Abstract
Background and Objectives
We assessed the ability of portable echocardiography (with contrasts) to clearly delineate the cardiac structure, and evaluated the impact of its use on the diagnosis and management of critically ill patients in Korea.
Subjects and Methods
We prospectively enrolled 123 patients (mean age 66±16 years), who underwent portable transthoracic echocardiography (with contrast) for image enhancement at 12 medical centers. The quality of the global left ventricular (LV) images, the number of the regional LV segments visualized, the ability to visualize the LV apex and the right ventricle (RV), and any changes in the diagnostic procedure and treatment strategy were compared before and after the contrast.
Results
Of the 123 patients, 52 (42%) were using mechanical ventilators. The amount of poor or uninterpretable images decreased from 48% to 5% (p<0.001), after the contrast. Before the contrast, 15.6±1.1 of 16 LV segments were seen, which improved to 15.9±0.6 segments (p=0.001) after the contrast. The ability to visualize the LV apex increased from 47% to 94% (p<0.001), while the inability to clearly visualize the RV decreased from 46% to 19% (p<0.001). Changes in the diagnostic procedure (for example, not requiring other types of imaging studies) were observed in 18% of the patients, and the treatment plan (medication) was altered in 26% of patients after the contrast echocardiography.
Echocardiography has become an integral part of modern cardiovascular imaging. It is a relatively simple procedure, and it is noninvasive, inexpensive, and easily accessible, even at a bedside or an outpatient clinic. Echocardiography has become an invaluable tool for the management of critically ill patients, to provide rapid, detailed information regarding the cardiovascular system. It can noninvasively elucidate the cardiac function and structure, and provide vital information for the management of hemodynamically unstable patients in intensive care settings, including medical or surgical intensive care units (ICUs) and coronary care units.1)
Portable echocardiography, for the management of critically ill patients, often has limitations; these are mostly related to suboptimal imaging conditions and a constrained physical environment within the ICU. Indeed, the partial or complete failure rate of fundamental transthoracic echocardiography (due to incomplete endocardial resolution) is reported to be 30% to 40% in critically ill patients in the ICU.2)3)4) Furthermore, additional diagnostic tests, including transesophageal echocardiography, radionuclide scans, cardiac computed tomography, or even invasive coronary angiography may be necessary.
Recently, contrast echocardiography, for the purpose of enhancing the endocardial border, has been widely employed to improve the assessment of the global and regional left ventricular (LV) function, the detection of LV thrombi, and the discrimination of cardiac structures.3)5)6)7)8) The impact of contrast echocardiography on the diagnosis and management of ICU patients has been validated previously8)9)10)11)12); however, there have been no reports on the usefulness of portable echocardiography (with contrast agents) in Korean ICU settings, with patients who generally have small bodies and thin chest walls (possibly resulting in a better transthoracic view compared to patients from other regions). Therefore, we assessed the ability of portable contrast echocardiography to delineate the cardiac chamber structures, and the impact of its use on the diagnosis and management of critically ill patients in Korea.
Consecutive patients from 12 Korean medical centers, who received contrast agents (due to the technical difficulties of bedside portable echocardiographies in ICUs) between July 2009 and November 2013, were enrolled. The study was approved by the hospital ethics committee at each study center.
Two-dimensional (and Doppler, if available) transthoracic echocardiography was performed with the portable machines available at each study center, by a cardiology fellow or a cardiologist. Baseline images were obtained using second harmonic imaging, with other settings tailored to optimize the image quality. If the conventional echocardiographic study was regarded as technically difficult (namely, having poor echo windows), contrast echocardiography was performed using a low mechanical index (MI) of between 0.3 and 0.5, according to the American Society of Echocardiography guidelines.13) The contrast agents used were Definity (Lantheus Medical Imaging, North Billerica, MA, USA) and SonoVue (Bracco Diagnostics, Milan, Italy), which were delivered by bolus injection or by continuous intravenous infusion, according to the manufacturer's instructions. All images were digitally stored, and interpreted within a few hours by a blinded cardiologist (investigator) at each study center.
The conventional and contrast echocardiographic images were separately analyzed, with regard to:
(1) The global LV image quality
(2) The number of visualized LV myocardial segments
(3) The ability to visualize the LV apex, including thrombi, aneurysms or pseudoaneurysms, false tendons or trabeculations, or apical hypertrophy
(4) The ability to visualize the right ventricle (RV), which is estimated semi-quantitatively (Table 1)
(5) The LV ejection fraction (EF), estimated in incremental ranges of 10%.
The regional LV function was assessed, using a 16 myocardial segment model.14)
After the interpretation of the echocardiographic study, the attending physician was asked whether the result of the contrast echocardiography would alter the requirement for further diagnostic procedures (such as transesophageal echocardiography, radionuclide scans, computed tomography, or coronary angiography), or change the management plans (therapeutic procedures or medication).
The safety end points that were monitored and recorded were: significant hypotension, an anaphylactoid reaction, any new chest pain, cardiac arrhythmia requiring intervention, cardiac arrest, or death within 24 h of contrast administration.
Statistical analyses were performed, using SPSS for Windows (version 12.0; SSPS Inc., Chicago, IL, USA). Continuous variables were expressed as the mean±standard deviation. Categorical variables were expressed as group percentages. McNemar and Wilcoxon signed rank tests were used to estimate the significant differences in the visualized echocardiographic parameters, before and after contrast, as well as the clinical impact of contrast echocardiography. A p value of <0.05 was considered significant.
A total of 123 consecutive patients were enrolled in the study, for which the mean age was 66±16 years. There were 62 patients admitted to cardiology departments (50%). 52 (42%) of the total 123 patients were using mechanical ventilators (Table 2). The common indications for echocardiography were chest discomfort, ischemic heart disease, and heart failure (Table 3). Definity was the main contrast agent used in the study (Table 4). For the delivery, the bolus injection method was used more often than the continuous intravenous infusion method.
The incidence of "uninterpretable" or "poor quality" global LV images decreased from 48% (pre-contrast) to 5% (post-contrast) (p<0.001) (Fig. 1). The average number of visualized LV myocardial segments improved from 15.6±1.1 to 15.9±0.6 of 16 LV segments, after the contrast echocardiography (p=0.001). The visualization of the LV apex was adequate (fair and excellent) in 47% of the cases (pre-contrast) and in 94% of the cases (post-contrast) (p<0.001) (Fig. 2). The ability to visualize the RV was adequate in 54% of the cases (pre-contrast) and increased to 81% of the cases (post-contrast) (p<0.001) (Fig. 3). The estimated EF was uninterpretable in 13 patients (10.7%; pre-contrast) and in only 1 patient (0.8%; post-contrast). There was no significant difference between pre- and post-contrast in the estimated EF, in incremental ranges of 10% (p=0.106) (Fig. 4).
Contrast echocardiography decreased the need for additional diagnostic imaging procedures in 22 (18%) patients {8 avoided transesophageal echocardiographies; 2 avoided coronary angiographies; 12 avoided other imaging (nuclear scan or computed tomography)} (Fig. 5). The management strategy was altered in 32 (26%) patients after contrast echocardiography (19 avoided additional procedures; 12 changed medication; 1 both avoided additional procedures and changed medication) (Fig. 6).
There were no reported serious adverse effects of contrast use, potentially including hemodynamic changes, cardiac arrhythmia, injection site reaction, back or renal pain, chest pain or discomfort, headache, dizziness, flushing, and gastrointestinal symptoms.
This multicenter study demonstrated that the use of contrast agents, during portable echocardiography in intensive care settings, can improve the image quality and impact the diagnostic procedures and treatment plans in Korean patients. Bedside portable echocardiography, in an ICU setting, is frequently suboptimal as a result of the challenges related to changing the patient position, the lack of patient cooperation, ventilator use, critical lung problems, and the placement of catheters adjacent to the heart. Thus, other imaging tests may be required for diagnosis and management. Transesophageal echocardiography can be done at the bedside, but it is relatively invasive, technically difficult, and is risky in the ICU setting. Other cardiac imaging tests, such as radionuclide scans and cardiac computed tomography, are time consuming and cannot be performed at the bedside.
Contrast echocardiography opacifies the cardiac chambers, thus enhancing the detection of the endocardial borders. This technique would be useful in patients having poor echo images. In several previous studies, contrast echocardiography proved to be beneficial during stress tests, and in ICU settings.5)9)10)11) The number of LV myocardial segments visualized, pre-contrast, was larger (with an average of 15.6 segments) in our study than in similar studies conducted be Kurt et al.8) (with an average of 11.5 segments) and Reilly et al.9) (with an average of 11.6 segments). These findings may imply the possibility of better transthoracic echocardiography imaging in Koreans than in patients from other regions, and may partly explain why 18% of the patients in our study experienced a decrease in the requirement of alternate diagnostic procedures-after contrast echocardiography-compared to the 32% in the study conducted by Kurt et al.8) The benefit of contrast echocardiography, when it comes to visualizing the RV, has been considered to be lower than that of visualizing the LV1)5)15); however, our study indicated that contrast echocardiography did improve the visualization of the RV.
This study has some limitations. First, the sample size is relatively small, in spite of the fact that it is a multicenter study. Second, a selection bias may exist, since this study depends on the physician's decision regarding echocardiographic image quality and the necessity for contrast echocardiography. Since contrast imaging has been known to be beneficial compared to the conventional echocardiography, the reviewers could have been biased toward the contrast imaging. Third, the determination of the impact of the contrast echocardiography on additional diagnostic procedures and management depends on the attending physician's decision, which could differ between doctors. Finally, because there is no comparative gold standard diagnostic imaging modality, such as cardiac magnetic resonance or nuclear scan, we may not know whether the result of the "better interpretation" after contrast is really correlated with increased accuracy.
In conclusion, portable echocardiography, using a contrast agent, impacts the diagnostic procedures and management plans due to the enhanced image quality and opacification of the cardiac chambers and structures in Korean ICU patients.
Figures and Tables
Fig. 1
The effect of contrast echocardiography on the global left ventricular (LV) image quality. Contrast echocardiography significantly improves the general LV image quality, compared to fundamental echocardiography (McNemar's test, p<0.001 comparing uninterpretable and poor with fair and adequate).
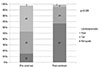
Fig. 2
The effect of contrast echocardiography on the visualization of the left ventricular (LV) apex. Contrast echocardiography significantly improves the ability to visualize the LV apex, compared to fundamental echocardiography (p<0.001).
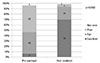
Fig. 3
The effect of contrast echocardiography on the visualization of the right ventricle (RV). Contrast echocardiography significantly improves the ability to visualize the RV (p<0.001).
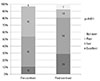
Fig. 4
A comparison of the estimated ejection fractions, between pre-contrast and post-contrast images (Wilcoxon signed rank test, p=0.106, in incremental ranges of 10%).

Fig. 5
The impact of contrast echocardiography on diagnostic procedures. Contrast echocardiography decreased the need for additional diagnostic imaging procedures in 22 patients (18%). TEE: transesophageal echocardiography, CAG: coronary angiography.

Fig. 6
The impact of contrast echocardiography on management strategies. Contrast echocardiography altered the management plan for 32 patients (26%).

Table 1
The scoring system for the quality of each image

Table 2
The baseline characteristics of the subjects
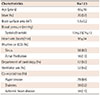
Table 3
The clinical indications for portable echocardiography

Table 4
The characteristics of contrast echocardiography

References
1. Beaulieu Y. Bedside echocardiography in the assessment of the critically ill. Crit Care Med. 2007; 35:5 Suppl. S235–S249.
2. Senior R, Dwivedi G, Hayat S, Lim TK. Clinical benefits of contrast-enhanced echocardiography during rest and stress examinations. Eur J Echocardiogr. 2005; 6:Suppl 2. S6–S13.
3. Hwang JJ, Shyu KG, Chen JJ, Tseng YZ, Kuan P, Lien WP. Usefulness of transesophageal echocardiography in the treatment of critically ill patients. Chest. 1993; 104:861–866.
4. Cook CH, Praba AC, Beery PR, Martin LC. Transthoracic echocardiography is not cost-effective in critically ill surgical patients. J Trauma. 2002; 52:280–284.
5. Senior R, Becher H, Monaghan M, et al. Contrast echocardiography: evidence-based recommendations by European Association of Echocardiography. Eur J Echocardiogr. 2009; 10:194–212.
6. Hundley WG, Kizilbash AM, Afridi I, Franco F, Peshock RM, Grayburn PA. Administration of an intravenous perfluorocarbon contrast agent improves echocardiographic determination of left ventricular volumes and ejection fraction: comparison with cine magnetic resonance imaging. J Am Coll Cardiol. 1998; 32:1426–1432.
7. Hundley WG, Kizilbash AM, Afridi I, Franco F, Peshock RM, Grayburn PA. Effect of contrast enhancement on transthoracic echocardiographic assessment of left ventricular regional wall motion. Am J Cardiol. 1999; 84:1365–1368. A8–A9.
8. Kurt M, Shaikh KA, Peterson L, et al. Impact of contrast echocardiography on evaluation of ventricular function and clinical management in a large prospective cohort. J Am Coll Cardiol. 2009; 53:802–810.
9. Reilly JP, Tunick PA, Timmermans RJ, Stein B, Rosenzweig BP, Kronzon I. Contrast echocardiography clarifies uninterpretable wall motion in intensive care unit patients. J Am Coll Cardiol. 2000; 35:485–490.
10. Makaryus AN, Zubrow ME, Gillam LD, et al. Contrast echocardiography improves the diagnostic yield of transthoracic studies performed in the intensive care setting by novice sonographers. J Am Soc Echocardiogr. 2005; 18:475–480.
11. Yong Y, Wu D, Fernandes V, et al. Diagnostic accuracy and cost-effectiveness of contrast echocardiography on evaluation of cardiac function in technically very difficult patients in the intensive care unit. Am J Cardiol. 2002; 89:711–718.
12. Jung HO. Pericardial effusion and pericardiocentesis: role of echocardiography. Korean Circ J. 2012; 42:725–734.
13. Mulvagh SL, Rakowski H, Vannan MA, et al. American Society of Echocardiography Consensus Statement on the clinical applications of ultrasonic contrast agents in echocardiography. J Am Soc Echocardiogr. 2008; 21:1179–1201. quiz 1281
14. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005; 18:1440–1463.
15. Mulvagh SL, DeMaria AN, Feinstein SB, et al. Contrast echocardiography: current and future applications. J Am Soc Echocardiogr. 2000; 13:331–342.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download