Abstract
Standard endovascular repair of iliac/aortoiliac pathologies can lead to complications, such as buttock claudication, colon ischemia and erectile dysfunction. Branch grafts have been developed but require at least 6 weeks for customization and are not currently available in China; they are also quite expensive. To our knowledge, modified fenestrated stent grafts (MFSGs) are a safe and effective alternative for treating patients with juxtarenal aneurysms. Most MFSGs are used for the preservation of renal and left subclavian arteries. Few cases of MFSGs have been reported in the treatment of iliac pathologies. The use of an MFSG is decided on a case-by-case basis. This report presents our first clinical use of an MFSG for preservation of the internal iliac artery.
Isolated dissection of the iliac artery without aortic involvement is exceedingly rare. Endovascular treatment of aortic pathologies has become the predominant form of repair.1) Standard endovascular repair of aortic pathologies, in which the internal iliac artery is generally embolized, can lead to complications, such as buttock claudication, colon ischemia, and erectile dysfunction.2) Therefore, antegrade flow of the internal iliac artery should be conserved, particularly in young patients. To address this problem, various scalloped, fenestrated, and branched aortic stent grafts have been developed and studied. Most of these stent grafts are dedicated iliac branch grafts that require at least a 6-week customization period and are very costly.3) Also, they are currently unavailable for use in China. Modified fenestrated stent grafts (MFSGs) are a safe and effective alternative for treatment of patients with juxtarenal aneurysms, for whom no other alternatives are available. Only a few cases of MFSG use in the treatment of iliac pathologies have been reported.4) The current report describes the treatment of isolated iliac dissection with an MFSG with preservation of the internal iliac artery.
A 54-year-old man was admitted with complaints of backache that had lasted two weeks. The pain was intermittent. He was normotensive and had no history of smoking, diabetes, or trauma. No family history of vascular disease was reported. Physical examination revealed normal femoral and distal pulses without any palpable mass. Cross-sectional computed tomography (CT) and three-dimensional reconstructed images showed a slightly dilated common iliac artery (CIA), as well as dissection from the CIA to the external iliac artery with intimal tears in the CIA, without dilation of the internal iliac artery (Fig. 1).
Given the patient's age, possible inflammatory adhesion around the dissection, absence of dilation of the internal artery, and the desire to minimize the risks of colon ischemia, buttock claudication, and impotence, we proceeded with an attempt at endovascular dissection repair with an MFSG.
The modified graft was created using a 16 mm×13 mm×80 mm Endurant stent graft (Medtronic, Minneapolis, MN, USA). The first six stents of the graft were deployed, leaving the remaining stents loaded in the sheath. A sterile marking pen was used to mark the location of the fenestrations based on both length and clock face measurements that had been previously determined with image reconstruction software (GE ADW4.5, Connecticut, USA). An ophthalmologic cautery was used to carefully burn the Dacron fabric to create the fenestration (Fig. 2). The stent strut from the original iliac stent graft limb was secured to the polyester graft with continuous 6-0 Prolene sutures. A longitudinal radiopaque marker was sutured to the polyester graft for orientation just below the position of the fenestrated ostium using 6-0 Prolene sutures (Ethicon, West Somerville, NJ, USA) (Fig. 3). The modified graft was resheathed into the original sheath using interrupted silk sutures to collapse each stent.
An aortogram revealed right iliac dissection with intimal tears in the common iliac artery, which was limited to the proximal end of the external iliac artery at the left anterior oblique (LAO) 40°+caudal (CAUD) 15° projection angle (Fig. 4). Proper orientation of the graft was confirmed by rotating the MFSG clockwise under fluoroscopy and adjusting the longitudinal radiopaque marker to the level of the internal iliac artery. The graft was then carefully deployed at the opening of the ipsilateral limb. We placed a 16 mm×13 mm×80 mm Medtronic Endurant endograft below the aortic bifurcate with the distal end positioned at the external iliac artery. The longitudinal radiopaque marker revealed the direction of the internal iliac artery. The aortogram revealed that the iliac dissection successfully excluded and preserved the flow of the internal iliac artery. Endoleaks Ib and IV were also observed (Fig. 5). Thus, a 12 mm×40 mm Fluency cover stent (Bard, Karlsruhe, Germany) was placed distally to extend to the landing zone and ballooned with a Coda balloon. Repeat angiography showed intact flow into the internal iliac artery covering the dissection and a narrowed endoleak IV, while endoleak Ib had disappeared (Fig. 6).
The patient recovered uneventfully. No buttock claudication, colon ischemia, or erectile dysfunction occurred. The patient was discharged 4 days after the procedure.
Three-dimensional reconstructed CT images 5 months later revealed no endoleaks and showed a patent right internal iliac artery. The preplanned fenestration was aligned with the vessel ostia (Fig. 7).
Reports of isolated iliac artery dissection in the literature are rare. Most cases are related to Marfan syndrome, pregnancy, fibromuscular dysplasia, alpha-1-antitrypsin deficiency, athletic training, or atherosclerosis. Endovascular treatment is becoming more popular in aortic pathologies.5)6)7)8) The risks of internal iliac artery embolization have been well described. Preservation of pelvic flow is crucial in various circumstances.2)9) The advent of fenestrated endovascular aortic repair, which can reduce aortic pathologies while preserving blood flow to major organs through visceral branches by using fenestrated stent grafts (FSGs), increases the possibility for treatment of these aortic pathologies. However, most FSGs are focused on the use of an iliac branch device or in situ FSG for endovascular treatment of iliac/aortoiliac pathologies.3) MFSGs are a safe and effective alternative for treatment of patients with juxtarenal aneurysms, in which no other alternatives are available.10)
In this study, we demonstrated endovascular treatment of iliac/aortoiliac pathologies with an MFSG. The effectiveness of this procedure is exhibited by preservation of the internal iliac artery, which showed favorable patency. To our knowledge, most MFSGs are used for preservation of renal and left subclavian arteries.11)12) Few cases of MFSG use in the treatment of iliac/aortoiliac pathologies have been reported.4) The current report presents our first clinical use of an MFSG for preservation of the internal iliac artery.
Preprocedural planning and some anatomical and technical considerations were taken into consideration. Measurements of the abdominal aorta and iliac arteries, as well as deployment of longitudinal radiopaque marker, were of paramount importance. Several anatomical and related factors may limit the widespread applicability of this technique. Patient access vessels must be of adequate diameter to accommodate large sheaths and areas of narrowing or tortuosity within the iliac system may prevent device advancement and positioning.
Hence, the choice of MFSG must be made on a case-by-case basis. Several factors supported our use of an MFSG in this case. First, dedicated iliac branch grafts have been developed and tested but are currently unavailable for use because of a lack of approval from the China Food and Drug Administration; they also require at least 6 weeks for customization and are more complicated than standard endovascular aortic repair. Second, in situ FSG is theoretically another endovascular alternative.13) So far, in situ FSG has mainly been used to preserve the left subclavian artery; there are no published reports of an in situ FSG being used to treat iliac/aortoiliac pathologies. Finally, the absences of severe vessel tortuosity, iliac anatomies, and internal artery dilatation are prerequisites for the selection of an MFSG.
As a result, for this case, use of an MFSG avoids the need to construct a branched limb and may require minimal or no device modifications compared with other cases.
The selection of the proper projection angle is a critical step for the MFSG procedure. LAO 40°+CAUD 15°, which are optimal projection angles for displaying the tear of iliac dissection, maintained the internal and external iliac arteries in the same plane for the current case. Accurate projection angles can improve alignment in the fenestrated ostium.
In addition to an MFSG, other technologies may preserve the internal iliac artery. Such techniques include sandwich technology and the bell-bottom technique. In the bell-bottom technique, the landing zone is usually located in a diseased segment of the common iliac artery, which can lead to future growth and development of a type Ib endoleak and has a 4% reintervention rate.14) The sandwich technique may be difficult in patients with short common iliac arteries along with a narrow-caliber external iliac artery on the same side.15) This technique would have been a viable alternative in the current case, but the cost of treatment would have increased.
In conclusion, we report our first clinical case of MFSG usage for preservation of the internal iliac artery. MFSG use is feasible and can be applied with devices available in most endovascular centers. It may become the best option due to comparative effectiveness and low cost if it can be shown to be just as safe and effective as commercially available custom devices. What's more, an MFSG may be used in urgent or emergent cases (symptomatic or ruptured aneurysms), in patients considered hemodynamically stable. The success of fenestrated endovascular iliac/aortoiliac pathologies can facilitate treatment of aortic pathologies involving visceral arteries. The short-term follow-up in this case indicated that the technique was successful, but there are still uncertainties regarding the long-term stability of the stent graft. Further studies are required to evaluate its long-term effectiveness and assess any possible reinterventions associated with modified fenestrated stent grafts.
Figures and Tables
Fig. 1
Three-dimensional reconstructed images show a slightly dilated common iliac artery (CIA), as well as dissection from the CIA to the external iliac artery with intimal tears in the CIA, without dilation of the internal iliac artery.
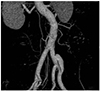
Fig. 2
An ophthalmologic cautery was used to carefully burn the Dacron fabric to create the fenestration.

Fig. 3
A longitudinal radiopaque marker was sutured to the polyester graft for orientation just below the fenestrated ostium using 6-0 Prolene sutures.

Fig. 4
The aortogram revealed right iliac dissection with intimal tears in the common iliac artery, which was limited to the proximal end of the external iliac artery at the left anterior oblique 40°+caudal 15° projection angle.

Fig. 5
The aortogram revealed that the iliac dissection successfully excluded and preserved the flow of the internal iliac artery. Arrows show the endoleak Ib (down) and IV (up).

References
1. Kwak HS, Han YM, Chung GH, Yu HC, Jeong YJ. Isolated spontaneous dissection of the common iliac artery: percutaneous stent placement in two patients. Cardiovasc Intervent Radiol. 2006; 29:883–885.
2. Farahmand P, Becquemin JP, Desgranges P, Allaire E, Marzelle J, Roudot-Thoraval F. Is hypogastric artery embolization during endovascular aortoiliac aneurysm repair (EVAR) innocuous and useful? Eur J Vasc Endovasc Surg. 2008; 35:429–435.
3. Parlani G, Verzini F, De Rango P, et al. Long-term results of iliac aneurysm repair with iliac branched endograft: a 5-year experience on 100 consecutive cases. Eur J Vasc Endovasc Surg. 2012; 43:287–292.
4. Oderich GS, Ricotta JJ 2nd. Novel surgeon-modified hypogastric branch stent graft to preserve pelvic perfusion. Ann Vasc Surg. 2010; 24:278–286.
5. Honjo O, Yamada Y, Kuroko Y, Kushida Y, Une D, Hioki K. Spontaneous dissection and rupture of common iliac artery in a patient with fibromuscular dysplasia: a case report and review of the literature on iliac artery dissections secondary to fibromuscular dysplasia. J Vasc Surg. 2004; 40:1032–1036.
6. Cook PS, Erdoes LS, Selzer PM, Rivera FJ, Palmaz JC. Dissection of the external iliac artery in highly trained athletes. J Vasc Surg. 1995; 22:173–177.
7. Kwon SH, Oh JH. Successful interventional treatment of a spontaneous right common iliac artery dissection extending retrogradely into the left external iliac artery. J Vasc Interv Radiol. 2006; 17:717–721.
8. Stone PA, Campbell JE, Hass SM, Jain A, Kazmi H. Kissing iliac artery stent technique for salvage of hypogastric artery occlusion secondary to iliac artery dissection during endovascular aneurysm repair. Vasc Endovascular Surg. 2011; 45:174–177.
9. Lee CW, Kaufman JA, Fan CM, et al. Clinical outcome of internal iliac artery occlusions during endovascular treatment of aortoiliac aneurysmal diseases. J Vasc Interv Radiol. 2000; 11:567–571.
10. Oderich GS, Ricotta JJ 2nd. Modified fenestrated stent grafts: device design, modifications, implantation, and current applications. Perspect Vasc Surg Endovasc Ther. 2009; 21:157–167.
11. Ricotta JJ 2nd, Tsilimparis N. Surgeon-modified fenestratedbranched stent grafts to treat emergently ruptured and symptomatic complex aortic aneurysms in high-risk patients. J Vasc Surg. 2012; 56:1535–1542.
12. Starnes BW. Physician-modified endovascular grafts for the treatment of elective, symptomatic, or ruptured juxtarenal aortic aneurysms. J Vasc Surg. 2012; 56:601–607.
13. Redlinger RE Jr, Ahanchi SS, Panneton JM. In situ laser fenestration during emergent thoracic endovascular aortic repair is an effective method for left subclavian artery revascularization. J Vasc Surg. 2013; 58:1171–1177.
14. Naughton PA, Park MS, Kheirelseid EA, et al. A comparative study of the bell-bottom technique vs hypogastric exclusion for the treatment of aneurysmal extension to the iliac bifurcation. J Vasc Surg. 2012; 55:956–962.
15. Lobato AC, Camacho-Lobato L. The sandwich technique to treat complex aortoiliac or isolated iliac aneurysms: results of midterm follow-up. J Vasc Surg. 2013; 57:2 Suppl. 26S–34S.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download