impaired thrombolysis in myocardial infarction (TIMI) perfusion grade had a 10-fold-higher incidence of post-procedural CK-MB elevation.17) Bolognese et al. found using a combination of TIMI flow grade, corrected TIMI frame count, TIMI perfusion grade, and myocardial contrast echocardiography, that post-PCI cardiac troponin I elevation in high-risk patients with ACS was associated with an abnormal tissue-level perfusion.18) Recently, IMR has been shown to be a reliable and reproducible index to evaluate coronary microvascular function with less interference by other hemodynamic changes.19) Fearon et al. reported that high IMR measured after primary PCI was associated with low left ventricular function at three month follow-up and reduced long-term survival.14) Furthermore, Pepine et al. reported that a limited coronary microvascular response to adenosine is associated with increased risk for major adverse outcomes, even in the absence of significant obstructive coronary artery disease.20) In agreement with previous findings, our study showed that the assessment of microvascular function using IMR during the invasive procedure can be helpful in the evaluation of ACS patients. The low post-PCI IMR in the high dose atorvastatin group was associated with less myocardial damage, represented by less CK-MB elevation. As expected, there was no difference in FFR between the two groups; however, there was also no difference in CFR and Pw/Pa between the two groups in our study, in contrast to IMR.
Previous randomized controlled trials demonstrated that pretreatment with atorvastatin can reduce PCI induced myocardial damage,4)5) while a recent study by Jang et al.6) showed that a high loading dose of atorvastatin did not translate into clinical benefit over the usual atorvastatin administration (40 mg/day) in patients with NSTE-ACS. When we compared the incidence of post-PCI myocardial infarction defined as CK-MB>3 times the upper limit of normal, there was no significant difference between the two groups. However, we conducted this randomized trial focused on coronary microvascular function after PCI and showed the beneficial effect of high-dose atorvastatin loading on preventing microvascular dysfunction in patients with NSTE-ACS.
Despite the significant difference of post-PCI IMR between the two groups, post-PCI CFR, and Pw values were comparable. This may be due to CFR being influenced by various hemodynamic conditions and that Pw value is less sensitive to the changes of microvascular status than IMR.
Suggested pathophysiology of peri-procedural myocardial injury includes embolism of atheromatous and thrombotic debris, platelet activation and thrombosis, neurohormonal activation and modulation of vascular and myocardial functions, oxidative stress and inflammation.21)22) Atorvastatin is the most widely used 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor. In addition to beneficial lipid modulation effects, its benefits in ACS begin early, suggesting its pleiotropic effects,23)24) such as improving or restoring endothelial function, enhancing the stability of atherosclerotic plaques, and decreasing oxidative stress and vascular inflammation.25)
It has been demonstrated that increased myocardial CRP levels are associated with endothelial toxicity and reduced cardiac microvessel density in cardiovascular disease specimens.26) Previous studies have demonstrated that an inflammatory status with increased CRP levels at the time of PCI may increase subsequent clinical events or myocardial damage.27)28) Post-PCI CRP levels in the high dose loading group were significantly lower than in the low dose group in our study, supporting the anti-inflammatory actions of atorvastatin seen in previous studies.29)30) As there was no difference in baseline clinical characteristics and CRP levels between the high and low dose groups, the difference in post-PCI CRP levels likely result from the effects of the study drug.
First, this study was not a blinded study, with a relatively small study population. Second, the criterion for microcirculatory impairment used in this study was defined based on previous studies and there is no conclusive evidence on the cut-off value of microvascular impairment. However, previous studies in asymptomatic, normal control subjects have found that the normal IMR is <25.14)15)16) Third, pre-PCI measurements of IMR, CFR and wedge pressure were not mandatory and the comparison of these parameters between pre- and post-PCI was not available in all patients. Finally, we could not assess the association between post-PCI microcirculatory impairment and adverse clinical outcomes due to limited sample size.
Figures and Tables
Fig. 1
Study design and flow. ACS: acute coronary syndrome, PCI: percutaneous coronary intervention, CRP: C-reactive protein, CK-MB: creatine kinase-myocardial band, CK: creatine kinase, FFR: fractional flow reserve, DES: drug-eluting stent, IMR: index of microcirculatory resistance, CFR: coronary flow reserve, Pw: wedge pressure.

Fig. 2
Distribution of post-PCI IMR values among patients treated with and without high dose atorvastatin loading before PCI. IMR: index of microcirculatory resistance, PCI: percutaneous coronary intervention.

Fig. 3
Box plots comparing CK-MB levels before and after stenting in the two groups. The median, interquartile range (IQR) and 1.5 IQR for each group are shown. Comparison was performed by Man-Whitney and Wilcoxon tests. CK-MB: creatine kinase-myocardial isoenzyme, PCI: percutaneous coronary intervention.

Fig. 4
Scatterplots of the relationship between post-PCI IMR values and post-PCI CK-MB levels. PCI: percutaneous coronary intervention, IMR: index of microcirculatory resistance, CK-MB: creatine kinase-myocardial isoenzyme.
Table 1
Baseline clinical characteristics of the patients
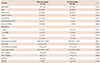
Variables are mean±standard deviation, n (%) or median (interquartile range) depending on normality criteria. CAD: coronary artery disease, ACEI: angiotensin-converting enzyme inhibitors, ARB: angiotensin receptor blockers, CCB: calcium channel blocker, HbA1c: hemoglobin A1c, LDL-C: low-density lipoprotein cholesterol, HDL-C: high-density lipoprotein cholesterol, LVEF: left ventricular ejection fraction, NSTEMI: non-ST-segment elevation myocardial infarction
Table 2
Procedural features

Table 3
Coronary physiological parameters
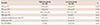
Table 4
Changes of serum biomarkers before and after stent implantation
Acknowledgements
This study was supported by a grant from the Korean Society of Cardiology (2009).
Dr. Bon-Kwon Koo received institutional research grant from St. Jude Medical. Dr. Fearon received grants from St. Jude Medical, grants and personal fees from Medtronics, other from Heart Flow, outside the submitted work.
References
1. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011; 58:e44–e122.
2. Prasad A, Singh M, Lerman A, Lennon RJ, Holmes DR Jr, Rihal CS. Isolated elevation in troponin T after percutaneous coronary intervention is associated with higher long-term mortality. J Am Coll Cardiol. 2006; 48:1765–1770.
3. Fuchs S, Kornowski R, Mehran R, et al. Prognostic value of cardiac troponin-I levels following catheter-based coronary interventions. Am J Cardiol. 2000; 85:1077–1082.
4. Patti G, Pasceri V, Colonna G, et al. Atorvastatin pretreatment improves outcomes in patients with acute coronary syndromes undergoing early percutaneous coronary intervention: results of the ARMYDA-ACS randomized trial. J Am Coll Cardiol. 2007; 49:1272–1278.
5. Briguori C, Visconti G, Focaccio A, et al. Novel approaches for preventing or limiting events (Naples) II trial: impact of a single high loading dose of atorvastatin on periprocedural myocardial infarction. J Am Coll Cardiol. 2009; 54:2157–2163.
6. Jang Y, Zhu J, Ge J, Kim YJ, Ji C, Lam W. Preloading with atorvastatin before percutaneous coronary intervention in statin-naïve Asian patients with non-ST elevation acute coronary syndromes: a randomized study. J Cardiol. 2014; 63:335–343.
7. Veselka J, Zemánek D, Hájek P, et al. Effect of two-day atorvastatin pretreatment on long-term outcome of patients with stable angina pectoris undergoing elective percutaneous coronary intervention. Am J Cardiol. 2011; 107:1295–1299.
8. Zemánek D, Branny M, Martinkovičová L, et al. Effect of seven-day atorvastatin pretreatment on the incidence of periprocedural myocardial infarction following percutaneous coronary intervention in patients receiving long-term statin therapy. A randomized study. Int J Cardiol. 2013; 168:2494–2497.
9. Fearon WF, Balsam LB, Farouque HM, et al. Novel index for invasively assessing the coronary microcirculation. Circulation. 2003; 107:3129–3132.
10. Fearon WF, Low AF, Yong AS, et al. Prognostic value of the index of microcirculatory resistance measured after primary percutaneous coronary intervention. Circulation. 2013; 127:2436–2441.
11. Patti G, Colonna G, Pasceri V, Pepe LL, Montinaro A, Di Sciascio G. Randomized trial of high loading dose of clopidogrel for reduction of periprocedural myocardial infarction in patients undergoing coronary intervention: results from the ARMYDA-2 (Antiplatelet therapy for Reduction of MYocardial Damage during Angioplasty) study. Circulation. 2005; 111:2099–2106.
12. Fearon WF, Nakamura M, Lee DP, et al. Simultaneous assessment of fractional and coronary flow reserves in cardiac transplant recipients: Physiologic Investigation for Transplant Arteriopathy (PITA Study). Circulation. 2003; 108:1605–1610.
13. Aarnoudse W, Fearon WF, Manoharan G, et al. Epicardial stenosis severity does not affect minimal microcirculatory resistance. Circulation. 2004; 110:2137–2142.
14. Fearon WF, Shah M, Ng M, et al. Predictive value of the index of microcirculatory resistance in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2008; 51:560–565.
15. Melikian N, Vercauteren S, Fearon WF, et al. Quantitative assessment of coronary microvascular function in patients with and without epicardial atherosclerosis. EuroIntervention. 2010; 5:939–945.
16. Lee BK, Lim HS, Fearon WF, et al. Invasive evaluation of patients with angina in the absence of obstructive coronary artery disease. Circulation. 2015; 131:1054–1060.
17. Gibson CM, Murphy SA, Marble SJ, et al. Relationship of creatine kinase-myocardial band release to Thrombolysis in Myocardial Infarction perfusion grade after intracoronary stent placement: an ESPRIT substudy. Am Heart J. 2002; 143:106–110.
18. Bolognese L, Ducci K, Angioli P, et al. Elevations in troponin I after percutaneous coronary interventions are associated with abnormal tissue-level perfusion in high-risk patients with non-ST-segment-elevation acute coronary syndromes. Circulation. 2004; 110:1592–1597.
19. Ng MK, Yeung AC, Fearon WF. Invasive assessment of the coronary microcirculation: superior reproducibility and less hemodynamic dependence of index of microcirculatory resistance compared with coronary flow reserve. Circulation. 2006; 113:2054–2061.
20. Pepine CJ, Anderson RD, Sharaf BL, et al. Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia results from the National Heart, Lung and Blood Institute WISE (Women's Ischemia Syndrome Evaluation) study. J Am Coll Cardiol. 2010; 55:2825–2832.
21. Herrmann J. Peri-procedural myocardial injury: 2005 update. Eur Heart J. 2005; 26:2493–2519.
22. Prasad A, Herrmann J. Myocardial infarction due to percutaneous coronary intervention. N Engl J Med. 2011; 364:453–464.
23. Cannon CP, Braunwald E, McCabe CH, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004; 350:1495–1504.
24. Schwartz GG, Olsson AG, Ezekowitz MD, et al. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: the MIRACL study: a randomized controlled trial. JAMA. 2001; 285:1711–1718.
25. Takemoto M, Liao JK. Pleiotropic effects of 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitors. Arterioscler Thromb Vasc Biol. 2001; 21:1712–1719.
26. Joshi MS, Tong L, Cook AC, et al. Increased myocardial prevalence of C-reactive protein in human coronary heart disease: direct effects on microvessel density and endothelial cell survival. Cardiovasc Pathol. 2012; 21:428–435.
27. Ahmed K, Jeong MH, Chakraborty R, et al. Prognostic impact of baseline high-sensitivity C-reactive protein in patients with acute myocardial infarction undergoing percutaneous coronary intervention based on body mass index. Korean Circ J. 2012; 42:164–172.
28. Patti G, Mangiacapra F, Ricottini E, et al. Correlation of platelet reactivity and C-reactive protein levels to occurrence of peri-procedural myocardial infarction in patients undergoing percutaneous coronary intervention (from the ARMYDA-CRP study). Am J Cardiol. 2013; 111:1739–1744.
29. Correia LC, Spósito AC, Lima JC, et al. Anti-inflammatory effect of atorvastatin (80 mg) in unstable angina pectoris and non-Q-wave acute myocardial infarction. Am J Cardiol. 2003; 92:298–301.
30. Kinlay S, Schwartz GG, Olsson AG, et al. High-dose atorvastatin enhances the decline in inflammatory markers in patients with acute coronary syndromes in the MIRACL study. Circulation. 2003; 108:1560–1566.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download