This article has been corrected. See "Erratum: Psychiatric Characteristics of the Cardiac Outpatients with Chest Pain" in Volume 46 on page 432.
Abstract
Background and Objectives
A cardiologist's evaluation of psychiatric symptoms in patients with chest pain is rare. This study aimed to determine the psychiatric characteristics of patients with and without coronary artery disease (CAD) and explore their relationship with the intensity of chest pain.
Subjects and Methods
Out of 139 consecutive patients referred to the cardiology outpatient department, 31 with atypical chest pain (heartburn, acid regurgitation, dyspnea, and palpitation) were excluded and 108 were enrolled for the present study. The enrolled patients underwent complete numerical rating scale of chest pain and the symptom checklist for minor psychiatric disorders at the time of first outpatient visit. The non-CAD group consisted of patients with a normal stress test, coronary computed tomography angiogram, or coronary angiogram, and the CAD group included those with an abnormal coronary angiogram.
Results
Nineteen patients (17.6%) were diagnosed with CAD. No differences in the psychiatric characteristics were observed between the groups. "Feeling tense", "self-reproach", and "trouble falling asleep" were more frequently observed in the non-CAD (p=0.007; p=0.046; p=0.044) group. In a multiple linear regression analysis with a stepwise selection, somatization without chest pain in the non-CAD group and hypochondriasis in the CAD group were linearly associated with the intensity of chest pain (β=0.108, R2=0.092, p=0.004; β= -0.525, R2=0.290, p=0.010).
One of the most common complaints of patient in the cardiology outpatient department is chest pain. The difficulty in differentiating chest pain caused by cardiac and non-cardiac factors has long been recognized. More than half of the patients referred for coronary angiography (CAG) suffer chest pain that is not of cardiac origin.1) Hoffman and colleagues found that of 103 patients with acute chest pain, 14 (13.6%) had acute coronary syndrome (ACS), assessed by coronary computed tomography angiography (CCTA).2) Many patients with chest pain do not receive a medical explanation for their pain.3) Non-cardiogenic chest pain is associated with impaired psychiatric functioning and reduced quality of life.4) Studies have found that patients with non-cardiogenic chest pain had significantly more symptoms of depression and anxiety than those with cardiogenic chest pain.5)6) In contrast, other studies have reported no differences in psychiatric characteristics for patients with or without coronary artery disease (CAD).7)8)9)
If the causes of chest pain are obvious and include non-psychiatric factors, the condition can be treated based on recent advances in diagnostic tools, medications, interventions, and surgery. However, if the causes of chest pain are psychiatric in nature, cardiologists will not be able to alleviate the patients' chief complaints.4)
In many previous studies, the effect and necessity of psychiatric intervention or medications have been demonstrated in patients with chest pain with or without CAD.9)10)11)12)13)14) However, the psychiatric evaluation of patients with chest pain by a cardiologist is very rare in Korea. Therefore, the purposes of this study are to 1) determine the psychiatric characteristics of patients with and without CAD, and 2) explore the relationship between the intensity of chest pain and psychiatric characteristics, assessed by cardiologists, in the cardiology outpatient department in Korea. This study also examined the method used to differentiate between cardiogenic and non-cardiogenic chest pain.
This prospective cohort study was approved by the ethical committee of the institutional review board of Jeju National University Hospital, and the need for written informed consent was waived owing to the non-interventional nature of the study.
Between May and December 2012, 139 consecutive patients from Jeju, a rural area of Korea, were referred to the cardiology outpatient department based on their complaint of chest pain. Patients whose atypical chest pain included conditions of heartburn, acid regurgitation, dyspnea, and palpitation were excluded in the study. Consequently, 31 patients were excluded due to conditions of pneumonia (n=2), atrial fibrillation (n=11), heart failure (n=7), and improved symptoms after using proton pump inhibitors (n=11). Ultimately, 108 patients were enrolled in the study.
The patients were divided into two groups according to their probability of ACS (unstable angina and non ST-elevation myocardial infarction), as determined by the cardiologists. Group 1 consisted of patients, who were at a low probability for having ACS and Group 2 consisted of patients, who were at a high probability for having ACS. Patients had a high probability of ACS when they demonstrated: (1) chest pain at rest (or with minimal exertion), usually lasting >10 minutes; (2) severe chest pain (within the prior 4–6 weeks); and/or (3) a crescendo pattern (distinctly more severe, prolonged, or frequent).15)
Group 1 underwent a treadmill test (TMT), single-photon emission computed tomography (SPECT), or CCTA. Subsequently, CAG was performed for the patients who displayed abnormal results, whereas Group 2 received CAG directly.
For the TMT, an abnormal result was defined as the presence of chest pain, electrocardiographic (ECG) changes, or both. A normal TMT involved no chest pain and no ECG changes. Patients with a normal TMT were not diagnosed with CAD. On SPECT, a reduced tracer uptake in a myocardial region on the resting and/or stress images was defined as abnormal. On CCTA, significant stenosis was defined as the presence of luminal narrowing of a >50% diameter reduction in the cross-sectional images. Patients with a normal CCTA were defined as having non-cardiogenic chest pain.
All CAG assessments were performed while the patient was in a fasting condition. Patients provided informed consent before the CAG procedure. Normal saline was administered intravenously before CAG to provide renal protection and to prepare for any potential emergency. Quantitative coronary angiographic analysis was performed using standard techniques and automated edge-detection algorithms (ANCOR V2.0, Siemens, Munich, Germany). If diagnostic CAG failed to reveal significant stenosis (>50% diameter stenosis, based on quantitative angiographic analysis), increasing doses of intravenous ergonovine (100 and 200 µg) were administered every 2 min until coronary artery spasms were provoked; a standard, 12-lead ECG was monitored. Variant angina was defined as chest pain and ECG evidence of myocardial ischemia and/or severe transient coronary stenosis.
The patients provided responses to the numerical rating scale (NRS) of pain (0-10) and the symptom checklist for minor psychiatric disorders (SCL-MPD) questionnaires at the time of first outpatient visit. The SCL-MPD is a Korean questionnaire used to evaluate psychiatric symptoms consisting of 10 dimensions with 67 items. The dimensions measuring paranoia and psychosis were removed in the SCL-90, and hypochondriasis and neurasthenia were added instead. It has been proven to be reliable and valid method of evaluating psychiatric symptoms (total score, 0.980, 0.001).16) There are 5 responses to assess the severity of symptoms for each item: "not at all" (0), "few" (1), "usually" (2), "quite severe" (3) and "very severe" (4). The score for each dimension represents the sum of the scores for the items within that dimension. Patients who were illiterate completed the questionnaires with the help of a research assistant. The total score of the SCL-MPD was converted to a T-score. An abnormal tendency was defined as a T score greater than 60 points.
Statistical analyses were performed using SPSS 17.0 software (SPSS, Chicago, IL, USA). Data are presented as the mean±standard deviation or the median and interquartile range for continuous variables or as frequencies for categorical variables. The goal sample size of 130 subjects with chest pain was determined using the single proportion method with the following values: the proportion of patients with cardiogenic chest pain in a previous study2) was 13.6%; the hypothesis value, 5%; significance level, 0.05; power, 80%; and dropout rate, 20%. Comparisons between the two groups were made using the Wilcoxon two-sample test (or the Mann-Whitney test) for continuous variables and the chi-squared test for categorical variables. Spearman correlation analysis was used to evaluate the correlation between the intensity of chest pain and psychiatric variables. Figure 2 was based on Pearson correlation coefficient. Analysis of covariance (ANCOVA) was also performed to compare the associations between chest pain and psychiatric parameters for the CAD and non-CAD groups (adjusting for age, hypertension, previous ischemic heart disease, and hyperlipidemia). A multiple linear regression analysis with stepwise selection was performed to identify the variables that were independently related to the intensity of chest pain. These were based on an initial full model; p≤0.05 was considered significant.
In total, 70 patients (64.8%) underwent a TMT, 14 (12.9%) underwent CCTA, and 37 (34.3%) underwent CAG. Of all patients, 19 (17.6%) were diagnosed with CAD. The clinical diagnoses included stable angina (n=7 [6.5%]; Group 1, n=3 [2.8%]; Group 2, n=4 [3.7%]), variant angina (n=4 [3.7%]; Group 1, n=1 [0.9%]; Group 2, n=3 [2.8%], and ACS (n=8 [7.4%]). Revascularization was performed in 10 patients (9.3%; Group 1, n=2 [1.9%]; Group 2, n=8 [7.4%]). Medications for stable and variant angina were administered to 9 patients (8.3%, Table 1). Fig. 1 shows the flow diagram used to differentiate between the CAD and non-CAD groups upon admission to the cardiology outpatient department.
The mean age was significantly higher in the CAD group 63.3±8.4 years vs. 47.8±15.1 years, p<0.001). Hypertension (63.2% vs. 21.3%, p<0.001), hyperlipidemia (26.3% vs. 7.9%, p<0.035), and previous ischemic heart disease (36.8% vs. 6.7%, p<0.001) were more frequently noted in the CAD group than in the non-CAD group (Table 2).
The items that received the highest scores and most frequent responses for all patients were, in order, "over-concern about your health" (item 16, hypochondriasis, 2 [1-3], 91%), "over-concern about unusual body signs or sensations" (item 24, hypochondriasis, 2 [1-3], 90%), easily mentally fatigued" (item 8, neurasthenia, 2 [1-3], 84%), and "worrying too much" (item 23, depression, 2 [1-3], 81%). In the non-CAD group, these items were "over-concern about your health" (item 16, hypochondriasis, 2 [1-3], 94%), "worrying too much" (item 23, depression, 2 [1-2], 87%), "over-concern about unusual body signs or sensations" (item 24, hypochondriasis, 2 [1-2], 84%), and "easily mentally fatigued" (item 8, neurasthenia, 2 [1-3], 83%). In the CAD group, these items were "easily mentally fatigued" (item 8, neurasthenia, 2 [1-3], 84%), "over-concern about unusual body signs or sensations" (item 24, hypochondriasis, 2 [1-3], 84%), "awakening in the morning" (item 49, general, 1 [1-3], 84%), and "sleep that is restless or disturbed" (item 51, general, 2 [1-3], 79%).
The median values for each subsection of the SCL-MPD for the CAD and non-CAD groups are presented in Tables 3-1 and 3-2. The differences in the dimension scores, total score, and T score were not statistically significant. The proportions of patients with a high T score (≥60) were not different between the groups (19.1% vs. 15.8%, p=0.736). Furthermore, no differences were observed in the psychiatric factors between the CAD and non-CAD groups before or after adjusting for age, hypertension, previous ischemic heart disease, and hyperlipidemia. However, "feeling tense" (item 44, anxiety), "self-reproach for things" (item 20, depression), and "trouble falling asleep" (item 30, general) were more frequently observed in the non-CAD group (1 [0-2] vs. 0 [0-1], p=0.007; 1 [0-2] vs. 0 [0-1], p=0.046; 1 [0-3] vs. 0 [0-2], p=0.044; Table 3-1 an, 3-2).
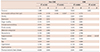
Statistically significant correlations between the intensity of chest pain and psychiatric symptom dimensions were observed in the non-CAD group (somatization, rho=0.336, p=0.001; somatization without chest pain, rho=0.294, p=0.005; anxiety, rho=0.229, p=0.031; and hypochondriasis, rho=0.225, p=0.034). Statistically significant inverse correlations between the intensity of chest pain and psychological symptom dimensions were observed in the CAD group (depression, rho=-0.503, p=0.028; hypochondriasis, rho= -0.647, p=0.003; general, rho=-0.584, p=0.009, Table 4 an, Fige 2).
In a multiple linear regression analysis with a stepwise selection, the score for somatization without chest pain in the non-CAD group and hypochondriasis in the CAD group were associated with the intensity of chest pain (β=0.108, R2=0.092, p=0.004; β=-0.525, R2=0.329, p=0.010, Table 5).
The present study observed (1) no differences in psychological characteristics between the groups with and without CAD, though some psychiatric items were different between the groups; (2) a correlation between the intensity of chest pain and somatization without chest pain in the non-CAD group; and (3) an inverse correlation between the intensity of chest pain and hypochondriasis in the CAD group. This study also illustrates the method used by cardiologists to differentiate between cardiogenic and non-cardiogenic chest pain.
It is difficult to differentiate chest pain with cardiac versus non-cardiac causes. However, this study had a standard method for diagnosing cardiogenic chest pain and did not limit the test method to conform to other standards. Therefore, cardiogenic chest pain was defined by (1) abnormality in a non-invasive test (TMT, SPECT) and CAG or (2) abnormality on CAG. According to an earlier cohort study of acute chest pain and CCTA, a small number of patients (only 13.5%) were reported to have ACS.2) We also found a small proportion of patients with chest pain diagnosed as CAD in the outpatient department.
The SCL-MPD is a simplified version of the SCL-90 questionnaire that contains 67 items. The paranoia and psychosis categories were removed from the SCL-90, and hypochondriasis and neurasthenia were added to the SCL-MPD. As per previous studies, it is evident that paranoia and psychosis are rare and hypochondriasis and neurasthenia are common in patients with chest pain, the SCL-MPD was found to be more appropriate for this study.5)6)17)18)
Several studies have reported that scores on tests of panic phobia, somatization, neurasthenia, anxiety, and depression were higher in patients with non-cardiogenic chest pain than patients with cardiogenic chest pain.5)6)17)18) In contrast, other studies have reported that psychiatric characteristics did not differ in patients with or without CAD.7)8)9) In this study, some psychiatric symptom dimensions tended to differ between the CAD and non-CAD groups. Furthermore, some specific items ("feeling tense", "self-reproach for things" and "trouble falling asleep") were significantly different between the groups. However, the differences in the dimension scores were not statistically significant. According to a previous study, the lack of difference in psychiatric characteristics between CAD and non-CAD groups could be due to the high psychiatric morbidities in both the groups as the source of chest pain.7) According to other previous studies, the chest pain is established as the source of psychiatric morbidities in both the groups.8)19) In this study, high psychiatric morbidities (hypochondriasis, neurasthenia, and depression) were also present, as evidenced by high frequency SCL-MPD items. In addition, the proportion of patients with a high SCL-MPD T score (≥60) did not differ between the groups.
Some risk factors in this study (old age, hypertension, and hyperlipidemia) differed between the CAD and non-CAD groups. A number of studies on psychiatric factors and CAD have not considered the importance of the risk factors.4)5)6)7)8)9)10)17)18)19)20)21)22) Psychosocial factors such as depression, anxiety, hostility, social isolation, and life stress are associated with cardiovascular risk factors.20) For instance, hypertension is related to anxiety,21)22) and the association of metabolic syndrome with depression has been well documented.23) These relationships have been explained based on sympathetic nervous system hyperresponsivity, hypercortisolism, and unhealthy lifestyle behaviors.20)21)22)23)24) Older populations have less psychological disorders,25) and old age is considered as an important cardiovascular risk factor.26) Therefore, cardiovascular risk factors should be considered in the studies dealing with psychiatric factors and CAD. No differences were observed in the psychiatric factors between the CAD and non-CAD groups before or after adjusting for age, hypertension, previous ischemic heart disease, and hyperlipidemia in this study.
In some studies, patients who have experienced chest pain with or without CAD had a higher sensitivity to pain and more severe pain than healthy groups.8) In addition, the degree of anxiety was linearly associated with the intensity of pain in sensitive patients.27) In this study, linear association between the intensity of chest pain and psychiatric characteristics (somatization without chest pain, anxiety, and hypochondriasis) was observed in the non-CAD group. An inversely linear association between psychiatric characteristics (depression, hypochondriasis, and general) and the intensity of chest pain was observed in the CAD group. Finally, somatization without chest pain in the non-CAD group and hypochondriasis in the CAD group had the greatest effect on the intensity of chest pain among the psychiatric characteristics. The cause of the inverse correlation between hypochondriasis and chest pain score in the CAD group might be explained by the fact that hypochondriacs usually have many other symptoms to worry about, so chest pain itself might be a relatively minor concern to them. Additionally, the pain typically occurs only during exertion, not during low-intensity or everyday activities.
Patients with non-cardiogenic chest pain are at a lower risk of death. However, they experience continuing chest pain, limitation of activities, concerns about the cause of their symptoms, and dissatisfaction with medical care1)4) and they have high psychiatric morbidities.4)5)6)7)8)9)10)17)18)19)20) Interestingly, gastroesophageal reflux disease, a major cause of non-cardiogenic chest pain, has a high psychiatric morbidity.28) Patients with cardiogenic chest pain also had high psychiatric morbidities.10)19) Because they are related to cardiovascular risk factors and medication non-adherence,20)29) psychiatric morbidities are also predictors of mortality in patients with CAD.30) Therefore, psychiatric intervention or medications were necessary and effective in both the groups.10)11)12)13)14)
This study has several limitations. The prime one is the small sample size and inclusion of multiple psychiatric items. In a study of CCTA and ACS,2) ACS was present in 13.6% of patients in the emergency department. We set the hypothesis value of our study low (5%), because we recruited patients from the outpatient department. Despite this, 19 patients (17.6%) were diagnosed with CAD. Hence, a well-designed larger cohort study is needed to confirm these results and expand upon this limitation. Second, the patients were limited to cardiac outpatients, because it is more difficult for patients in the emergency room to fill out questionnaires. However, patients with chest pain in the emergency room may be different from those in the outpatient department. Finally, the use of a more typical diagnostic standard may help us discover less obvious origins of chest pain than the current design. For instance, intermediate stenosis (50-75%) was also defined as CAD in the direct CAG group. In these cases, the cause of chest pain may not be CAD. Additionally, we cannot rule out variant angina in cases with a normal CCTA. However, the selection of the initial test for CAD, either TMT, SPECT, CCTA, or CAG, was made by the cardiologists. Thus, all patients underwent an initial test similar to the typical practice in the cardiology outpatient department.
No differences in the overall psychiatric characteristics were observed between the groups with and without CAD. However, some psychiatric items were more frequently observed in the non-CAD group. The intensity of chest pain was linearly associated with the score of somatization without chest pain in the non-CAD group and inversely linearly associated with hypochondriasis in the CAD group. In summary, patients with more intense chest pain had more additional discomfort in the non-CAD group, and less health concerns in the CAD group.
Figures and Tables
 | Fig. 1The flow diagram used to differentiate between the CAD and non-CAD groups from the point of admission to the cardiology outpatient department. CAD: coronary artery disease, CAG: coronary angiography, CCTA: coronary artery computed tomography angiography, SPECT: single-photon emission computed tomography, TMT: treadmill test. |
 | Fig. 2The relationships between the intensity of chest pain and psychological symptom dimensions. Somatization without chest pain in the non CAD group (A). Hypochondriasis in the CAD group (B). CAD, coronary artery disease. |
Table 1
Clinical baseline characteristics of thespatients

Table 2
Comparison of the clinical baseline characteristics between groups with and without coronary artery disease
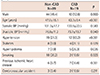
Table 3-1
Comparisons of the dimensions and symptoms between groups with and without coronary artery disease

Table 3-2
Comparison of the dimensions and symptoms between groups with and without coronary artery disease

Table 4
Analysis of the correlation between the intensity of chest pain and psychiatric symptom dimensions
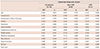
Table 5
Multiple linear regression analysis of psychiatric characteristics according to the intensity of chest pain
Acknowledgments
This study was supported by a research grant from the Jeju National University Hospital (2012-21).
References
1. Papanicolaou MN, Califf RM, Hlatky MA, et al. Prognostic implications of angiographically normal and insignificantly narrowed coronary arteries. Am J Cardiol. 1986; 58:1181–1187.
2. Hoffmann U, Nagurney JT, Moselewski F, et al. Coronary multidetector computed tomography in the assessment of patients with acute chest pain. Circulation. 2006; 114:2251–2260.
3. Kroenke K, Mangelsdorff AD. Common symptoms in ambulatory care: incidence, evaluation, therapy, and outcome. Am J Med. 1989; 86:262–266.
4. Mayou R, Bryant B, Forfar C, Clark D. Non-cardiac chest pain and benign palpitations in the cardiac clinic. Br Heart J. 1994; 72:548–553.
5. Channer KS, Papouchado M, James MA, Rees JR. Anxiety and depression in patients with chest pain referred for exercise testing. Lancet. 1985; 2:820–823.
6. Cormier LE, Katon W, Russo J, Hollifield M, Hall ML, Vitaliano PP. Chest pain with negative cardiac diagnostic studies. Relationship to psychiatric illness. J Nerv Ment Dis. 1988; 176:351–358.
7. Dammen T, Arnesen H, Ekeberg O, Friis S. Psychological factors, pain attribution and medical morbidity in chest-pain patients with and without coronary artery disease. Gen Hosp Psychiatry. 2004; 26:463–469.
8. Zachariae R, Melchiorsen H, Frøbert O, Bjerring P, Bagger JP. Experimental pain and psychologic status of patients with chest pain with normal coronary arteries or ischemic heart disease. Am Heart J. 2001; 142:63–71.
9. Tennant C, Mihailidou A, Scott A, et al. Psychological symptom profiles in patients with chest pain. J Psychosom Res. 1994; 38:365–371.
10. Kisely SR. The relationship between admission to hospital with chest pain and psychiatric disorder. Aust N Z J Psychiatry. 1998; 32:172–179.
11. Mayou RA, Bryant BM, Sanders D, Bass C, Klimes I, Forfar C. A controlled trial of cognitive behavioural therapy for non-cardiac chest pain. Psychol Med. 1997; 27:1021–1031.
12. Cannon RO 3rd, Quyyumi AA, Mincemoyer R, et al. Imipramine in patients with chest pain despite normal coronary angiograms. N Engl J Med. 1994; 330:1411–1417.
13. Mayou RA, Bass CM, Bryant BM. Management of non-cardiac chest pain: from research to clinical practice. Heart. 1999; 81:387–392.
14. Varia I, Logue E, O'Connor C, et al. Randomized trial of sertraline in patients with unexplained chest pain of noncardiac origin. Am Heart J. 2000; 140:367–372.
15. Wright RS, Anderson JL, Adams CD, et al. 2011 ACCF/AHA focused update incorporated into the ACC/AHA 2007 Guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in collaboration with the American Academy of Family Physicians, Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2011; 57:e215–e367.
16. Jeong W, Chang H. Rliability and Validity of Korean Version of Symptom Check list for Minor psychiatric Disorders (SCL-MPD). J Korean Neuropsychiatr Assoc. 1987; 26:15.
17. Rohani A, Akbari V, Zarei F. Anxiety and depression symptoms in chest pain patients referred for the exercise stress test. Heart Views. 2011; 12:161–164.
18. Bass C, Wade C. Chest pain with normal coronary arteries: a comparative study of psychiatric and social morbidity. Psychol Med. 1984; 14:51–61.
19. Ladwig KH, Hoberg E, Busch R. Psychological comorbidity in patients with alarming chest pain symptoms. Psychother Psychosom Med Psychol. 1998; 48:46–54.
20. Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999; 99:2192–2217.
21. Watkins LL, Grossman P, Krishnan R, Sherwood A. Anxiety and vagal control of heart rate. Psychosom Med. 1998; 60:498–502.
22. Lown B, Verrier R, Corbalan R. Psychologic stress and threshold for repetitive ventricular response. Science. 1973; 182:834–836.
23. Ramasubbu R. Insulin resistance: a metabolic link between depressive disorder and atherosclerotic vascular diseases. Med Hypotheses. 2002; 59:537–551.
24. Gold PW, Loriaux DL, Roy A, et al. Responses to corticotropin-releasing hormone in the hypercortisolism of depression and Cushing's disease. Pathophysiologic and diagnostic implications. N Engl J Med. 1986; 314:1329–1335.
25. Reynolds K, Pietrzak RH, El-Gabalawy R, Mackenzie CS, Sareen J. Prevalence of psychiatric disorders in U.S. older adults: findings from a nationally representative survey. World Psychiatry. 2015; 14:74–81.
26. D'Agostino RB Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008; 117:743–753.
27. Chen AC, Dworkin SF, Haug J, Gehrig J. Human pain responsivity in a tonic pain model: psychological determinants. Pain. 1989; 37:143–160.
28. Kim JY, Kim N, Seo PJ, et al. Association of sleep dysfunction and emotional status with gastroesophageal reflux disease in Korea. J Neurogastroenterol Motil. 2013; 19:344–354.
29. Dempe C, Jünger J, Hoppe S, et al. Association of anxious and depressive symptoms with medication nonadherence in patients with stable coronary artery disease. J Psychosom Res. 2013; 74:122–127.
30. Meyer T, Hussein S, Lange HW, Herrmann-Lingen C. Anxiety is associated with a reduction in both mortality and major adverse cardiovascular events five years after coronary stenting. Eur J Prev Cardiol. 2015; 22:75–82.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download