1. Julius S, Mejia A, Jones K, et al. "White coat" versus "sustained" borderline hypertension in Tecumseh, Michigan. Hypertension. 1990; 16:617–623.
2. Verdecchia P, Schillaci G, Boldrini F, Zampi I, Porcellati C. Variability between current definitions of 'normal' ambulatory blood pressure. Implications in the assessment of white coat hypertension. Hypertension. 1992; 20:555–562.
3. Bonow RO, Mann DL, Zipes DP, Libby P. Braunwald's Heart Disease. 9th ed. Philadelphia: Elsevier Health Sciences;2012. p. 218.
4. Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens. 2007; 25:2193–2198.
5. Ohkubo T, Kikuya M, Metoki H, et al. Prognosis of "masked" hypertension and "white-coat" hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol. 2005; 46:508–515.
6. Mancia G, Bombelli M, Brambilla G, et al. Long-term prognostic value of white coat hypertension: an insight from diagnostic use of both ambulatory and home blood pressure measurements. Hypertension. 2013; 62:168–174.
7. Glen SK, Elliott HL, Curzio JL, Lees KR, Reid JL. White-coat hypertension as a cause of cardiovascular dysfunction. Lancet. 1996; 348:654–657.
8. Mancia G, Facchetti R, Bombelli M, Grassi G, Sega R. Long-term risk of mortality associated with selective and combined elevation in office, home, and ambulatory blood pressure. Hypertension. 2006; 47:846–853.
9. Rothwell PM. Limitations of the usual blood-pressure hypothesis and importance of variability, instability, and episodic hypertension. Lancet. 2010; 375:938–948.
10. Pierdomenico SD, Di Nicola M, Esposito AL, et al. Prognostic value of different indices of blood pressure variability in hypertensive patients. Am J Hypertens. 2009; 22:842–847.
11. Rothwell PM, Howard SC, Dolan E, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet. 2010; 375:895–905.
12. Poortvliet RK, Ford I, Lloyd SM, et al. Blood pressure variability and cardiovascular risk in the PROspective Study of Pravastatin in the Elderly at Risk (PROSPER). PLoS One. 2012; 7:e52438.
13. Endo K, Kario K, Koga M, et al. Impact of early blood pressure variability on stroke outcomes after thrombolysis: the SAMURAI rt-PA Registry. Stroke. 2013; 44:816–818.
14. Schillaci G, Bilo G, Pucci G, et al. Relationship between short-term blood pressure variability and large-artery stiffness in human hypertension: findings from 2 large databases. Hypertension. 2012; 60:369–377.
15. Zakopoulos NA, Tsivgoulis G, Barlas G, et al. Impact of the time rate of blood pressure variation on left ventricular mass. J Hypertens. 2006; 24:2071–2077.
16. Franks PW. White-coat hypertension and risk of stroke: do the data really tell us what we need to know? Hypertension. 2005; 45:183–184.
17. Kang IS, Pyun WB, Shin J, Kim JH, Kim SG, Shin GJ. Association between central obesity and circadian parameters of blood pressure from the korean ambulatory blood pressure monitoring registry: Kor-ABP registry. J Korean Med Sci. 2013; 28:1461–1467.
18. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003; 42:1206–1252.
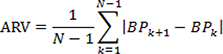
19. Mena L, Pintos S, Queipo NV, Aizpúrua JA, Maestre G, Sulbarán T. A reliable index for the prognostic significance of blood pressure variability. J Hypertens. 2005; 23:505–511.
20. Cacciolati C, Tzourio C, Hanon O. Blood pressure variability in elderly persons with white-coat and masked hypertension compared to those with normotension and sustained hypertension. Am J Hypertens. 2013; 26:367–372.
21. Myers MG. Pseudoresistant hypertension attributed to white-coat effect. Hypertension. 2012; 59:532–533.
22. Björklund K, Lind L, Vessby B, Andrén B, Lithell H. Different metabolic predictors of white-coat and sustained hypertension over a 20-year follow-up period: a population-based study of elderly men. Circulation. 2002; 106:63–68.
23. Sorof JM, Poffenbarger T, Franco K, Portman R. Evaluation of white coat hypertension in children: importance of the definitions of normal ambulatory blood pressure and the severity of casual hypertension. Am J Hypertens. 2001; 14(9 Pt 1):855–860.
24. Parati G, Di Rienzo M, Mancia G. Neural cardiovascular regulation and 24-hour blood pressure and heart rate variability. Ann N Y Acad Sci. 1996; 783:47–63.
25. Pickering TG. Variability of blood pressure. Blood Press Monit. 1998; 3:141–145.
26. Diaz KM, Veerabhadrappa P, Kashem MA, et al. Relationship of visit-to-visit and ambulatory blood pressure variability to vascular function in African Americans. Hypertens Res. 2012; 35:55–61.
27. Verdecchia P, Reboldi GP, Angeli F, et al. Short- and long-term incidence of stroke in white-coat hypertension. Hypertension. 2005; 45:203–208.
28. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013; 34:2159–2219.
29. Hong KS, Bang OY, Kang DW, et al. Stroke statistics in Korea: part I. Epidemiology and risk factors: a report from the korean stroke society and clinical research center for stroke. J Stroke. 2013; 15:2–20.
30. Mozaffarian D, Benjamin EJ, Go AS, et al. Executive summary: heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015; 131:434–441.









 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download