Abstract
Background and Objectives
The prognostic role of the right atrium (RA) compared with that of the left atrium (LA) is unclear in patients with atrial fibrillation (AF). We assessed structural changes in both atria and determined their association with recurrence of AF after radiofrequency catheter ablation (RFCA).
Subjects and Methods
All 111 patients with nonvalvular AF (87 men; mean age, 57±11 years; 68 with paroxysmal AF) who underwent RFCA were enrolled consecutively. Three-dimensional volumes of both atria measured from computed tomography images were compared between subjects with and without recurrence of AF during the follow-up.
Results
Early (<3 months), 6-month, and 1-year recurrence was documented in 26 (24%), 30 (27%), and 36 (32%) patients, respectively. Significantly larger RA and LA volume indices (RAVI and LAVI) were observed in the early, 6-month, and 1-year recurrence groups (p<0.05 for all). In multivariate analysis, Early recurrence was independently associated with RAVI (for each 10 mL/m2 increase; odds ratio [OR], 1.31; 95% confidence interval [CI], 1.03-1.66, p= 0.03), but not with LAVI. However, both RAVI and LAVI failed to predict 6-month outcomes independently. LAVI was the only independent predictor of 1-year recurrence (for each 10 mL/m2 increase; OR, 1.36; 95% CI, 1.08-1.71, p=0.009).
Conclusion
RA enlargement was more closely related to early recurrence of AF after RFCA than LA size. However, LA size, rather than RA volume, was a determinant of long-term AF prognosis after RFCA. These findings suggest a temporal pattern in the prognostic implication of enlargement in each atrium that switches over time after RFCA for AF.
Atrial fibrillation (AF) is the most common sustained cardiac rhythm disorder.1) Although pharmacological therapy for rate and/or rhythm control has been the mainstay of treatment for arrhythmia, recently introduced radiofrequency catheter ablation (RFCA) is a robust and promising technique for eradicating AF in carefully selected patients.2) However, a considerable proportion of patients fail to maintain sinus rhythm even after successful RFCA; thus, predicting outcome is clinically important for selecting appropriate patients before the procedure.
AF causes various anatomical and electrical changes in the atria, which play a pathological role generating and maintaining the arrhythmia.3)4) Patients with more severe left atrial (LA) disease experience earlier and more frequent AF recurrence after the index RFCA. In contrast, because structurally evaluating the chamber is difficult with two-dimensional echocardiography, which has been the most widely used cardiac imaging modality, knowledge regarding the prognostic implications of right atrial (RA) size is relatively limited. Multi-detector computed tomography (MDCT) is a promising tool for three-dimensional evaluation of cardiac chamber anatomy and is superior to conventional echocardiography for that purpose. In this study, we investigated the prognostic implications of three-dimensional RA and LA enlargement assessed with MDCT after RFCA for AF.
All 111 patients (87 males; mean age, 57±11 years) with nonvalvular AF who underwent RFCA between 2009 and 2011 were enrolled consecutively at the Severance Cardiovascular Hospital (Seoul, Korea). Patients with any medical history of cardiomyopathy, pericardial disease, or valvular heart disease with moderate or greater severity or a congenital cardiac abnormality were excluded. None of the patients in this cohort suffered from lung diseases, including chronic obstructive pulmonary disease or pulmonary hypertension which may cause right-heart structural/functional changes. Paroxysmal atrial fibrillation (PaAF) was defined as a history of one or more episodes of self-terminating AF lasting ≤7 days. Patients who had an AF episode that lasted >7 days or required termination by cardioversion either with antiarrhythmic drugs or by direct current cardioversion were allocated into the persistent atrial fibrillation (PeAF) group. This study protocol was approved by the Institutional Review Board of Severance Cardiovascular Hospital, and complied with the Declaration of Helsinki (sixth revision). All patients in this study cohort provided written informed consent.
Conventional transthoracic echocardiographic evaluations were performed using commercially available equipment (Vivid 9, GE Vingmed ultrasound, Horten, Norway or Sonos 5500, Philips Medical Systems, Andover, MA, USA) in all subjects before the index procedure. Standard M-mode, two-dimensional, and color Doppler imaging were performed in the parasternal and apical views. Left ventricular (LV) ejection fraction was calculated from two-dimensional recordings using the modified Quinones method. All measurements were averaged over five cardiac cycles. The echocardiographic data were analyzed by two blinded echocardiographer cardiologists.
Cardiac MDCT scans were performed using a dual-source computed tomography (CT) (Somatom Definition Flash, Siemens Healthcare, Forchheim, Germany). Scan delay times between the start of contrast injection and scanning were determined for each patient using the test bolus technique. After a 10 mL intravenous injection of iopamidol (Pamiray 370; 370 mg iodine/mL, Dongkook Pharma, Seoul, Korea) followed by 20 min of saline at 5 mL/s, optimal delay times were determined by automatic evaluation of contrast enhancement in the ascending aorta. Contrast-enhanced cardiac CT was performed using the triple phase injection method (60-80 mL iopamidol followed by 30 mL 30% blended iopamidol with saline and 20 mL saline at 5 mL/s). Scanning was performed using the following parameters: retrospective electrocardiography (ECG)-gated spiral acquisitions or prospective axial acquisition targeting end-systole, 80-120 kVp and 280-450 mAs depending on patient size. Images used to measure maximum atrial volume were reconstructed at the end-systolic phase just before atrioventricular valve opening at a slice thickness of 0.75 mm, an increment interval of 0.5 mm, and a medium-smooth convolution kernel of B36f. All atrial volumes were measured by two experienced radiologists with consensus, who were unaware of the patients' clinical and electrophysiological data, using software (Aquaris Intuition Edition V4.4.6, TeraRecon, San Francisco, CA, USA). Atria were automatically or semi-automatically segmented based on the three-dimensional threshold method and atrial volumes were determined after manually excluding the pulmonary veins and vena cavi (Fig. 1). Atrial volume was indexed to each patient's body surface area {right atrial volume indices (RAVI) and left atrial volume indices (LAVI), respectively}. Left atrial appendage (LAA) volume was also separately measured and indexed to each patient's body surface area.
The electrophysiological study was performed in the postabsorptive state with the patients sedated with midazolam and fentanyl. Three-dimensional geometry of the LA was reconstructed with the CARTO (Biosense Webster, Diamond Bar, CA, USA) or NavX (St Jude Medical, Inc., Minnetonka, MN, USA) electroanatomic mapping system. The circumferential pulmonary vein was isolated in all patients using a 3.5-mm irrigated-tip catheter (ThermoCool, Biosense Webster, CA, USA). We used a circular mapping catheter {Lasso (Biosense Webster, Diamond Bar, CA, USA)} to confirm isolation of the pulmonary veins. Successful ablation was defined as the elimination of all pulmonary vein potentials along the antrum or inside the veins (entry block). If AF was not terminated after eliminating all pulmonary vein potentials, linear ablation and complex fragmented atrial electrogram ablation were performed. Cavotricuspid isthmus ablation was performed in all patients.
The patients were monitored continuously by ECG during their hospital stay before and after the index RFCA. After the index procedure, the patients were discharged without routine antiarrhythmic drugs and were followed up with a clinical examination, ECG, and Holter monitoring at 1, 3, 6, 9, and 12 months. Patients who developed recurrence of symptoms between follow-up visits were evaluated with a clinical examination, ECG, and Holter monitoring. AF recurrence within the first 3 months after ablation was defined as early recurrence, and anti-arrhythmic drug treatment (class Ic or amiodarone) followed by electrical cardioversion was initiated. Oral anticoagulation therapy was prescribed for at least 3 months. We divided the study subjects based on the presence of early recurrence (<3 months), 6-month recurrence, or 1-year recurrence of AF after successful catheter ablation.
Continuous data are expressed as mean±standard deviation and normality tests were performed for each variable. The baseline characteristics between the groups were compared using the two-sample t-test for continuous variables, and the chi-square test and Fisher's exact test for categorical variables. Univariate and multivariate logistic regression analyses were performed to identify factors associated with early recurrence or long-term outcomes. Pearson's bivariate correlation analysis was used to determine the correlation between variables. We calculated the variance inflation factor in the multiple regression analysis model to assess multicollinearity. Receiver operating characteristics curves were used to determine the accuracy of variables for predicting recurrence. A p value <0.05 was considered significant.
The baseline characteristics of the entire cohort are shown in Table 1. The clinical characteristics were similar between the PaAF and PeAF groups, although more PeAF patients had accompanying hypertension (p=0.045). The LV ejection fraction on echocardiography was not different between the groups; however, PeAF patients had a larger LA anterior-posterior diameter (p<0.001). PeAF patients had larger RAVI (83±19 vs. 104±29 mL/m2, p<0.001) and LAVI (73±18 vs. 101±29 mL/m2, p<0.001) on MDCT evaluation than those of PaAF patients. Concurrently, indexed LAA size was greater in PeAF (9±3 mL/m2) than that in the PaAF (7±3 mL/m2, p<0.001) group. However, RA and LA conduction velocities did not differ between the groups. Procedural, fluoroscopic, and ablation times were significantly longer in PeAF patients than those in the PaAF patients. Additional ablation procedures, including complex fractionated atrial electrogram ablation and LA roof or left anterior ablation were more frequently performed in the PeAF group. Complications after RFCA were noted as one cardiac tamponade treated with pericardiocentesis, one stroke, and five puncture site hematomas.
Comparisons of clinical characteristics, echocardiographic parameters, MDCT findings, and electrophysiological characteristics between patients with early recurrence and subjects without early recurrence are shown in Table 2. The proportion of PeAF was higher in the early recurrence group than that in the no recurrence group (33% vs. 56%, respectively, p=0.04), but other demographic findings did not differ between the groups. However, both atrial volume indices and indexed LAA size measured by MDCT were significantly larger in the early recurrence than in the no recurrence group (p<0.05 for all). RAVI and LAVI showed no significant multicollinearity when assessed by the variance inflation factor tolerance. Early recurrence was independently associated with RAVI {for each 10 mL/m2 increase; odds ratio (OR), 1.31; 95% confidence interval (CI), 1.03-1.66; p=0.03}, but not with LAVI in the multivariate analysis (Table 3). RAVI of 89 mL/m2 showed fair sensitivity (0.704) and specificity (0.631) for predicting early recurrence (area under curve: 0.691, p=0.003).
Comparisons of clinical characteristics, echocardiographic parameters, MDCT findings, and electrophysiological parameters between patients with 6-month recurrence and without recurrence are summarized in Table 2. Demographic findings were grossly similar, although the proportion of PeAF tended to be higher in the recurrence group with borderline significance (33% vs. 53%, respectively, p=0.06). LV ejection fraction and LA anterior-posterior diameter did not differ between the groups. However, RAVI and LAVI determined by MDCT were significantly greater in patients with recurrence than in those without (p<0.05 for all). Both atrial volumes failed to independently predict 6-month recurrence in the multivariate logistic regression analysis (Table 3).
Comparisons of clinical characteristics, echocardiographic parameters, MDCT findings, and electrophysiological parameters between patients with long-term recurrence (1-year recurrence) and subjects without recurrence are shown in Table 2. The proportion of PeAF was significantly higher in patients with 1-year recurrence than in those with long-term recurrence (37% vs. 64%, respectively, p<0.001), but other demographic findings were similar including the CHADS2 score. Echocardiographically measured LA anterior-posterior diameter was significantly greater in the recurrence group than that in no recurrence group (p=0.008). Both atrial volumes determined by MDCT were significantly larger in the recurrence group (p<0.05 for all). In a multivariate logistic regression analysis, LAVI was the only independent predictor of 1-year recurrence (for each 10 mL/m2 increase: OR, 1.36; 95% CI; 1.08-1.71, p=0.009). In contrast, RAVI was not an independent determinant of 1-year recurrence after RFCA for AF (Table 3). LAVI of 86 mL/m2 showed fair sensitivity (0.639) and specificity (0.733) for predicting 1-year recurrence (area under curve: 0.710, p<0.001).
RAVI was positively correlated with LAVI (Fig. 2) (r=0.68, p<0.001). The significant linear correlation observed between RAVI and LAVI was also observed in the PaAF (r=0.62, p<0.0001) and PeAF groups (r=0.61, p<0.001). In addition, we calculated the RA/LA ratio, and the values were 1.13±0.25 in the entire study group. Interestingly, the RA/LA ratio was significantly higher in the early recurrence group than that in subjects without recurrence (Table 2 and Fig. 3). However, the RA/LA ratio tended to be not different between patients with and without 6-month (data not shown) or 1-year recurrence (Table 2 and Fig. 3).
We found that: (1) increased RA volume was linearly correlated with the severity of LA enlargement in patients with nonvalvular AF; (2) RA enlargement was closely associated with early recurrence of AF after RFCA than that of LA volume; and (3) LA enlargement, rather than RA size, played a key role predicting long-term outcome of AF after the index procedure. Our results suggest that RA and LA play a potential role in AF recurrence, particularly during the early period after RFCA. A temporal pattern was detected in the prognostic implications of each atrial volume that changed over time after the index procedure.
Atrial structural/electrical remodeling is commonly observed in patients with AF.5)6)7)8) Many forms of atriopathies induced by AF play a key role in the occurrence and maintenance of the arrhythmia (so called "AF begets AF").4)9)10) However, this knowledge is mainly based on LA studies, whereas little is known about the potential relationship between RA disease and pathophysiology/prognosis of AF. Echocardiography has been traditionally used to structurally evaluate the cardiac chambers; however, an evaluation of the RA is technically challenging,11) which may, at least in part, be responsible for our lack of knowledge regarding the RA not only in patients with AF but also in other cardiac diseases. MDCT provides more reliable three-dimensionally reconstructed cardiac chamber images with higher spatial resolution than that of two-dimensional echocardiography; thus, we were able to determine the sizes of both atria accurately and relatively free from intra and interobserver variations. Anatomical and histological changes in the RA in patients with AF have been recognized with recent advances in cardiac imaging tools and electrophysiology.12)13)14) In an insightful study conducted in patients with AF who underwent RFCA, O'Neill et al.15)M. reported that about 1 in 5 AF events have a RA origin. In the current study, we observed that RA size increased in a close association with LA enlargement in patients with AF. In addition, patients with a more chronic form of AF suffer more severe RA structural changes.
Early recurrence following RFCA of AF is relatively common, and the rate of early recurrence is 37.8% (range 15.9-65.0%) in multiple investigations implementing a 3-month blanking period.16) Although the exact mechanisms for early recurrence after RFCA remain to be determined, numerous predictors have been suggested,17) such as acute inflammation, local irritation, and/or increased levels of circulating catecholamines after RFCA.18) We reported previously that RA size is an independent predictor of early recurrence, whereas LA volume is not.19) In the current study, we further support our previous observations in a larger cohort. The data from the current study suggest that chronic RA disease also affects early outcomes after RFCA, and that it may be more important than LA size in terms of predicting early recurrence.
LA enlargement has been reportedly correlated with early recurrence;18)20)21)22)23) however, those investigators did not include RA volume in their data analysis. In the current study, patients with severe LA enlargement were clinically excluded before the procedure by the attending cardiologists. Therefore, our data can be interpreted as: (1) a current RFCA technique can sufficiently eradicate the pathological substrate for AF in LA; thus, (2) RA volume has an independent and additional prognostic implication, which is greater than LA size, for early recurrence in carefully selected patients for RFCA who have a "not-so-large" LA. In contrast, we failed to determine the prognostic implications of RA or LA conduction velocity.
We observed a temporal change in the prognostic implication pattern of each atrial size after RFCA (i.e., RAVI for early recurrence and LAVI for 1-year recurrence). RA size remained greater in patients with longer-term recurrence (6-month and 1-year recurrence), but it failed to independently predict longer-term recurrence. We also observed that LA volume served as a key predictor of post RFCA longer-term recurrence, which is parallel with data from other investigations.20)23)24)25)26)27) The unique findings of our study are that enlargement of the LA predicts AF recurrence independently from RA size, and that RA structural changes have a limited role in terms of predicting long-term maintenance of sinus rhythm after the index procedure. This result is contradictory with the findings of Akutsu et al.28) who emphasized the role of RA as a long-term prognosticator after RFCA in PaAF patients. The discrepancy might be explained by the different study groups (inclusion of PeAF or not) because our results demonstrate that the proportion of PeAF patients in the 1-year recurrence group was greater than that in the early recurrence group, and that RA volume was not as strong as LA size for predicting 1-year recurrence. Therefore, a diseased LA serves as a more important nidus for the arrhythmia substrate than RA, as AF becomes more chronic.
Our study is based on data from a single tertiary center; thus, the study group was not representative of all patients with AF. However, this is the largest study investigating RA using MDCT in patients with AF. Second, although MDCT is a promising diagnostic modality for measuring of cardiac chamber size, the method has not been widely validated. Finally, RFCA for AF decreases LA size27); thus, the change in RA size after the index procedure is essential to elucidate reverse RA remodeling. Unfortunately, we did not perform a follow-up RA size measurement in our cohort.
Figures and Tables
Fig. 1
Three-dimensional measurements of right atrial (A), left atrial (B), and left atrial appendage (C) volumes using software (Aquaris Intuition Edition V4.4.6, TeraRecon, San Francisco, CA, USA) on multidetector computed tomography images.

Fig. 2
Strong linear correlation between the right atrial and left atrial volume indices in patients with/without early recurrence (A) and in patients with/without 1-year recurrence (B). RAVI: right atrial volume indices, LAVI: left atrial volume indices.

Fig. 3
Comparisons of both atrial volume indices and the ratio of right atrial (RA) volume to left atrial (LA) size between patients with/without early (A) or 1-year recurrence (B). Note that RA/LA is significantly higher in the early recurrence group, but not in the 1-year recurrence group. RAVI: right atrial volume indices, LAVI: left atrial volume indices.

Table 1
Baseline clinical characteristics, echocardiographic parameters, and MDCT findings and intergroup comparisons between patients with paroxysmal and persistent AF

MDCT: multidetector computed tomography, AF: atrial fibrillation, PaAF: paroxysmal atrial fibrillation, PeAF: persistent atrial fibrillation, CHF: congestive heart failure, LVEF: left ventricular ejection fraction, LA: left atrium/atrial, RA: right atrium/atrial, LAA: left atrial appendage; CFAE: complex fractionated atrial electrogram. *p<0.05
Table 2
Comparisons of clinical characteristics, echocardiographic parameters, and MDCT findings of patients according to recurrence after AF catheter ablation
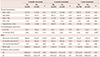
Table 3
Predictors of recurrence over time after successful catheter ablation of atrial fibrillation

Acknowledgements
We thank the Research Affairs Department of Yonsei University College of Medicine for its assistance with the statistical analysis.
This study was supported by a grant from the Korea Society of Cardiology (2012).
References
1. Heeringa J, van der Kuip DA, Hofman A, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J. 2006; 27:949–953.
2. Wann LS, Curtis AB, January CT, et al. 2011 ACCF/AHA/HRS focused update on the management of patients with atrial fibrillation (updating the 2006 guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2011; 123:104–123.
3. Wijffels MC, Kirchhof CJ, Dorland R, Allessie MA. Atrial fibrillation begets atrial fibrillation. A study in awake chronically instrumented goats. Circulation. 1995; 92:1954–1968.
4. Ausma J, Wijffels M, Thoné F, Wouters L, Allessie M, Borgers M. Structural changes of atrial myocardium due to sustained atrial fibrillation in the goat. Circulation. 1997; 96:3157–3163.
5. Allessie M, Ausma J, Schotten U. Electrical, contractile and structural remodeling during atrial fibrillation. Cardiovasc Res. 2002; 54:230–246.
6. Avitall B, Bi J, Mykytsey A, Chicos A. Atrial and ventricular fibrosis induced by atrial fibrillation: evidence to support early rhythm control. Heart Rhythm. 2008; 5:839–845.
7. Schoonderwoerd BA, Ausma J, Crijns HJ, Van Veldhuisen DJ, Blaauw EH, Van Gelder IC. Atrial ultrastructural changes during experimental atrial tachycardia depend on high ventricular rate. J Cardiovasc Electrophysiol. 2004; 15:1167–1174.
8. Hu YF, Chen YJ, Lin YJ, Chen SA. Inflammation and the pathogenesis of atrial fibrillation. Nat Rev Cardiol. 2015; 12:230–243.
9. Li D, Fareh S, Leung TK, Nattel S. Promotion of atrial fibrillation by heart failure in dogs: atrial remodeling of a different sort. Circulation. 1999; 100:87–95.
10. Bauer A, McDonald AD, Donahue JK. Pathophysiological findings in a model of persistent atrial fibrillation and severe congestive heart failure. Cardiovasc Res. 2004; 61:764–770.
11. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005; 18:1440–1463.
12. Sanfilippo AJ, Abascal VM, Sheehan M, et al. Atrial enlargement as a consequence of atrial fibrillation. A prospective echocardiographic study. Circulation. 1990; 82:792–797.
13. Schotten U, Ausma J, Stellbrink C, et al. Cellular mechanisms of depressed atrial contractility in patients with chronic atrial fibrillation. Circulation. 2001; 103:691–698.
14. Luong C, Thompson DJ, Bennett M, et al. Right atrial volume is superior to left atrial volume for prediction of atrial fibrillation recurrence after direct current cardioversion. Can J Cardiol. 2015; 31:29–35.
15. O'Neill MD, Jaïs P, Takahashi Y, et al. The stepwise ablation approach for chronic atrial fibrillation--evidence for a cumulative effect. J Interv Card Electrophysiol. 2006; 16:153–167.
16. Andrade JG, Khairy P, Verma A, et al. Early recurrence of atrial tachyarrhythmias following radiofrequency catheter ablation of atrial fibrillation. Pacing Clin Electrophysiol. 2012; 35:106–116.
17. European Heart Rhythm Association (EHRA). European Cardiac Arrhythmia Scoiety (ECAS). American College of Cardiology (ACC). . HRS/EHRA/ECAS expert Consensus Statement on catheter and surgical ablation of atrial fibrillation: recommendations for personnel, policy, procedures and follow-up. A report of the Heart Rhythm Society (HRS) Task Force on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2007; 4:816–861.
18. O'Donnell D, Furniss SS, Dunuwille A, Bourke JP. Delayed cure despite early recurrence after pulmonary vein isolation for atrial fibrillation. Am J Cardiol. 2003; 91:83–85.
19. Moon J, Hong YJ, Shim J, et al. Right atrial anatomical remodeling affects early outcomes of nonvalvular atrial fibrillation after radiofrequency ablation. Circ J. 2012; 76:860–867.
20. Arya A, Hindricks G, Sommer P, et al. Long-term results and the predictors of outcome of catheter ablation of atrial fibrillation using steerable sheath catheter navigation after single procedure in 674 patients. Europace. 2010; 12:173–180.
21. Jiang H, Lu Z, Lei H, Zhao D, Yang B, Huang C. Predictors of early recurrence and delayed cure after segmental pulmonary vein isolation for paroxysmal atrial fibrillation without structural heart disease. J Interv Card Electrophysiol. 2006; 15:157–163.
22. Lee SH, Tai CT, Hsieh MH, et al. Predictors of early and late recurrence of atrial fibrillation after catheter ablation of paroxysmal atrial fibrillation. J Interv Card Electrophysiol. 2004; 10:221–226.
23. Themistoclakis S, Schweikert RA, Saliba WI, et al. Clinical predictors and relationship between early and late atrial tachyarrhythmias after pulmonary vein antrum isolation. Heart Rhythm. 2008; 5:679–685.
24. Bhargava M, Di Biase L, Mohanty P, et al. Impact of type of atrial fibrillation and repeat catheter ablation on long-term freedom from atrial fibrillation: results from a multicenter study. Heart Rhythm. 2009; 6:1403–1412.
25. Verma A, Wazni OM, Marrouche NF, et al. Pre-existent left atrial scarring in patients undergoing pulmonary vein antrum isolation: an independent predictor of procedural failure. J Am Coll Cardiol. 2005; 45:285–292.
26. Pappone C, Santinelli V, Manguso F, et al. Pulmonary vein denervation enhances long-term benefit after circumferential ablation for paroxysmal atrial fibrillation. Circulation. 2004; 109:327–334.
27. Hof IE, Velthuis BK, Chaldoupi SM, et al. Pulmonary vein antrum isolation leads to a significant decrease of left atrial size. Europace. 2011; 13:371–375.
28. Akutsu Y, Kaneko K, Kodama Y, et al. Association between left and right atrial remodeling with atrial fibrillation recurrence after pulmonary vein catheter ablation in patients with paroxysmal atrial fibrillation: a pilot study. Circ Cardiovasc Imaging. 2011; 4:524–531.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download