Abstract
Background and Objectives
Cigarette smoking has been recognized as a prominent threat to women's health. We investigated the impact of smoking on clinical outcomes in Korean female patients after acute myocardial infarction (AMI).
Subjects and Methods
Out of the AMI patients who enrolled in the Korea AMI Registry, 4444 female patients were included in this study. Patients were divided into two groups-non-smoker and smoker-according to their current smoking status. We compared in-hospital mortality and major adverse cardiac events (MACE), including cardiac death, myocardial infarction, repeated percutaneous coronary intervention (PCI), or coronary artery bypass grafting during the one-year clinical follow-up period between two groups.
Results
The non-smoker group had more hypertension (HTN) and diabetes mellitus. The levels of total cholesterol, triglyceride, and low-density lipoprotein cholesterol were higher in the non-smoker group. However, in-hospital mortality was significantly higher in the smoker group (1.0% vs. 2.4%, p=0.002), and cardiac death during the 12-month clinical follow-up was significantly more frequent in the smoker group (2.2% vs. 4.5%, p=0.003). Total MACEs during the 12 months were higher in the smoker group (4.9% vs. 6.8%, p=0.014). Smoking and HTN were independent predictors of MACE {odds ratio (OR): 1.742, 95% confidence interval (CI): 1.010-3.000, p=0.046; OR: 1.573, 95% CI: 1.003-2.466, p=0.049, respectively}.
Ischemic heart disease is the second leading cause of death in Korea,1) and smoking has been recognized as a major risk factor.2) Within the past two or three decades, female smoking habits have become similar to those of males. The steep rise in prevalence of smoking among women is expected to continue, while the prevalence of smoking among men is expected to decrease. Systematic review and meta-analysis found that, compared with non-smokers, female smokers have a 25% greater risk of coronary heart disease than male smokers.3)
The data for men and women may be different but recent work underscores the importance of smoking as a cause of myocardial infarction in both genders.4) As an example, in a Norwegian study, the acute myocardial infarction (AMI) incidence was 4.6 times higher among men. The incidence was increased six-fold in women and threefold in men who smoked at least 20 cigarettes per day compared with never-smokers, and the rate in female heavy smokers exceeded that of never-smoking men.5) Danish investigators reported that the relative risks suggest that women may be more sensitive than men to some of the deleterious effects of smoking.3) Until now, there have been few reports regarding clinical outcomes in female smokers with AMI.6)7)
The authors investigated the impact of smoking on the long-term outcomes in female Korean patients after AMI.
The Korea Acute Myocardial Infarction Registry (KAMIR) is a Korean prospective multicenter online registry designed to describe characteristics and clinical outcomes of Korean patients with AMI and to reflect current practice of management in Korea.8) The registry includes 52 community and university hospitals for primary percutaneous coronary intervention (PCI), and 4444 female patients were enrolled from 2005 to 2011. Data was collected at each site by an experienced study coordinator based on a standardized protocol. The study protocol was approved by the ethics committee at each participating institution.
From November 2005 to December 2011, a total of 4444 female patients with AMI patients were enrolled from the KAMIR. Patients were divided into two groups according to cigarette smoking status; 3819 patients were non-smokers, and 625 patients had smoked or currently were smokers. The latter group covered people who had smoked at least one hundred cigarettes during the course of her life.
Acute myocardial infarction was defined by clinical signs or symptoms, increased cardiac biomarkers {creatine kinase-MB (CK-MB), troponin-I or troponin-T}, and 12-lead electrocardiographic findings. Non-ST segment elevation myocardial infarction (STEMI) was defined as troponin-I levels elevated above 0.05 (units) without an elevated ST segment. We considered "smoker" to represent people who have ever smoked 100 cigarettes in their lifetime, including those who currently smoke and those who used to do so. "Past smoker" means individuals that who previously smoked at least 100 cigarettes in their lifetime, but they do not smoke currently. Left ventricular ejection fraction (LVEF) was checked using 2-dimensional echocardiography. The morphology of the lesion was examined using coronary angiography and was classified using criteria established by the American College of Cardiology/American Heart Association.9) The degree of coronary flow was classified by the Thrombolysis in Myocardial Infarction (TIMI) flow grade.10)
Clinical follow-up was performed 12 months after the commencement of the study. Major adverse cardiac events (MACE) included cardiac death, myocardial infarction (MI), repeated PCI, and coronary artery bypass grafting. Repeated PCI included target lesion revascularization (TLR) and target vessel revascularization (TVR). TLR was defined as a repeat intervention in the stent or within 5 mm proximal or distal to the stent. TVR was defined as a repeat intervention in the same vessel, more than 5 mm from the stent.
All analyses were performed by using Statistical Package for the Social Sciences (SPSS) for Windows, version 19.0 (SPSS Inc., Chicago, IL, USA). Continuous variables are presented as means±standard deviations and were compared with unpaired Student's t-tests. Discrete variables are expressed as percentages and frequencies and were compared by chi-square statistics. All statistical tests were 2-tailed with statistical significance defined as a p≤0.05. To identify the predictors of MACE, a multivariate analysis was performed using the logistic regression model. Included variables were age, body mass index (BMI), history of hypertension (HTN), history of diabetes mellitus (DM), history of dyslipidemia, history of coronary artery disease, symptoms at arrival, systolic blood pressure (SBP), left main complex lesion, multivessel disease, achievement of post TIMI flow, and STEMI patients. The results are presented as estimated odds ratios (ORs) with 95% confidence intervals (CIs) and p.
In comparing the clinical characteristics of the two groups, there was a difference in BMI, HTN, and DM. The average BMI was higher in the non-smoker group (23.7±3.3 vs. 23.4±3.5, p=0.033). The non-smoker group also had more patients with HTN and DM (63.5% vs. 52.8%, p<0.001; 34.0% vs. 26.9%, p=0.100, respectively). Hyperlipidemia, familial history and previous history of ischemic heart disease, and SBP were not significantly different between the groups. Symptoms of chest pain and dyspnea at arrival were more frequent in the smoker group (80.2% vs. 72.8%, p<0.001; 29.9% vs. 25.6%, p=0.022, respectively) (Table 1).
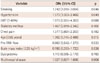
The LVEF measured by 2-dimentional echocardiogram and the total wall motion score were not significantly different. However, the levels of CK-MB (109.0±246.6 vs. 52.6±138.7, p<0.001), troponin-I (41.0±174.7 vs. 17.2±40.6, p<0.001), total cholesterol (190.0±46.6 vs. 177.8±44.3, p<0.001), triglycerides (123.3±90.8 vs. 109.0±60.3, <0.001), and low density lipoprotein-cholesterol (LDL-C) (121.8±40.9 vs. 111.9±48.2, p<0.001) were higher in the non-smoker group. On the other hand, level of high density lipoprotein-cholesterol (HDL-C) and high sensitivity C-reactive protein were not different between the two groups. Pro-brain natriuretic peptide was higher in the smoker group (3423.1±6624.8 vs. 5645±9091.1, p<0.001) (Table 2).
Multi vessel disease was found more frequently in the non-smoker group (57.4% vs. 52.1%, p=0.019), while the target vessel was similar between the two groups. The most common target vessel was the left anterior descending artery in both groups. Pre-TIMI flow had no significant difference between the groups (p=0.631) (Table 3).
The in-hospital mortality was significantly higher in the smoker group (1.0% vs. 2.4%, p=0.002), and cardiac death during the 12 months of clinical follow-up was significantly higher in the smoker group (4.5% vs. 2.2%, p=0.001). Total MACEs during 12 months were also higher in the smoker group (6.8% vs. 4.9%, p=0.014) (Table 4).
Multivariate logistic regression analysis was performed to identify the predictors of MACEs. Smoking and HTN were independent predictors of MACEs. In the smoking group, the MACE risk was 1.742 times that of the non-smoking group (p=0.046) (Table 5).
This is the first large clinical outcome analysis of Korean female smokers with AMI. In this analysis, female smokers with AMI showed higher in-hospital mortality rates and MACE rates during the one-year clinical follow-up period. Therefore, the prevalence of female smoking should be closely monitored in the Korean population.
Among the clinical characteristics of female AMI smoking patients, age was higher in the past smoker group than both the current smoker and the non-smoker groups. Lipid profiles, total cholesterol, triglycerides, and LDL-C were higher in the current smoker group, while multi vessel disease was higher in the non-smoker group. In spite of lower incidences of coronary artery disease risk factors, such as HTN and DM, female smoker patients, both current and former, with AMI showed higher in-hospital mortality rates and 12 month MACEs during the long-term clinical follow-up period. In multivariate logistic regression analysis, smoking had OR was 1.742 times (1.010-3.004) (p=0.046) higher than HTN and DM. We cautiously assume that smoking is most powerful risk factor. Viewed from another angle, non-smokers tended to be older, so they had a greater prevalence of HTN and DM due to their age. Also, non-smokers had a higher prevalence of chronic disease. So, they may be more concerned about their health, which may influence their smoking habits. They have more contact with healthcare providers and hospitals, which may also have some influence. Our study also had limitations, which could affect the results.
According to an epidemiologic study of Korean patients admitted for coronary angiography, younger Korean patients have different demographic findings than older patients: the higher prevalence of smoking and obesity are important risk factors in younger patients.11) Recent research has shown the importance of smoking as a cause of MI in both genders, especially in females. Shiraki and Saito7) showed a multivariate logistic regression model that revealed that gender differences affect in-hospital mortality. Grundtvig et al.12) reported that smoking is more detrimental in females than in men. In the years of 1998-2005, 2281 patients (36.8% female) were discharged. During follow-up, 55% of the patients died. Non-smokers, past smokers, and current smokers lost 5.4, 6.4, and 10.3 years of life, respectively. Female current smokers lost 1.9 years more than male current smokers (p<0.001). More years of life were lost among smoking women than among smoking men, indicating that smoking is most detrimental in the female gender.
Also, Wijnbergen et al.13) reported that women have higher rates of both MACEs and mortality after PCI compared to men. By multivariate analysis after adjusting for age and baseline characteristics, HTN, smoking, DM, stent diameter, and the time between onset of symptoms and arrival of the ambulance, the study showed similar MACE and mortality rates in men and women. However, smoking is one of the predictive factors influencing MACE and mortality in both genders. In a prospective study including both men and women aged 35-52 years, it was been demonstrated that the incidence of myocardial infarction increased 6-fold in women and 3-fold in men who smoked at least 20 cigarettes per day, compared to those who never smoked. In addition, current smoking was identified as a stronger risk factor in women than in men (relative risk 3.3 vs. 1.9) and smoking-related gender differences were more pronounced when considering women under 45 years of age.5)
Our results are in accordance with the Copenhagen City Heart Study, in which the relative risk of a first myocardial infarction in smokers was 9.4 in women and 2.9 in men with respect to non-smokers and the risk increased by 2-3% for each gram of tobacco smoked.14)
Tverdal et al.15) studied the mortality for different causes in relation to smoking history in men and women aged 35-49 who were followed for 13.3 years. They found that the relative risk of coronary death per ten cigarettes per day was 1.8 in women and 1.2 in men.
Smoking significantly affects the in-hospital mortality and MACE in female Korean MI patients. Of the Korean AMI patients who underwent PCI, their mortality rate was significantly higher in current smokers than in past smokers after PCI.16) Therefore, clinical efforts for smoking cessation may be very important even after successful PCI in Korea.
According to a Korean smoking analysis from July 2011, the male smoking rate has been slowly decreasing since 1998, but female smoking rate has not changed significantly (remaining at about 6.8%). Therefore, the smoking rate should be decreased in Korean females to prevent MI. It is important that smoking is not only a risk factor of MI but also a factor in the increasing mortality rate after survival from AMI. National surveillance and routine screening of the smoking female population will be effective for the primary and secondary prevention of development of ischemic heart disease, especially AMI. In Korea, adherence to preventive guidelines among smokers after AMI is relatively low.17) Only 52% of the AMI patients stopped smoking at one year after a heart attack. This finding underscores the need for an effective patient education system and program for smoking cessation.
Kim et al.18) analyzed clinical pattern changes in elderly Korean patients who underwent PCI between 1999 and 2009. The prevalence of HTN increased over time, but smoking decreased. Predictive factors of MACEs were female gender, smoking, old age, DM, and low thombolysis in myocardial infarction flow. Choi et al.19) observed the relationship between restenosis and compliance with self-care among acute coronary syndrome patients undergoing follow-up coronary angiograms. Patients who continued to smoke showed a stronger tendency for lower compliance with self-care and lifestyle modification. Choi et al.20) reported predictive factors for long-term clinical outcomes in 1162 patients with variant angina between 1996 and 2011. A history of smoking was the only independent risk factor for MACEs during long-term clinical follow-up in Korean patents with variant angina.
In female patients, early menopause increases the risk of MI.21) Further research using menopause status should be performed. After MI, current smokers who quit smoking may have different mortality rates from those that continue smoking. So, further research about smoking cessation's influence on mortality rate after MI, should be carried out in AMI patients.
This is the first study regarding female smoking in AMI patients based on KAMIR data. However, several limitations of this study exist. First, smoking history was self-reported by patients, so there may be inaccuracies. Second, long-term follow-up data was not acquired in this registry. If more follow-up data was collected, it would be helpful in identifying the multivariate comparison of survival curves by Cox proportional hazards model. Third, the exact manner of smoking habits or duration was not obtained in all patients due to registry data. Fourth, the initial study population was 4444 peoples, but not all patients were not included in the one-year period. So, there were limitations due to missing patients.
The in-hospital and 1-year mortality rates of this study were very low compared to previous reports. As coronary heart disease increases, there has been more education and publicity supplied material, in addition to increased media reports. Nowadays, there is a heightened awareness of coronary heart disease, so it may reduce the time one waits to go to the to hospital. Our hospital is trying to cut the door-to-balloon time, which may explain the results, in part.
In conclusion, female smokers with AMI showed higher in-hospital mortality rates and MACE rates during the one-year clinical follow-up period.
Figures and Tables
Table 1
Baseline clinical characteristics

Table 2
Echocardiographic and laboratory findings

Table 3
Coronary angiographic findings

Table 4
In-hospital mortality and MACE during one-year clinical follow-up
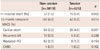
Table 5
Predictors of MACE according to multivariate logistic regression analysis
Acknowledgments
This study was supported by grants of The Korean Society of Cardiology, The Korea Centers for Disease Control and Prevention (2013-E63005-01), and The Korean Health Technology R&D Project (HI13C1527), Ministry of Health & Welfare, Republic of Korea.
References
1. Statistics Korea. 2012 Death Statistics. Daejeon: Statistics Korea;2012.
2. Jang SY, Ju EY, Cho SI, Lee SW, Kim DK. Comparison of cardiovascular risk factors for peripheral artery disease and coronary artery disease in the Korean population. Korean Circ J. 2013; 43:316–328.
3. Prescott E, Osler M, Andersen PK, et al. Mortality in women and men in relation to smoking. Int J Epidemiol. 1998; 27:27–32.
4. Lee JH, Lee H, Bae MH, et al. Gender differences among Korean patients with coronary spasm. Korean Circ J. 2009; 39:423–427.
5. Njølstad I, Arnesen E, Lund-Larsen PG. Smoking, serum lipids, blood pressure, and sex differences in myocardial infarction. A 12-year follow-up of the Finnmark Study. Circulation. 1996; 93:450–456.
6. Nauta ST, Deckers JW, van Domburg RT, Akkerhuis KM. Sex-related trends in mortality in hospitalized men and women after myocardial infarction between 1985 and 2008: equal benefit for women and men. Circulation. 2012; 126:2184–2189.
7. Shiraki T, Saito D. Sex difference of in-hospital mortality in patients with acute myocardial infarction. Acta Med Okayama. 2011; 65:307–314.
8. Sim DS, Jeong MH, Cho KH, et al. Effect of early statin treatment in patients with cardiogenic shock complicating acute myocardial infarction. Korean Circ J. 2013; 43:100–109.
9. Ellis SG, Vandormael MG, Cowley MJ, et al. Coronary morphologic and clinical determinants of procedural outcome with angioplasty for multivessel coronary disease. Implications for patient selection. Multivessel Angioplasty Prognosis Study Group. Circulation. 1990; 82:1193–1202.
10. TIMI Study Group. The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase I findings. N Engl J Med. 1985; 312:932–936.
11. Park JS, Lee HJ, Kim YJ, et al. The epidemiological and clinical characteristics of patients admitted for coronary angiography to evaluate ischemic heart disease. Korean J Intern Med. 2007; 22:87–92.
12. Grundtvig M, Hagen TP, Amrud ES, Reikvam A. Reduced life expectancy after an incident hospital diagnosis of acute myocardial infarction-effects of smoking in women and men. Int J Cardiol. 2013; 167:2792–2797.
13. Wijnbergen I, Tijssen J, van't Veer M, Michels R, Pijls NH. Gender differences in long-term outcome after primary percutaneous intervention for ST-segment elevation myocardial infarction. Catheter Cardiovasc Interv. 2013; 82:379–384.
14. Nyboe J, Jensen G, Appleyard M, Schnohr P. Smoking and the risk of first acute myocardial infarction. Am Heart J. 1991; 122:438–447.
15. Tverdal A, Thelle D, Stensvold I, Leren P, Bjartveit K. Mortality in relation to smoking history: 13 years' follow-up of 68,000 Norwegian men and women 35-49 years. J Clin Epidemiol. 1993; 46:475–487.
16. Seol SY, Lee SJ, Jeong MH, et al. Clinical outcomes of persistent smoking in patients with acute myocardial infarction who underwent percutaneous coronary intervention. Korean J Med. 2011; 80:562–570.
17. Choi YJ, Park JS, Kim U, et al. Changes in smoking behavior and adherence to preventive guidelines among smokers after a heart attack. J Geriatr Cardiol. 2013; 10:146–150.
18. Kim MS, Jeong MH, Hwang SH, et al. Clinical pattern changes in elderly patients who underwent percutaneous coronary intervention in the last ten years. Korean J Med. 2010; 79:661–672.
19. Choi MJ, Jeong MH, Hwang SY. Restenosis and compliance with self-care among acute coronary syndrome patients undergoing follow-up angiograms. Korean J Health Promot. 2011; 11:34–41.
20. Choi MJ, Jeong MH, Cho JY, et al. Predictive factors for long-term clinical outcomes in patients with variant angina. Korean J Med. 2013; 84:522–530.
21. Rosenberg L, Hennekens CH, Rosner B, Belanger C, Rothman KJ, Speizer FE. Early menopause and the risk of myocardial infarction. Am J Obstet Gynecol. 1981; 139:47–51.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download