Abstract
Background and Objectives
We sought to determine whether an elevated homocysteine (Hcy) level is associated with a worse prognosis in Korean patients with coronary artery disease (CAD).
Subjects and Methods
A total of 5839 patients (60.4% male, mean age 61.3±11.2 years) with CAD were enrolled from 2000 to 2010 at Gangnam Severance Hospital. CAD was diagnosed by invasive coronary angiography. Laboratory values including Hcy level were obtained on the day of coronary angiography and analyses were performed shortly after sampling. Patients were divided into two groups according to their Hcy levels. Baseline risk factors, coronary angiographic findings, length of follow-up, and composite endpoints including cardiac death (CD) and non-fatal myocardial infarction (NFMI) were recorded. 1:1 propensity score matched analysis was also performed.
Results
Over a mean follow-up period of 4.4±2.5 years, there were 132 composite endpoints (75 CD and 57 NFMI) with an event rate of 2.3%. Mean Hcy level was 9.9±4.3 µmol/L (normal Hcy 7.9±1.5 µmol/L and elevated Hcy 13.9±5.1 µmol/L). Kaplan-Meier survival analysis showed an association of elevated Hcy level with worse prognosis (p<0.0001). In addition, a multivariate Cox regression analysis showed an association of elevated Hcy level with worse prognosis for both the entire cohort (hazard ratio [HR] 2.077, 95% confidence interval [CI] 1.467-2.941, p<0.0001) and the propensity score matched cohort (HR 1.982, 95% CI 1.305-3.009, p=0.001).
Homocysteine (Hcy) is a sulfur-containing amino acid metabolized either by the remethylation pathway to methionine or the transsulfuration pathway to cysteine; each pathway depends on other series of biochemical enzymes such as methionine synthetase and methylene tetrahydrofolate reductase as well as vitamin B12 and folic acid. A later pathway is dependent on the enzymes cystathionine β-synthetase and pyridoxine (vitamin B6). Any loss of one of those pathways and/or a dietary deficiency can result in an elevated Hcy level.1) Therefore, Hcy level may be influenced by factors such as nutrition, genetics, lifestyle, ethnicity, age, and gender.1)2) Epidemiological studies have demonstrated that progression of atherosclerosis plaques is correlated with elevated circulating Hcy due to increased thrombogenicity, oxidative stress status and endothelial dysfunction.3)4) Consequently, a recent large prospective study reported an independent association of elevated Hcy level with coronary artery disease (CAD), and the prognostic value of elevated Hcy level is well validated in Caucasians, both in the general population and in the patients with CAD.5)6)7)8)9) However, there are limited data regarding the prognostic value of elevated Hcy in other ethnicities. Because Hcy level may be influenced by ethnicity, it is not certain whether elevated Hcy level is associated with worse outcome in Korean patients with CAD. Therefore, we sought to evaluate the prognostic value of elevated Hcy level in such Korean patients.
A total of 5839 patients (60.4% male, mean age 61.3±11.2 years) with CAD from 2000 to 2010 at Gangnam Severance Hospital were enrolled. CAD was diagnosed by invasive coronary angiography. Laboratory values including Hcy level were obtained on the day of coronary angiography and analyses were performed shortly after sampling. Patients were divided into two groups according to their Hcy levels. Baseline risk factors, coronary angiographic findings, length of follow-up, and composite endpoints including cardiac death (CD) and non-fatal myocardial infarction (NFMI) were recorded. Institutional review committee approval and informed consent were obtained.
Risk factors were recorded as categorical variables in all patients. Hypertension was defined as systolic blood pressure≥140 mmHg and/or diastolic blood pressure≥90 mmHg, or by antihypertensive prescription. Type 2 diabetes was defined by hypoglycemic agents or insulin prescription, fasting plasma glucose≥126 mg/dL, glycosylated hemoglobin≥6.5%, or known but untreated hyperglycemia. Hyperlipidemia was defined by total cholesterol≥240 mg/dL, triglycerides≥200 mg/dL, low-density lipoprotein cholesterol≥130 mg/dL, high-density lipoprotein cholesterol<40 mg/dL, and/or by lipid-lowering prescription. A patient was considered a smoker, if the patient currently smoked or had smoked up until 1 month prior to the baseline coronary angiography. Non-obstructive CAD was defined as <50% luminal narrowing, whereas obstructive CAD was defined as ≥50% luminal narrowing. The extent of obstructive CAD was categorized according to the number of vessels involved (1, 2, or 3).
Total cholesterol, triglycerides, low-density lipoprotein cholesterol, and high-density lipoprotein cholesterol were measured directly using colorimetric and turbidimetric assays with an autoanalyzer AU5800 (Beckman Coulter, Irvine, CA, USA). Hcy measurement was determined using a commercially available enzymatic colorimetric assay AU5800 (Beckman Coulter, Irvine, CA, USA), and the values were expressed in µmol/L. Patients were divided into two groups according to the respective Hcy concentration levels: 1) normal Hcy group (lower two tertiles [Hcy median value 7.9 µmol/L, range: 0.1-10.3 µmol/L]) and 2) elevated Hcy group (upper tertile [Hcy median value 12.5 µmol/L, range: 10.4-94.0 µmol/L]).
Composite endpoints were defined as CD or NFMI. To avoid treatment bias, coronary artery revascularization procedures, such as coronary artery bypass graft surgery and percutaneous coronary intervention, were not regarded as endpoints.10) For patients with multiple cardiovascular events, only the first event was considered for analysis. Cardiac death was defined as death caused by acute myocardial infarction, ventricular arrhythmias, refractory heart failure, or cardiogenic shock. Diagnosis of NFMI required the presence of at least two of the three following criteria: characteristic chest pain, elevated cardiac enzymes, or electrocardiographic alterations indicative of myocardial infarction. Patient follow-up data were collected using electronic medical record reviews and/or standardized telephone interviews.
Continuous data were expressed as a mean value±standard deviation. All categorical data were presented as a percentage or an absolute number. Analyses of continuous data were performed using independent t-test and analyses of categorical data were performed using chi-square test to assess differences between the two groups. The C-statistic for the logistic regression model used for calculation of the propensity score matching for the 2 groups was 0.66. Patients with elevated Hcy level were then 1-to-1 matched to the patients with normal Hcy level on the propensity scores using the nearest available pair matching method. The procedure yielded 1818 well-matched pairs. Cumulative event rates as a function over time were estimated using the Kaplan-Meier method, and survival curves of composite CD/NFMI were compared using the log-rank test for both the entire cohort and the propensity score matched cohort. Univariate and multivariate Cox regression analyses were performed to determine associations between clinical characteristics (age, gender, hypertension, smoking, and hyperlipidemia), lipid parameters, Hcy, extent of CAD and clinical outcome in both the entire cohort and the propensity score-matched cohort. Hazard ratios (HRs) were calculated as an estimate of the risk associated with a particular variable with 95% confidence intervals (CIs), based on binomial distributions. All analyses were performed using SPSS version 19.0 (SPSS, Chicago, IL, USA). A p of less than 0.05 was considered statistically significant.
Of the 5839 patients in the study, 60.4% were male and the mean age was 61.3±11.2 years. Mean Hcy level was 9.9±4.3 µmol/L (7.9±1.5 µmol/L for normal Hcy groups and 13.9±5.1 µmol/L for elevated Hcy group, respectively). A summary of the baseline characteristics of both the entire cohort and propensity matched cohort according to the Hcy level is shown in Table 1. Patients with elevated Hcy levels tended to be older (p<0.0001), male (p<0.0001), diabetic (p=0.003), hypertensive (p<0.0001), smoker (p<0.0001), and hyperlipidemic (p<0.0001) (Table 1). More patients with elevated Hcy level had acute coronary syndrome at their clinical presentation (p<0.0001) (Table 1). A summary of laboratory and angiographic characteristics of both the entire cohort and the propensity matched cohort according to the Hcy level is shown in Table 2. Patients with elevated Hcy level had higher triglyceride levels (p=0.020) and lower high-density lipoprotein cholesterol levels (p<0.0001) (Table 2). In addition, elevated Hcy level showed an association with higher rates of both obstructive CAD (p<0.0001) and 3-vessel obstructive CAD (p<0.0001), at the time of baseline coronary angiography (Table 2). Consequently, higher coronary revascularization rates as well as coronary bypass graft surgery rates were observed in patients with elevated Hcy level (Table 2).
Over a mean follow-up period of 4.4±2.5 years, there were 132 composite endpoints (75 CD and 57 NFMI) with an event rate of 2.3%. The composite CD/NFMI rates were 1.5% (60/3886) and 3.7% (72/1953) for the normal Hcy and the elevated Hcy group, respectively, which were significantly different (p<0.0001) (Fig. 1A). In multivariate Cox proportional survival analysis, age (HR 1.054, 95% CI 1.035-1.073, p<0.0001), diabetes (HR 2.137, 95% CI 1.052-3.039, p<0.0001), obstructive CAD (HR 3.226, 95% CI 1.721-6.047, p<0.0001), and elevated Hcy (HR 2.077, 95% CI 1.467-2.941, p<0.0001) were independent risk factors for composite CD/NFMI (Table 3A).
After performing propensity score matching, a total of 1818 matched pairs (1818 patients from the normal Hcy group and 1818 patients from the elevated Hcy group) were generated. There were no significant differences in baseline, laboratory and angiographic characteristics for the propensity score matched subjects except for Hcy levels (Tables 1 and 2). A total of 97 composite endpoints (56 CD and 41 NFMI) occurred during the follow-up period in the matched cohorts. The respective composite CD/NFMI rates were 1.9% (34/1818) and 3.5% (63/1818) for normal Hcy and elevated Hcy group. The elevated Hcy group was associated with significantly worse outcomes than the normal Hcy group in the matched cohort (p=0.001) (Fig. 1B). In addition, in the multivariate analysis, the elevated Hcy group still had almost 2-fold higher risk for composite CD/NFMI, when compared to the normal Hcy group (HR 1.982, 95% CI 1.305-3.009, p=0.001) (Table 3B).
Hcy is an intermediate metabolite of methionine that contributes to atherosclerosis through several mechanisms, such as endothelial dysfunction, increased permeability of lipid and inflammatory cells, lipoprotein oxidation, vascular inflammation, smooth muscle proliferation, platelet activation, and abnormalities in the clotting cascade.11)12)13) During the process of Hcy metabolism pathways, any interference of one of those pathways and/or a dietary deficiency can result in elevation of Hcy level.1) Therefore, Hcy level may be influenced by factors such as nutrition, genetics, lifestyle, ethnicity, age, and gender.1) Previous study by Cappuccio et al.2) reported the discordance of Hcy levels which differ among Caucasians, African origins, and South Asians living in England, suggested a variance of the Hcy level between ethnicities. Another study reported that the frequency of the homozygous dominant mutation genotype of the enzyme methylene tetrahydrofolate reductase (C677T gene) is higher in the Hispanic population in the United States compared to other populations.14) Since, genetic polymorphism of methylene tetrahydrofolate reductase affects the Hcy level, the ethnic differences of this enzyme polymorphism may result in variations in Hcy level.
A recent large prospective cohort study reported an association of elevated Hcy level with the severity as well as the presence of CAD.5) This study confirmed this association even after correction for baseline differences, suggesting an independent role of Hcy in prediction of CAD risk. In addition, since the Hcy level may be influenced by ethnicity, several previous cross-sectional studies from non-Caucasian populations reported the association between Hcy level and CAD. Baños-González et al.15) reported an association of elevated Hcy with CAD in a Hispanic male population. Another study by Ghassibe-Sabbagh et al.16) reported an association of elevated Hcy with CAD in a Middle East Asian population. Kumakura et al.17) reported an association of elevated Hcy with CAD in Japanese patients with peripheral artery disease. Consistent with these studies, our study demonstrated that elevated Hcy levels have positive correlation with both the presence and extent of CAD in the Korean population.
Previous meta-analysis study by Homocysteine Studies Collaboration consisting of 30 prospective or retrospective studies reported that elevated Hcy is a modest independent predictor of ischemic heart disease in a healthy population.6) In addition, a recent study suggested that elevated Hcy level has additive prognostic value in terms of predicting adverse cardiac events in the general population.7) With regard to the prognostic value of elevated Hcy level in other ethnic general populations, Sun et al.18) reported a significant association of elevated Hcy level with cardiovascular events and all cause mortality in the general Chinese population. The prognostic value of elevated Hcy in patients with CAD is still a subject under debate. Previous study reported that elevated Hcy level was not associated with worse prognosis in patients with CAD.19) In contrast, other study reported that elevated Hcy level was a strong predictor of mortality in patients with CAD.8) Another study reported an association of elevated Hcy level with adverse cardiac events in patients with CAD.9) However, aforementioned studies on the prognostic value of elevated Hcy level in patients with CAD were conducted in Caucasians. In the context of these conflicting findings, we evaluated the prognostic value of elevated Hcy level in non-Caucasian (Korean) patients with CAD. In our study, we demonstrated the distribution of Hcy level in Korean patients with CAD. Besides, we documented that elevated Hcy level is associated with worse outcome in Korean patients with CAD, even after propensity score matching for other confounding variables. Therefore, we believe that our data support the clinical value of determining elevated Hcy level in Korean patients with CAD.
There are several limitations in our study. First, this was an observational study conducted at a single center. Second, there are no data for vitamin cofactors (vitamin B6 and B12 and folic acid) required for Hcy metabolism, all of which may affect the Hcy levels. Pharmacological interferences such as vitamin B/folate intake administration or some genetic mutations might have played a role in modifying Hcy levels.20) However, several randomized controlled trials and a recent meta-analysis have shown that Hcy-lowering interventions with vitamin B/folate supplementation did not reduce the occurrence of cardiovascular events, particularly coronary heart disease.21)22)23)24)25)26) In conclusion, an elevated Hcy level is associated with worse outcomes in Korean patients with CAD.
Figures and Tables
 | Fig. 1Kaplan-Meier survival analysis according to Hcy levels. (A) Total cohort and (B) propensity score matched cohort. Hcy: homocysteine. CD: cardiac death, NFMI: non-fatal myocardial infarction. |
Table 1
Baseline clinical characteristics according to Hcy levels

Table 2
Laboratory and angiographic characteristics according to Hcy levels
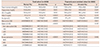
Data are expressed as number (%) or mean±standard deviation. Hcy: homocysteine, LDL-C: low density lipoprotein cholesterol, HDL-C: high density lipoprotein cholesterol, CAD: coronary artery disease, VD: vessel disease, BMS: bare metal stent, DES: drug-eluting stent, CABG: coronary artery bypass graft
Table 3
Univariate and multivariate Cox regression analysis for predicting composite CD/NFMI in (a) total cohort and (b) propensity score matched cohort

References
1. Welch GN, Loscalzo J. Homocysteine and atherothrombosis. N Engl J Med. 1998; 338:1042–1050.
2. Cappuccio FP, Bell R, Perry IJ, et al. Homocysteine levels in men and women of different ethnic and cultural background living in England. Atherosclerosis. 2002; 164:95–102.
3. Tyagi N, Sedoris KC, Steed M, Ovechkin AV, Moshal KS, Tyagi SC. Mechanisms of homocysteine-induced oxidative stress. Am J Physiol Heart Circ Physiol. 2005; 289:H2649–H2656.
4. Weiss N, Heydrick SJ, Postea O, Keller C, Keaney JF Jr, Loscalzo J. Influence of hyperhomocysteinemia on the cellular redox state--impact on homocysteine-induced endothelial dysfunction. Clin Chem Lab Med. 2003; 41:1455–1461.
5. Schaffer A, Verdoia M, Cassetti E, Marino P, Suryapranata H, De Luca G. Novara Atherosclerosis Study Group (NAS). Relationship between homocysteine and coronary artery disease Results from a large prospective cohort study. Thromb Res. 2014; 134:288–293.
6. Homocysteine Studies Collaboration. Homocysteine and risk of ischemic heart disease and stroke: a meta-analysis. JAMA. 2002; 288:2015–2022.
7. Veeranna V, Zalawadiya SK, Niraj A, et al. Homocysteine and reclassification of cardiovascular disease risk. J Am Coll Cardiol. 2011; 58:1025–1033.
8. Nygård O, Nordrehaug JE, Refsum H, Ueland PM, Farstad M, Vollset SE. Plasma homocysteine levels and mortality in patients with coronary artery disease. N Engl J Med. 1997; 337:230–236.
9. Marcucci R, Brogi D, Sofi F, et al. PAI-1 and homocysteine, but not lipoprotein (a) and thrombophilic polymorphisms, are independently associated with the occurrence of major adverse cardiac events after successful coronary stenting. Heart. 2006; 92:377–381.
10. Kwon SW, Lee BK, Hong BK, et al. Prognostic significance of elevated lipoprotein(a) in coronary artery revascularization patients. Int J Cardiol. 2013; 167:1990–1994.
11. Tanriverdi H, Evrengul H, Enli Y, et al. Effect of homocysteine-induced oxidative stress on endothelial function in coronary slow-flow. Cardiology. 2007; 107:313–320.
12. Ferretti G, Bacchetti T, Nègre-Salvayre A, Salvayre R, Dousset N, Curatola G. Structural modifications of HDL and functional consequences. Atherosclerosis. 2006; 184:1–7.
13. Dayal S, Bottiglieri T, Arning E, et al. Endothelial dysfunction and elevation of S-adenosylhomocysteine in cystathionine beta-synthase-deficient mice. Circ Res. 2001; 88:1203–1209.
14. Wilcken B, Bamforth F, Li Z, et al. Geographical and ethnic variation of the 677C>T allele of 5,10 methylenetetrahydrofolate reductase (MTHFR): findings from over 7000 newborns from 16 areas world wide. J Med Genet. 2003; 40:619–625.
15. Baños-González MA, Anglés-Cano E, Cardoso-Saldaña G, et al. Lipoprotein(a) and homocysteine potentiate the risk of coronary artery disease in male subjects. Circ J. 2012; 76:1953–1957.
16. Ghassibe-Sabbagh M, Platt DE, Youhanna S, et al. Genetic and environmental influences on total plasma homocysteine and its role in coronary artery disease risk. Atherosclerosis. 2012; 222:180–186.
17. Kumakura H, Fujita K, Kanai H, et al. High-sensitivity C-reactive protein, lipoprotein(a) and homocysteine are risk factors for coronary artery disease in Japanese patients with peripheral arterial disease. J Atheroscler Thromb. 2015; 22:344–354.
18. Sun Y, Chien KL, Hsu HC, Su TC, Chen MF, Lee YT. Use of serum homocysteine to predict stroke, coronary heart disease and death in ethnic Chinese. 12-year prospective cohort study. Circ J. 2009; 73:1423–1430.
19. Zairis MN, Ambrose JA, Manousakis SJ, et al. The impact of plasma levels of C-reactive protein, lipoprotein (a) and homocysteine on the long-term prognosis after successful coronary stenting: the global evaluation of new events and restenosis after stent implantation study. J Am Coll Cardiol. 2002; 40:1375–1382.
20. van Oijen MG, Claessen BE, Clappers N, et al. Prognostic value of free plasma homocysteine levels in patients hospitalized with acute coronary syndrome. Am J Cardiol. 2008; 102:135–139.
21. Martí-Carvajal AJ, Solà I, Lathyris D. Homocysteine-lowering interventions for preventing cardiovascular events. Cochrane Database Syst Rev. 2015; 1:CD006612.
22. Miller ER 3rd, Juraschek S, Pastor-Barriuso R, Bazzano LA, Appel LJ, Guallar E. Meta-analysis of folic acid supplementation trials on risk of cardiovascular disease and risk interaction with baseline homocysteine levels. Am J Cardiol. 2010; 106:517–527.
23. Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine (SEARCH) Collaborative Group. Armitage JM, Bowman L, et al. Effects of homocysteine-lowering with folic acid plus vitamin B12 vs placebo on mortality and major morbidity in myocardial infarction survivors: a randomized trial. JAMA. 2010; 303:2486–2494.
24. Bønaa KH, Njølstad I, Ueland PM, et al. Homocysteine lowering and cardiovascular events after acute myocardial infarction. N Engl J Med. 2006; 354:1578–1588.
25. Lonn E, Yusuf S, Arnold MJ, et al. Homocysteine lowering with folic acid and B vitamins in vascular disease. N Engl J Med. 2006; 354:1567–1577.
26. Ebbing M, Bønaa KH, Arnesen E, et al. Combined analyses and extended follow-up of two randomized controlled homocysteine-lowering B-vitamin trials. J Intern Med. 2010; 268:367–382.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download