Abstract
Background and Objectives
Both carotid intima-media thickness (CIMT) and carotid plaque are important factors in the primary prevention of cardiac disease. However, it is unclear which one is more important for prognosis, especially in patients with coronary artery disease (CAD).
Subjects and Methods
In total, 1426 consecutive CAD patients, proven by angiography, were followed-up for a mean of 85 months. The study population was divided into four groups depending on the CIMT (≥0.83 mm, >95 percentile in Korea) and the presence or absence of carotid plaque.
Results
Patients with carotid plaque and thick CIMT (n=237, 16.6%) had a higher prevalence of hypertension, diabetes mellitus, and dyslipidemia than those had plaque and thin CIMT (n=213, 14.9%), those without plaque and thick CIMT (n=265, 18.6%) and those without plaque and thin CIMT (n=711, 49.9%). The patients with carotid plaque and thick CIMT group had a higher cardiac mortality rate (20.7% vs. 13.1%, 9.4% and 3.9%, respectively, p<0.001) and higher major adverse cardiovascular events (MACE) including death, acute myocardial infarction, and stroke (27.8% vs. 18.8%, 15.5% and 9.3%, respectively, p<0.001) than any other groups. Multivariate Cox regression analysis showed that the presence of carotid plaque with thick CIMT had the highest hazard ratio (HR) compared to other groups (HR 2.23 vs. 1.81, 2.01) for cardiac mortality. Also, carotid plaque had a higher HR than CIMT for mortality (HR 1.56 vs. 1.37) and MACE (HR 1.54 vs. 1.36) in the total study population.
The measurement of carotid intima-media thickness (CIMT) and carotid plaque with B-mode ultrasound is a noninvasive, sensitive, and reproducible tool for identifying and quantifying subclinical vascular atherosclerosis and for evaluating the risk of cardiovascular disease.1)
It is widely recognized that the measurement of CIMT and carotid plaque with carotid ultrasound is not only related to cardiovascular risks such as age, diabetes, and hypertension (HTN), but also to the severity of cardiovascular disease.2)3)
Endothelial function, such as flow-mediated dilatation showed discordant results in some studies investigating its relationships with clinical aspects. These tests also showed varying outcomes depending on the patients' status, diet, and clinical conditions, leading to a limited range of applications in real clinical situations.4)5) On the other hand, carotid ultrasonography is advantageous because its measurements are sparsely affected by such factors as diet and clinical features, and is thus more reliable. Also, the recent advancement in measurement methods, moving from manual to automated measurement, reduced the errors in the measuring process, yielding results four times more accurate and contributing to the wide utilization of carotid ultrasonography in clinical situations presently.6)
Carotid intima-media thickness as well as the degree of coronary artery calcification is a widely used method for assessing patients' risks since the importance of primary prevention of CAD has been emphasized. In the process of carotid ultrasonography, the presence of carotid plaque is also recognized as an important prognostic factor, along with CIMT.7)8)9)10)11)
The Atherosclerosis Risk in Communities (ARIC) study showed that coronary heart disease and mortality risk prediction can be improved by adding CIMT and plaque information to traditional risk factors.12) In previous studies, assessment of carotid plaque, compared with the CIMT, had a higher diagnostic accuracy in the prediction of future CAD.7)8)11)13) Also, we previously reported that carotid plaque was a strong predictor of death and major adverse cardiovascular events (MACE) in patients with CAD.14)
However, most research focused on the role and clinical significance of carotid ultrasonography on primary prevention. Moreover, although the clinical significance of CIMT and carotid plaque has been recognized, simultaneous analysis of increased CIMT and the presence of carotid plaque has been reported limitedly in patients with CAD.
Carotid ultrasonographic findings have recently been proved to have meaningful effects on the secondary prevention of CAD,14)15) but the degree of influence of both CIMT and carotid plaque have on the prognosis of patients with CAD has not yet been studied. Therefore, the purpose of this study was to identify the impact of CIMT and the presence of carotid plaque, measured using carotid ultrasonography, on the long-term clinical prognosis of patients with CAD.
The study population consisted of 1654 consecutive patients who underwent carotid scanning and coronary angiograms (CAGs) from January 2000 to June 2007 in Konyang University Hospital CIMT Registry. We excluded 159 patients due to the following reasons; hemodynamic instability (n=21), poor carotid image quality (n=75), and lack of an evaluation of the presence of carotid plaque or CIMT (n=63). Patients who were lost to follow-up within 24 months (n=26) and who died from malignancy or infection (n=43), according to their medical records, were also excluded. Consequently, a total of 1426 consecutive patients (781 male, 54.8%; mean age of 64.7±10.1 years) with CAD, defined as ≥50% diameter stenosis by CAG, who underwent carotid scanning were enrolled. The demographic, clinical, and angiographic baseline data were collected by trained research technicians. The duration of patient follow-up was as follows: mean of 87 months for death, and 54 months for stroke and acute myocardial infarction (AMI).
The baseline evaluation included a complete history and physical examination including the following information: HTN (blood pressure ≥140/90 mm Hg, based on the average of repeated readings or patients on antihypertensive drugs), dyslipidemia (total cholesterol >200 mg/dL and/or triglycerides >150 mg/dL and/or low density lipoprotein cholesterol >130 mg/dL or patients on lipid-lowering therapy), diabetes mellitus (DM, controlled with diet, oral hypoglycemic agents, or insulin; or fasting glucose level ≥126 mg/dL or 2 hour oral glucose tolerance test ≥200 mg/dL), renal failure (creatinine ≥2.0 mg/dL), smoking habits (included former and current smokers), old myocardial infarction (MI) (previously documented AMI) and lower ejection fraction (EF ≤50% by echocardiography). Old age was defined as ≥60 years old.
Informed consent was obtained from each patient and the study was approved by our hospital ethics committee. The study protocol conforms to the ethical guidelines of the Declaration of Helsinki in 1975.
Coronary angiogram was performed to evaluate ischemic heart failure or non-cardiac preoperative risk (n=267) and ischemic heart disease {stable angina (n=769), unstable angina (n=153) or AMI (n=237)}. CAG was performed through either a femoral or radial artery using a standard technique. Significant coronary artery stenosis was defined as a ≥50% reduction of the internal diameter at major epicardial coronary arteries and side branches with a diameter ≥2.5 mm.
Before or within one day after the CAG, carotid artery scanning was performed with a high-resolution ultrasonographic unit (Hewlett-Packard Sonos-5500®, CA, USA), equipped with a 7.5 MHz linear array transducer. The subjects were assessed in a supine position. All ultrasonographic examinations were performed by one technician who was specialized, well trained, and blinded to the clinical and angiographic information of the study subjects. The CIMT was measured in 1 cm long segments just proximal to the carotid bulb in the common carotid artery using a semi-automatic technique with MATH® software (version 2.01; METRIS CO., Argenteuil, France). In the presence of plaque, the CIMT was measured at the segment without plaque. Carotid plaque was defined as a focal structure encroaching into the arterial lumen by at least 50% of the surrounding CIMT value,16) or with a thickness >1.2 mm.17)18) The bilateral common carotid arteries and bulbs were scanned to evaluate the presence or absence of plaque.
Carotid intima-media thickness was divided into two groups by the 95th percentile value (0.830 mm) of normal people with carotid IMT19) and thick CIMT was defined as >0.830 mm. Patients were divided into four groups according to CIMT and presence of carotid plaque (Group I: thin CIMT without carotid plaque, n=711, Group II: thick CIMT without carotid plaque, n=265, Group III: thin CIMT with carotid plaque, n=213, and Group IV: thick CIMT with carotid plaque, n=237).
Clinical follow-up was performed for at least 2 years (maximum: 120 months, mean: 87 months) and follow-up data was obtained from all patients.
Stroke and AMI events were documented by making phone calls to the patients (437 patients) and by reviewing hospital records (989 patients). Information regarding whether the patient expired was confirmed by the National Statistical Office. The primary outcome was all causes of death. The MACE were defined as the following: cardiac death, AMI, and stroke. Cardiac death was defined as death from pump failure, arrhythmia, or mechanical complications including ventricular septal rupture and free wall rupture. The definition of AMI included two among the following three criteria; prolonged chest pain for over 20 minutes, elevation of cardiac enzymes (creatinine kinase, creatine kinase-MB or the relative index) more than twice the upper limit of normal, and ST-T wave change or new Q waves on serial electrocardiography that were indicative of myocardial damage. Stroke was defined as a loss of neurological function caused by an ischemic event and this loss persisted for more than 24 hours or it left residual signs.
Differences in the continuous and categorical variables were evaluated through an analysis of variance test and chi-square test. The cumulative incidence of adverse events was estimated by the Kaplan-Meier method after stratifying subjects into four groups according to CIMT and presence of carotid plaque. The significance level was assessed by log-rank test.
The relationships between carotid plaque, CIMT, and cardiovascular events were tested by one variable Cox regression analysis. Multivariable Cox regression analysis was performed to evaluate the association between the clinical outcome and several parameters, including CIMT, carotid plaque, old age, gender, lower EF, DM, HTN, dyslipidemia, renal failure, smoking habits, acute coronary syndrome (ACS), and body mass index (BMI). All statistical tests were performed by using the Statistical Package for the Social Sciences (SPSS) program, version 18.0 (SPSS, Inc., Chicago, IL, USA) and a p of <0.05 was considered statistically significant.
Baseline characteristics of the four groups are listed in Table 1. Patients with carotid plaque and thick CIMT (group IV, n=237, 16.6%) were more likely to have HTN, DM, and multi-vessel diseases compared to those who had carotid plaque with thin CIMT (group III, n=213, 14.9%), who did not have plaque with thick CIMT (group II, n=265, 18.6%) and who did not have plaque with thin CIMT (group I, n=711, 49.9%).
The mean values of CIMT in groups I, II, III, and IV were 0.691±0.087 mm, 0.965±0.125 mm, 0.732±0.082 mm, and 1.033±0.164 mm, respectively. Groups I and II (those without plaque) had more medical treatment, whereas Group III and IV (those with carotid plaque) had more interventional treatment for CAD.
The average follow-up duration was 87 months (IQR 69-109) for death, and 54 months (IQR 36-72) for AMI, stroke, and MACE.
Patients with either carotid plaque or thick CIMT had higher MACE (23.6% vs. 10.9%, p<0.001, 21.3% vs. 11.5%, p<0.001) than those who did not have a carotid plaque or had thin CIMT. The patient group with thick CIMT and carotid plaque had the highest MACE rate (Group I: 9.3%, Group II: 15.1%, Group III: 18.8%, Group IV: 27.8%, p<0.001) (Table 2).
Univariate analysis showed that the hazard ratio (HR) of Groups II, III, and IV were 1.69 {95% confidence interval (CI) 1.14-2.51, p=0.001}, 2.30 (95% CI 1.55-3.40, p<0.001) and 3.79 (95% CI 2.69-5.33, p<0.001), respectively. Other significant predictors for death were: old age (HR 2.38, 95% CI 1.77-3.20, p<0.001), male gender (HR 1.62, 95% CI 1.22-2.14, p=0.001), lower EF (HR 3.76, 95% CI 2.41-5.85, p<0.001), renal failure (HR 2.73, 95% CI 1.35-5.55, p=0.005), smoking (HR 1.55, 95% CI 1.18-2.05, p=0.002), ACS (HR 2.20, 95% CI 1.67-2.89, p<0.001), and low BMI (HR 0.59, 95% CI 0.44-0.78, p<0.001).
Kaplan-Meier curve analysis showed that Group IV had the highest probability of future mortality, followed by patients with either thick CIMT or carotid plaque alone as illustrated in Fig. 1A. This means that patients with carotid plaque and thick CIMT have the highest probability of future MACE.
Multivariate analysis also showed that the HR of groups IV and III were significantly higher (HR 2.08, 95% CI 1.40-3.09, p<0.001 and HR 1.58, 95% CI 1.03-2.42, p=0.035, respectively) than Group I for MACE. Other factors, such as old age (HR 1.90, 95% CI 1.34-2.68, p<0.001), male gender (HR 1.61, 95% CI 1.14-2.27, p=0.007), lower EF (HR 2.49, 95% CI 1.54-4.04, p<0.001), renal failure (HR 3.05, 95% CI 1.45-6.42, p=0.003), ACS (HR 1.68, 95% CI 1.25-2.28, p=0.001), and low BMI (HR 0.68, 95% CI 0.51-0.91, p=0.011) were also independent predictors for MACE.
Patients with either carotid plaque or thick CIMT had a higher mortality rate than those who did not have carotid plaque or had thin CIMT (17.1% vs. 5.4%, p<0.001; 14.7% vs. 6.1%, p<0.001, respectively). Mortality was highest in Group IV, followed by Group III, Group II, and Group I (Group I: 3.9%, Group II: 9.4%, Group III: 13.1%, Group IV: 20.7%, p<0.001) (Table 2). Groups III and IV, who had carotid plaque, showed higher mortality rates than Groups I and II, who had no carotid plaque, regardless of CIMT. Univariate analysis showed that the HR of Group IV was highest (HR 5.31, 95% CI 3.33-8.45, p<0.001), followed by Group III (HR 3.43, 95% CI 2.03-5.80, p<0.001) and Group II (HR 2.27, 95% CI 1.32-3.90, p=0.003). The HR of carotid plaque was higher than those with thick CIMT (3.25, p<0.001 vs. 2.36, p<0.001, respectively). Other significant predictors for death were old age (HR 4.64, 95% CI 2.93-7.34, p<0.001), male gender (HR 1.43, 95% CI 1.00-2.04, p=0.05), lower EF (HR 5.94, 95% CI 3.65-9.67, p<0.001), renal failure (HR 5.13, 95% CI 2.51-10.49, p<0.001), DM (HR 1.80, 95% CI 1.26-2.58, p=0.001), and low BMI (HR 0.58, 95% CI 0.40-0.84, p=0.003).
The Kaplan-Meier curve analysis showed Group IV had the highest probability of future mortality, followed by patients with either thick CIMT or carotid plaque alone as illustrated in Fig. 1B and C shows the risks adjusted in Kaplan-Meier incidence curves, which demonstrate that the group with thick CIMT and existing carotid plaque had the highest mortality risk.
Multivariate analysis showed that Groups IV (HR 2.23, 95% CI 1.33-3.76, p=0.003), III (HR 2.01, 95% CI 1.45-3.52, p=0.015), and II (HR 1.81, 95% CI 1.02-3.21, p=0.042) all had significant higher HRs than Group I. The HR of carotid plaque was higher than those with thick CIMT (1.56, p=0.030 vs. 1.37, p=0.108). Other significant predictors for mortality by multivariate analysis were old age (HR 4.24, 95% CI: 2.51-7.15, p<0.001), male gender (HR 1.75, 95% CI 1.14-2.71, p=0.011), lower EF (HR 4.07, 95% CI 2.38-6.97, p<0.001), and renal failure (HR 6.01, 95% CI 2.74-13.17, p=0.003).
Patients with either carotid plaque or thick CIMT had higher stroke rates than those who did not have a carotid plaque or had thin CIMT (6.2% vs. 3.7%, p=0.032, 6.4% vs. 3.5%, p=0.011). The stroke rate was highest in Group IV (Group I: 3.19%, Group II: 5.3%, Group III: 4.7%, Group IV: 7.6%, p=0.030) (Table 2).
Univariate analysis showed that Group IV was a significant predictor (HR 2.70, 95% CI 1.45-5.05, p=0.002) for stroke. Old age (HR 2.21, 95% CI 1.30-3.76, p=0.003), HTN (HR 1.97, 95% CI 1.18-3.31, p=0.010), and ACS (HR 1.94, 95% CI 1.17-3.21, p=0.010) were also significant predictors for stroke. Kaplan-Meier curve analysis showed patients presenting with both thick CIMT and carotid plaque had the highest probability of future stroke, followed by patients with either thick CIMT or carotid plaque alone as illustrated in the Kaplan-Meier analysis shown in Fig. 1E.
However, multivariate analysis showed that there was no significant predictor for stroke among the parameters of carotid ultrasound findings. Thick CIMT with existing carotid plaque had the highest HR, but this result did not have statistical significance (Group II: HR 1.16, 95% CI 0.54-2.49, p=0.704, Group III: HR 1.15, 95% CI 0.51-2.60, p=0.738, Group IV: 1.61, 95% CI 0.79-3.30, p=0.190). The other significant predictor for stroke by multivariate analysis was HTN (HR 2.37, 95% CI 1.30-4.31, p=0.005).
The major finding of our study was that both CIMT and carotid plaque were important predictors for death and MACE, even after adjustment for cardiovascular risk factors, especially in patients with CAD. Secondly, carotid plaque had a higher HR than CIMT in this study group. This means that the presence of carotid plaque has more powerful prognostic significance than CIMT in this study group.
This result was in accordance with our previous study14) which evaluated the importance of carotid plaque only in CAD patients. But, the present study evaluated the significance of CIMT and carotid plaque's prognostic impact on MACE in the patient population. As a result, we examined CIMT in addition to the carotid plaque and divided our subjects into four groups. Ultimately, we found that thick CIMT with simultaneously existing carotid plaque was the most powerful independent predictor of mortality and MACE.
There are several cardiovascular risk stratification models: the Framingham risk score, the Systematic COronary Risk Evaluation project, and the Prospective Cardiovascular Munster Study that serve as useful methods for predicting the risk of future CAD.20)21)22) Battes et al.23) reported that old age, smoking, DM, cholesterol, BMI, old MI, heart failure, peripheral disease, revascularization, and previous stroke were independent predictors for mortality according to the cardiovascular risk assessment model in patients with established CAD. However, risk factor models for patients with known CAD are not well established.
Carotid ultrasound is the simplest, non-invasive imaging test and has been widely used as a surrogate marker of atherosclerotic disease1) and for established surrogate markers for CAD and MACE as well.8) Carotid ultrasound is also recommended for, and is used in, the screening test for CAD.24) However, measurement of the area or volume of plaque is generally considered to be a better predictor for the processing of atherosclerotic disease than CIMT.25) Furthermore, other studies demonstrated that carotid plaque, rather than CIMT, is a more accurate predictor of coronary events and is more closely related to CAD.7)11)26) The ARIC study reported that adding carotid plaque and CIMT to the traditional risk factors improved CAD risk prediction. However, the study population's heart disease was not confirmed by CAG.12)
Several studies revealed that carotid plaque and CIMT were also independent predictors of death and MI in patients with CAD.13)27)28) Our previous study also shown that carotid plaque is a more important predictor for MACE and mortality than CIMT in patients with CAD.14) The present study suggests that the presence of carotid plaque with thick CIMT was the most powerful predictor for mortality and MACE in patients with CAD; and coronary atherosclerosis was confirmed via CAG.
Carotid plaque and CIMT are well established independent predictors of stroke, and carotid plaque is known to be a more accurate surrogate than CIMT.29)30) In our study, carotid plaque or thick CIMT had higher incidence and prediction rates of stroke, but this was not statistically significant after being adjusted in multivariate analysis. Our study result with regards to stroke was different with the previous studies. This different result was possibly due to our study subjects, who had CAD confirmed by CAG, which was different to those of previous studies.29)30)
Although current guidelines do not recommend carotid ultrasonography in patients already diagnosed with CAD, our study results show the importance of the carotid scan. There was a higher MACE rate in patients with thick CIMT or those with carotid plaque than those with thin CIMT and/or without carotid plaque. Those patients who suffer from CAD require active efforts for secondary prevention if increased CIMT or carotid plaque has been discovered. According to our previous study, the presence of carotid plaque in patients with CAD was related with an increased cardiogenic mortality rate.14) However, most studies consistently reported the effects of carotid ultrasonographic results on MACE, especially in patients with HTN, DM, and old age, rather than in patients with CAD. Thus, current guidelines recommend the use of carotid ultrasonography only for the primary prevention of CAD, discouraging its use for patients without risk factors or those who already have confirmed CAD. In addition, follow-up carotid ultrasonography is not recommended and is considered a contraindication.
For patients who have the risk factors, carotid ultrasound can be utilized to assess the risk of cardiovascular adverse events along with coronary arterial calcium score, and further treatment steps, such as lipid lowering therapy or noninvasive cardiovascular tests, can be chosen depending on its results.
For patients without the risk factors, carotid ultrasonography may not be a useful examination method in real clinical conditions. However, for those patients already diagnosed with CAD, although carotid ultrasonographic results may not influence the treatment of the diseases itself, the results have shown to have a significant influence on the prognosis of these patients and have the potential to become a clinically significant means of examination.
In our study, there were other factors in addition to the carotid ultrasonographic results that influenced cardiovascular incidents, including a history of MI, poly-vascular diseases, ACS, and left ventricular dysfunction, but this result was in accordance with that of previous studies.
Another interesting consequence that we discovered was regarding the different prevalence rates of HTN and DM in each group. That is, HTN and DM were more prevalent with the presence of carotid plaque or increased CIMT and among these two factors, the presence of carotid plaque was associated with higher prevalence with HTN and DM. Both HTN and DM have previously been reported to have relationships with carotid ultrasonography, and the presence of each disease was reported to be more prevalent with thickened CIMT and existing carotid plaque.14) However, the fact that CIMT plays a role in the prevalence rate of such diseases is an interesting fact. Obviously, the duration of the disease or its severity will affect the difference, but was shown that the probability of HTN and DM increases with thickened CIMT and, especially, with the presence of carotid plaque.
Our study suggests that carotid plaque has more important prognostic power than CIMT in prognosis, especially in patients with CAD, although those two factors were significant prognostic predictors. Additionally, carotid scanning may be an important tool for secondary prevention purpose.
Our study had several limitations. The major limitation is that this study was single center registry cohort study. Although we performed adjustment analysis, unmeasured hidden biases may have remained. Secondly, we could not evaluate the impact of medical intervention on long-term clinical outcomes. Third, this study enrolled patients from 2000 to 2007 and defined carotid plaque as irregularly thickened part with 1.2 mm or thicker, but recently its definition has been altered to include a thickened part with 1.5 mm or thick or 50% thicker than its surroundings, and thus will require additional analysis. Fourth, initially we tried to seek cardiac death as a MACE, excluding the patients who died from infection and malignancy, but the death status in some patients was derived from the National Statistics Office without information for cause of death. Therefore, there is some chance of non-cardiac death in the cardiac death group. Finally, recent studies suggest that the morphologic abnormalities of carotid plaques, such as irregular surface, ulceration of the plaque, and hypoechoic characteristics are related to the rise in cardiovascular incidences. In this study, we focused primarily on the risk assessment of carotid plaque and intimamedia thickness on cardiovascular incidence rather than their morphology.
However, merits of this study include that large number of samples, prospective data collection, and confirmation of death via the National Statistical Office.
Figures and Tables
 | Fig. 1Kaplan-Meier survival curve (A, B, D, and E) and risk-adjusted Kaplan-Meier curve (C) after stratifying subjects into 4 groups according to CIMT and presence of carotid plaque during long-term follow-up. A and B: major adverse cardiovascular event (MACE) and death rate were significantly higher in patients with carotid plaque than those without carotid plaque and higher in those with thick CIMT than in those in the thin CIMT group. C: mortality risk was also highest in the thick CIMT with carotid plaque group followed by those with carotid plaque and thin CIMT, those without carotid plaque and thick CIMT, and those without carotid plaques and thin CIMT in risk-adjusted Kaplan-Meier curve analysis. D: acute myocardial infarction (AMI) rate showed no significant difference between the 4 groups. E: stroke rate was significantly higher in patients with thick CIMT and carotid plaque compared to those with thin CIMT and without carotid plaque. CIMT: carotid intima-media thickness. |
Table 1
Baseline characteristics

Values are mean±SD. Group I: thin CIMT without carotid plaque, Group II: thick CIMT without carotid plaque, Group III: thin CIMT with carotid plaque, Group IV: thick CIMT with carotid plaque. Thick CIMT: defined as >0.830. CIMT: carotid intima-media thickness, MI: myocardial infarction, ACS: acute coronary syndrome, BMI: body mass index, FBS: fasting blood sugar, TG: triglyceride, HDL-C: high density lipoprotein-cholesterol, LDL-C: low density lipoprotein-cholesterol, hs-CRP: high sensitivity C-reactive protein, CABG: coronary artery bypass graft
Table 2
Clinical outcomes by group
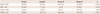
Table 3
Predictors for major adverse cardiovascular events by Cox regression analysis
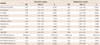
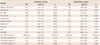
Table 4
Predictors for death by Cox regression analysis
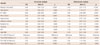
Table 5
Predictors for stroke by Cox regression analysis
References
1. Stein JH, Korcarz CE, Hurst RT, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force. Endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr. 2008; 21:93–111. quiz 189-90.
2. O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK Jr. Cardiovascular Health Study Collaborative Research Group. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med. 1999; 340:14–22.
3. Fathi R, Haluska B, Isbel N, Short L, Marwick TH. The relative importance of vascular structure and function in predicting cardiovascular events. J Am Coll Cardiol. 2004; 43:616–623.
4. Xu Y, Arora RC, Hiebert BM, et al. Non-invasive endothelial function testing and the risk of adverse outcomes: a systematic review and meta-analysis. Eur Heart J Cardiovasc Imaging. 2014; 15:736–746.
5. Corretti MC, Anderson TJ, Benjamin EJ, et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol. 2002; 39:257–265.
6. Bae JH, Kim WS, Rihal CS, Lerman A. Individual measurement and significance of carotid intima, media, and intima-media thickness by Bmode ultrasonographic image processing. Arterioscler Thromb Vasc Biol. 2006; 26:2380–2385.
7. Inaba Y, Chen JA, Bergmann SR. Carotid plaque, compared with carotid intima-media thickness, more accurately predicts coronary artery disease events: a meta-analysis. Atherosclerosis. 2012; 220:128–133.
8. Chambless LE, Heiss G, Folsom AR, et al. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987-1993. Am J Epidemiol. 1997; 146:483–494.
9. Chambless LE, Folsom AR, Clegg LX, et al. Carotid wall thickness is predictive of incident clinical stroke: the Atherosclerosis Risk in Communities (ARIC) study. Am J Epidemiol. 2000; 151:478–487.
10. Lorenz MW, von Kegler S, Steinmetz H, Markus HS, Sitzer M. Carotid intima-media thickening indicates a higher vascular risk across a wide age range: prospective data from the Carotid Atherosclerosis Progression Study (CAPS). Stroke. 2006; 37:87–92.
11. Simon A, Megnien JL, Chironi G. The value of carotid intima-media thickness for predicting cardiovascular risk. Arterioscler Thromb Vasc Biol. 2010; 30:182–185.
12. Nambi V, Chambless L, Folsom AR, et al. Carotid intima-media thickness and presence or absence of plaque improves prediction of coronary heart disease risk: the ARIC (Atherosclerosis Risk In Communities) study. J Am Coll Cardiol. 2010; 55:1600–1607.
13. Petersen C, Peçanha PB, Venneri L, Pasanisi E, Pratali L, Picano E. The impact of carotid plaque presence and morphology on mortality outcome in cardiological patients. Cardiovasc Ultrasound. 2006; 4:16.
14. Park HW, Kim WH, Kim KH, et al. Carotid plaque is associated with increased cardiac mortality in patients with coronary artery disease. Int J Cardiol. 2013; 166:658–663.
15. Hirano M, Nakamura T, Kitta Y, et al. Assessment of carotid plaque echolucency in addition to plaque size increases the predictive value of carotid ultrasound for coronary events in patients with coronary artery disease and mild carotid atherosclerosis. Atherosclerosis. 2010; 211:451–455.
16. Prati P, Vanuzzo D, Casaroli M, et al. Prevalence and determinants of carotid atherosclerosis in a general population. Stroke. 1992; 23:1705–1711.
17. Cho DK, Kwon SU, Kim SW, et al. Risk factors and predictors for the progression of carotid atherosclerotic stenosis in Korean adults. Korean Circ J. 2005; 35:834–840.
18. Ebrahim S, Papacosta O, Whincup P, et al. Carotid plaque, intima media thickness, cardiovascular risk factors, and prevalent cardiovascular disease in men and women: the British Regional Heart Study. Stroke. 1999; 30:841–850.
19. Lee SK, Hwang HY, Kim HS, et al. The carotid artery intima-media thickness measured with B-mode ultrasonography in adult volunteers. Korean Circ J. 1999; 29:1201–1211.
20. Conroy RM, Pyörälä K, Fitzgerald AP, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003; 24:987–1003.
21. Voss R, Cullen P, Schulte H, Assmann G. Prediction of risk of coronary events in middle-aged men in the Prospective Cardiovascular Münster Study (PROCAM) using neural networks. Int J Epidemiol. 2002; 31:1253–1262. discussion 1262-4.
22. Kannel WB, McGee D, Gordon T. A general cardiovascular risk profile: the Framingham Study. Am J Cardiol. 1976; 38:46–51.
23. Battes L, Barendse R, Steyerberg EW, et al. Development and validation of a cardiovascular risk assessment model in patients with established coronary artery disease. Am J Cardiol. 2013; 112:27–33.
24. Naghavi M, Falk E, Hecht HS, et al. From vulnerable plaque to vulnerable patient--Part III: Executive summary of the Screening for Heart Attack Prevention and Education (SHAPE) Task Force report. Am J Cardiol. 2006; 98(2A):2H–15H.
25. Finn AV, Kolodgie FD, Virmani R. Correlation between carotid intimal/medial thickness and atherosclerosis: a point of view from pathology. Arterioscler Thromb Vasc Biol. 2010; 30:177–181.
26. Brook RD, Bard RL, Patel S, et al. A negative carotid plaque area test is superior to other noninvasive atherosclerosis studies for reducing the likelihood of having underlying significant coronary artery disease. Arterioscler Thromb Vasc Biol. 2006; 26:656–662.
27. Held C, Hjemdahl P, Eriksson SV, Björkander I, Forslund L, Rehnqvist N. Prognostic implications of intima-media thickness and plaques in the carotid and femoral arteries in patients with stable angina pectoris. Eur Heart J. 2001; 22:62–72.
28. Komorovsky R, Desideri A, Coscarelli S, et al. Predictive value of associations between carotid and coronary artery disease in patients with acute coronary syndromes. Am J Cardiol. 2005; 95:116–119.
29. Kawai T, Ohishi M, Takeya Y, et al. Carotid plaque score and intima media thickness as predictors of stroke and mortality in hypertensive patients. Hypertens Res. 2013; 36:902–909.
30. Wannarong T, Parraga G, Buchanan D, et al. Progression of carotid plaque volume predicts cardiovascular events. Stroke. 2013; 44:1859–1865.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download