Abstract
Background and Objectives
Implantable cardioverter–defibrillators (ICDs) are indicated in patients with Brugada syndrome (BS), early repolarization syndrome (ERS), or idiopathic ventricular fibrillation (IVF) who are at high risk for sudden cardiac death. The optimal ICD programming for reducing inappropriate shocks in these patients remains to be determined. We investigated the difference in the mean cycle length of tachyarrhythmias that activated either appropriate or inappropriate ICD shocks in these three patient groups to determine the optimal ventricular fibrillation (VF) zone for minimizing inappropriate ICD shocks.
Subjects and Methods
We selected 41 patients (35 men) (mean age±standard deviation=42.6±13.0 year) who received ICD shocks between April 1996 and April 2014 to treat BS (n=24), ERS (n=9), or IVF (n=8). Clinical and ICD interrogation data were retrospectively collected and analyzed for all events with ICD shocks.
Results
Of the 244 episodes, 180 (73.8%) shocks were appropriate and 64 (26.2%) were inappropriate. The mean cycle lengths of the tachyarrhythmias that activated appropriate and inappropriate shocks were 178.9±28.7 ms and 284.8±24.4 ms, respectively (p<0.001). The cutoff value with the highest sensitivity and specificity for discriminating between appropriate and inappropriate shocks was 235 ms (sensitivity, 98.4%; specificity, 95.6%). When we programmed a single VF zone of ≤270 ms, inappropriate ICD shocks were reduced by 70.5% and appropriate shocks were missed in 1.7% of these patients.
Patients with Brugada syndrome (BS), with a typical electrocardiographic pattern of right bundle branch block and ST-segment elevation in the right precordial leads, are at high risk for sudden cardiac death.1) Early repolarization or a J-wave on the electrocardiogram (ECG) is associated with idiopathic ventricular fibrillation (IVF).2)3) Implantation of a cardioverter–defibrillator (ICD) is indicated in high-risk patients with BS, early repolarization syndrome (ERS), or IVF.4)5)
Inappropriate shocks due to atrial fibrillation occur in between 14% and 36% of patients with BS, according to long-term follow-up studies.6)7)8) ICD shocks negatively impact the quality of life and are associated with anxiety and depression, in addition to cardiac and cerebral ischemic injury.9)10)11)12) Although strategic programming of ICDs intended to reduce inappropriate shocks is associated with improved survival in patients with structural heart disease and left ventricular dysfunction,13)14) there are few data on the optimal programming required to reduce inappropriate shocks in patients with BS, ERS, or IVF.
The aim of the present study was to investigate the difference in the mean cycle length of tachyarrhythmias that activated appropriate and inappropriate ICD shocks in patients with BS, ERS, or IVF, and to suggest an optimal ventricular fibrillation (VF) zone to minimize inappropriate ICD shocks.
We retrospectively selected 41 patients with BS, ERS, or IVF who had received ICD shocks between April 1996 and April 2014 for primary or secondary prevention. All patients had completed a minimum follow-up of 6 months following the ICD implantation. The diagnosis of each arrhythmia syndrome was established according to the criteria of the Heart Rhythm Society/European Heart Rhythm Association/Asia Pacific Heart Rhythm Society expert consensus statement.15)
BS was diagnosed in patients who had one of two ECG morphologies in one or more of the right precordial leads (V1 or V2) positioned in the 2nd, 3rd, or 4th intercostal space: (1) type 1 ST-segment elevation of ≥2 mm, occurring either spontaneously or after a provocative drug test with the intravenous administration of Class I antiarrhythmic drugs; or (2) type 2 or type 3 ST-segment elevation when the same provocative drug test induced a type 1 ECG morphology.
ERS was diagnosed in the presence of a J-point elevation of ≥1 mm in two or more contiguous inferior and/or lateral leads of a standard 12-lead ECG in a patient resuscitated from otherwise unexplained VF/polymorphic ventricular tachycardia (VT).
IVF was defined as documented VF in a patient resuscitated from cardiac arrest for whom a thorough clinical evaluation had excluded known cardiac, respiratory, metabolic, and toxicologic etiologies and who had no signs of BS on ECG, with or without sodium-channel blocker provocation, ERS, and a normal Q–T interval.
In the 24 patients with BS, indications for ICD implantation included aborted cardiac arrest in 16 patients, syncope in 3 patients, and inducible VF in 5 patients. Seven patients with BS had a family history of sudden cardiac arrest. All patients with ERS or IVF had a history of aborted cardiac arrest due to VF. The choice between a single- and dual-chamber ICD implantation and selection of the device manufacturer were at the discretion of the attending physician.
All ICDs were programmed with a single VF detection zone, with a mean cutoff rate of 307.1±15.0 beats/minute (bpm), and with a maximum of six shocks at the maximal energy of the individual device. Back-up pacing was programmed to a rate of 40 bpm. In the ICDs from Medtronic (Minneapolis, Minnesota, USA), initial VF detection was set to 12 of 16 beats in 5 patients and 18 of 24 beats in 5 patients, with a redetection of 12/16 beats; in the ICDs from St. Jude Medical (Sylmar, California, USA), the initial VF detection was set to 12 beats, with a redetection of 12 beats.
A total of 244 episodes of ICD shock activations were reviewed by two independent cardiac electrophysiologists. Data were collected from routine device interrogations every 3 months and whenever ICD shocks occurred or an arrhythmic episode was suspected (i.e., syncope, palpitations, dyspnea, chest pain, and/or dizziness). The mean cycle length of the VF zone was calculated from the stored ventricular activation intervals for each episode that activated the ICD shock. Appropriate shocks were defined as shocks delivered for VT or VF, and inappropriate shocks were defined as those delivered in the absence of ventricular arrhythmias. The arrhythmia diagnosis was made according to a previous report.16)17) In brief, it was based on various characteristics, including the electrogram morphology, cycle length, regularity, abruptness of onset of the arrhythmia, mode of termination, and response to shock data, in conjunction with clinical information such as the symptoms. The study protocol was reviewed and approved by the institutional review board of the Asan Medical Center in Seoul, Korea.
All statistical analyses were performed with SPSS software version 18 (SPSS Inc., Chicago, IL, USA). Data are expressed as means±standard deviation or as number (%). Continuous variables were analyzed by the Student's t-test and the Mann–Whitney test. Categorical variables are presented as raw numbers and percentages and compared using the χ2 test. A p<0.05 was considered statistically significant. A receiver operating characteristic curve was used to determine the threshold for discriminating between appropriate and inappropriate shocks. The authors had full access to and take full responsibility for the integrity of the data. All authors have read and agree to the manuscript as written.
A total of 90 patients (79 men; 11 women) with BS, ERS, or IVF (39, 22, and 29 patients, respectively) had undergone ICD implantation at our center between April 1996 and April 2014. Of these patients, 41 patients (35 men) with BS, ERS, or IVF (24, 9, and 8 patients, respectively) who had received ICD shocks were included in the analysis. 11 patients had both appropriate and inappropriate ICD shocks. The baseline characteristics of the patients with ICD shocks are summarized in Table 1. The mean age of the patients at the time of implantation was 42.6±13.0 years. Single-chamber ICDs were implanted in 35 patients and dual-chamber ICDs in 6.
The median follow-up period was 101 months (interquartile range [IQR]=57.0-150.0). During that period, 29 patients received 180 appropriate ICD shocks in response to VF, polymorphic VT, or monomorphic VT (Fig. 1A). All ventricular tachyarrhythmias were correctly classified as VF and were successfully terminated by a single ICD shock. No patients experienced syncope or died during the follow-up period.
During a median follow-up period of 102.5 months (IQR=42.5-133.8), a total of 23 patients (20 men) (mean age=44.6±12.7 years) received 64 inappropriate ICD shocks in response to supraventricular tachyarrhythmias (SVAs) (59 episodes) (Fig. 1B), noise oversensing (4 episodes), and T-wave oversensing (1 episode). There were 42 inappropriate shocks due to SVAs in patients with single-chamber ICDs and 17 inappropriate shocks due to SVAs in patients with dual-chamber ICDs. All inappropriate shocks due to oversensing occurred in patients with single-chamber ICDs (Table 2). There were two or more inappropriate shocks in 11 patients. SVA was the cause of multiple inappropriate shocks in 10 patients, and noise oversensing was the cause of multiple inappropriate shocks in 1 patient.
The mean cycle length of tachyarrhythmias that activated inappropriate ICD shocks was longer than that for appropriate shocks (284.8±24.4 vs. 178.9±28.7 ms, respectively; p<0.001) (Figs. 2 and 3). Although the mean cycle length of the tachyarrhythmias that activated inappropriate shocks was significantly lower in the IVF patients, there was no significant difference in the mean cycle lengths of tachyarrhythmias that activated appropriate shocks among the BS, ERS, and IVF patients (Table 3). The best discriminating cutoff value with the highest sensitivity and specificity was 235 ms (Fig. 4); however, the application of this cutoff value caused 8 appropriate shocks (4.4%) to be missed. Application of a single VF zone of 250, 260, or 270 ms in all these patients reduced the inappropriate shocks by 91.8%, 82.0%, and 70.5%, respectively, whereas delayed or missed appropriate shocks occurred in 2.8%, 2.8%, and 1.7%, respectively. Application of a single VF zone of 250, 260, or 270 ms in the BS patients reduced inappropriate shocks by 94.1%, 88.2%, and 82.4%, respectively, whereas delayed or missed appropriate shocks occurred in 4.3%, 4.3%, and 3.2%, respectively. In patients with ERS and IVF, a single VF zone of 250, 260, or 270 ms reduced inappropriate shocks by 90.9%, 79.5%, and 65.9%, respectively, whereas delayed or missed appropriate shocks occurred in 1.1%, 1.1%, and 0%, respectively.
This analysis indicates that (1) the cycle length of tachyarrhythmias that activated appropriate ICD shocks was significantly shorter than that of inappropriate shocks; (2) a VF zone as short as 240 ms could virtually eliminate the possibility of inappropriate shocks; and (3) the VF zone should be optimized to reduce inappropriate shocks in patients with BS, ERS, or IVF while guaranteeing their safety.
Despite the overall success of ICDs in preventing death, inappropriate shocks are common in these high-risk patients without structural heart disease.6)7) Causes of inappropriate shocks in patients with BS include atrial tachyarrhythmias, sinus tachycardia, T-wave oversensing, and lead malfunction.6)8) However, no study has investigated the incidence of inappropriate shocks in patients with ERS or IVF. In the present study, inappropriate shocks in these patients occurred in 27.2% and 18.5%, respectively, which was similar to the rate in the patients with BS (30.8%). Inappropriate shocks negatively impact the quality of life of young patients with ICDs,18)19) as well as of patients with structural heart disease who have ICDs.9)10) A reduction in inappropriate shocks can be accomplished by (1) antitachycardia pacing;20) (2) ICD programming for tachyarrhythmias of 200 bpm or higher or with a prolonged delay in shocking at 170 bpm or higher;14) and (3) prolonged detection (30 of 40 intervals), allowing a delay in arrhythmia detection.13) Antitachycardia pacing cannot be applied in patients with BS, ERS, or IVF because most spontaneous ventricular arrhythmia episodes that trigger ICD shocks are VF and polymorphic VT, not monomorphic VT.8) Further studies are required to determine whether a shock delay can reduce inappropriate shocks without increasing the risk of syncope in the specific population with BS, IRS, or IVF. One strategy for reducing inappropriate shocks is to program a single high-rate VF zone (detection of tachyarrhythmia of 222 bpm or higher).21)
To the best of our knowledge, this is the first study to compare the mean cycle length of tachyarrhythmias that cause appropriate and inappropriate shocks. A mean VF cycle length (VFCL) calculated from stored ventricular activation intervals during VF is the simplest way to quantify and detect the patterns or order of VF waveforms.22)23)24) The mean VFCL is reproducible among different VF episodes in individual patients.24) In our present study, the mean VFCL of 178.9±28.7 ms was similar to the average cycle length of induced VF of 184±17 ms.25) In addition, the mean cycle length of the tachyarrhythmias that activated inappropriate shocks was 284.8±24.4 ms, which was significantly longer than the mean VFCL. In addition, 8.2% of episodes of inappropriate shocks had cycle lengths of <250 ms. In previous studies, the mean ventricular cycle length during atrial flutter with 1:1 atrioventricular (AV) conduction was between 265 ms and 292 ms.26)27) Enhanced AV nodal conduction in this young population, together with a short, heightened sympathetic tone that leads to shortening of the atrial flutter cycle length might have contributed to the very short cycle length of the SVAs. In our patient population, two patients with BS had three VT episodes with a cycle length of 282.0±11.7 ms, which activated ICD shocks. Although monomorphic VT rarely occurred in the patients with BS, programming of a single VF zone of ≤240 ms can miss VT episodes, which may cause serious symptoms, including syncope. No patients with ERS or IVF had VT episodes during the follow-up period, suggesting that the use of a single VF zone of 240 ms as an initial programmed cutoff can prevent inappropriate shocks. In our study, 55.6% of the patients with ERS had inappropriate shocks due to atrial fibrillation. The potassium inwardly rectifying channel variant (KCNJ8 mutation) is associated with early repolarization and atrial fibrillation.28) However, none of our patients underwent gene analysis.
First, our present study had limitations inherent in a retrospective analysis of electrograms stored in ICDs from a single tertiary center. However, our study still constituted the largest analysis to date of stored ICD electrograms of appropriate and inappropriate shocks in patients without structural heart disease across BS, ERS, or IVF. Second, some of the ICD programming is out of date in view of current ICD programming standards. However, this real-world practice data sheds light on the importance of optimal VF zone programming in reducing inappropriate shocks and ensuring patient safety. Third, the manufacturer and mode of ICD programming were not uniform, which also reflects differences in shock delays. Further study of an ICD population without structural heart disease is required to determine whether a delay in VF shocks can increase the detection of nonsustained VF/polymorphic VT, thereby avoiding unnecessary shocks. Fourth, because we did not include patients with short or long Q–T syndrome or catecholaminergic polymorphic VT, ICD programming in this patient group might differ from the suggested optimal programming in patients with BS, ERS, or IVF. Fifth, we did not measure the induced VFCL at the time of ICD implantation, which might be useful for tailoring the VF zone to individual patients. Sixth, we did not analyze the medications. Although medications would affect the VFCL, we could not evaluate the association between the VFCL and these patients' medications because of the limitations of the retrospective study.
In patients with BS, ERS, or IVF, the mean cycle length of the VF zone is significantly shorter for appropriate shocks than for inappropriate shocks. Programming a single VF zone (≤270 ms in patients with BS or as low as ≤250 ms in patients with ERS or IVF) might be one method to reduce inappropriate shocks in these patients. Further randomized clinical trials that compare the effect of ICD programming settings on the frequency of inappropriate shocks in patients with BS, ERS, or IVF are warranted.
Figures and Tables
Fig. 1
Representative electrograms of the episodes obtained upon device interrogation. (A) Appropriate ICD shock due to VF, (B) inappropriate ICD shock due to atrial fibrillation with rapid ventricular response. ICD: implantable cardioverter-defibrillator, VF: ventricular fibrillation, AMP: amplitude, HV: high voltage shock, AS: atrial sensing, STIM: stimulation (antitachycardia pacing).

Fig. 2
Distribution of the tachyarrhythmia cycle lengths of appropriate or inappropriate ICD shocks. ICD: implantable cardioverter-defibrillator.
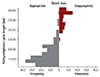
Fig. 3
Mean cycle lengths of the tachyarrhythmias causing appropriate or inappropriate ICD shocks in all patients. ICD: implantable cardioverter-defibrillator.

Fig. 4
Best cutoff value for discriminating between appropriate and inappropriate ICD shocks (235 ms; sensitivity: 98.4%, specificity: 95.6%). ICD: implantable cardioverter-defibrillator
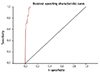
Table 1
Baseline characteristics of patients with ICDs
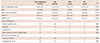
Table 2
Causes of inappropriate ICD shocks

Table 3
Mean cycle length of tachyarrhythmias causing appropriate or inappropriate shocks in all study patients and by diagnosis

|
Total (n=41) |
BS (n=24) |
ERS (n=9) |
IVF (n=8) |
|
|---|---|---|---|---|
| Appropriate shock (ms) | 178.9±28.7* | 178.4±30.4† | 181.1±29.0† | 176.1±22.5† |
| Inappropriate shock (ms) | 284.8±24.4* | 291.5±20.1‡ | 292.6±22.3‡ | 274.8±25.0‡ |
Acknowledgments
The authors thank Mr. John Martin for his linguistic assistance with this manuscript.
References
1. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992; 20:1391–1396.
2. Haïssaguerre M, Derval N, Sacher F, et al. Sudden cardiac arrest associated with early repolarization. N Engl J Med. 2008; 358:2016–2023.
3. Nam GB, Kim YH, Antzelevitch C. Augmentation of J waves and electrical storms in patients with early repolarization. N Engl J Med. 2008; 358:2078–2079.
4. Brugada J, Brugada R, Antzelevitch C, Towbin J, Nademanee K, Brugada P. Long-term follow-up of individuals with the electrocardiographic pattern of right bundle-branch block and ST-segment elevation in precordial leads V1 to V3. Circulation. 2002; 105:73–78.
5. Haïssaguerre M, Sacher F, Nogami A, et al. Characteristics of recurrent ventricular fibrillation associated with inferolateral early repolarization role of drug therapy. J Am Coll Cardiol. 2009; 53:612–619.
6. Bordachar P, Reuter S, Garrigue S, et al. Incidence, clinical implications and prognosis of atrial arrhythmias in Brugada syndrome. Eur Heart J. 2004; 25:879–884.
7. Sarkozy A, Boussy T, Kourgiannides G, et al. Long-term follow-up of primary prophylactic implantable cardioverter-defibrillator therapy in Brugada syndrome. Eur Heart J. 2007; 28:334–344.
8. Sacher F, Probst V, Maury P, et al. Outcome after implantation of a cardioverter-defibrillator in patients with Brugada syndrome: a multicenter study-part 2. Circulation. 2013; 128:1739–1747.
9. Schron EB, Exner DV, Yao Q, et al. Quality of life in the antiarrhythmics versus implantable defibrillators trial: impact of therapy and influence of adverse symptoms and defibrillator shocks. Circulation. 2002; 105:589–594.
10. Kamphuis HC, de Leeuw JR, Derksen R, Hauer RN, Winnubst JA. Implantable cardioverter defibrillator recipients: quality of life in recipients with and without ICD shock delivery: a prospective study. Europace. 2003; 5:381–389.
11. Xie J, Weil MH, Sun S, et al. High-energy defibrillation increases the severity of postresuscitation myocardial dysfunction. Circulation. 1997; 96:683–688.
12. de Vries JW, Bakker PF, Visser GH, Diephuis JC, van Huffelen AC. Changes in cerebral oxygen uptake and cerebral electrical activity during defibrillation threshold testing. Anesth Analg. 1998; 87:16–20.
13. Gasparini M, Proclemer A, Klersy C, et al. Effect of long-detection interval vs standard-detection interval for implantable cardioverter-defibrillators on antitachycardia pacing and shock delivery: the ADVANCE III randomized clinical trial. JAMA. 2013; 309:1903–1911.
14. Moss AJ, Schuger C, Beck CA, et al. Reduction in inappropriate therapy and mortality through ICD programming. N Engl J Med. 2012; 367:2275–2283.
15. Priori SG, Wilde AA, Horie M, et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013; 10:1932–1963.
16. Klein RC, Raitt MH, Wilkoff BL, et al. Analysis of implantable cardioverter defibrillator therapy in the Antiarrhythmics Versus Implantable Defibrillators (AVID) Trial. J Cardiovasc Electrophysiol. 2003; 14:940–948.
17. Raitt MH, Dolack GL, Kudenchuk PJ, Poole JE, Bardy GH. Ventricular arrhythmias detected after transvenous defibrillator implantation in patients with a clinical history of only ventricular fibrillation. Implications for use of implantable defibrillator. Circulation. 1995; 91:1996–2001.
18. Cook SC, Valente AM, Maul TM, et al. Shock-related anxiety and sexual function in adults with congenital heart disease and implantable cardioverter-defibrillators. Heart Rhythm. 2013; 10:805–810.
19. Dubin AM, Batsford WP, Lewis RJ, Rosenfeld LE. Quality-of-life in patients receiving implantable cardioverter defibrillators at or before age 40. Pacing Clin Electrophysiol. 1996; 19(11 Pt 1):1555–1559.
20. Wathen MS, DeGroot PJ, Sweeney MO, et al. Prospective randomized multicenter trial of empirical antitachycardia pacing versus shocks for spontaneous rapid ventricular tachycardia in patients with implantable cardioverter-defibrillators: Pacing Fast Ventricular Tachycardia Reduces Shock Therapies (PainFREE Rx II) trial results. Circulation. 2004; 110:2591–2596.
21. Veltmann C, Kuschyk J, Schimpf R, et al. Prevention of inappropriate ICD shocks in patients with Brugada syndrome. Clin Res Cardiol. 2010; 99:37–44.
22. Yokoshiki H, Kohya T, Sato M, et al. Increased cycle length variability during ventricular fibrillation: a novel predictor of arrhythmia recurrence. J Electrocardiol. 2003; 36:137–146.
23. Lever NA, Newall EG, Larsen PD. Differences in the characteristics of induced and spontaneous episodes of ventricular fibrillation. Europace. 2007; 9:1054–1058.
24. Li H, Easley A, Windle J, Samoil D, Barrington W. The mean ventricular fibrillation cycle length: a potentially useful parameter for programming implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 1998; 21:1789–1794.
25. Watanabe H, Chinushi M, Sugiura H, et al. Unsuccessful internal defibrillation in Brugada syndrome: focus on refractoriness and ventricular fibrillation cycle length. J Cardiovasc Electrophysiol. 2005; 16:262–266.
26. Turitto G, Akhrass P, Leonardi M, Saponieri C, Sette A, El-Sherif N. Atrial flutter with spontaneous 1:1 atrioventricular conduction in adults: an uncommon but frequently missed cause for syncope/presyncope. Pacing Clin Electrophysiol. 2009; 32:82–90.
27. Kawabata M, Hirao K, Higuchi K, et al. Clinical and electrophysiological characteristics of patients having atrial flutter with 1:1 atrioventricular conduction. Europace. 2008; 10:284–288.
28. Delaney JT, Muhammad R, Blair MA, et al. A KCNJ8 mutation associated with early repolarization and atrial fibrillation. Europace. 2012; 14:1428–1432.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download