Abstract
Figures and Tables
Fig. 1
Twelve-lead electrocardiography. The electrocardiography shows premature ventricular complexes and RSr' pattern in V 1.
Fig. 2
Chest X-ray on admission. A chest X-ray radiography showed no pulmonary lesion and no cardiomegaly (cardio-thoracic ratio was 48%).

Fig. 3
Intracardiac echocardiography. A: an ICE showed an underestimated large ASD. B: the Doppler imaging showed a left-to-right shunt through an ASD. C: however, a bidirectional shunt occurred with Valsalva maneuver. ICE: intracardiac echocardiography, ASD: atrial septal defect, LA: left atrium, RA: right atrium.
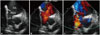
Fig. 4
A large ASD was treated with Amplatzer® (St. Jude Medical) septal occluder. A large ASD was measured by the balloon occlusion method (A) and successfully treated with 36-mm sized Amplatzer® (St. Jude Medical) septal occluder (B). Her symptoms were resolved immediately after the procedure. ASD: atrial septal defect.

Table 1
Results of cardiac catheterization
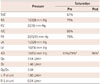
RA, PA and LA data were expressed as a wave/v wave/mean pressure. *The patients' arteial oxygen saturation was decreased from 93% while in supine position to 79% while at a 15° sitting position, †The arterial oxygen saturation after closure was also improved to 96%. To avoid complications, positional change was not perfomed. AO, RV and LV data were expressed as systolic/end-diastolic pressure. SVC: superior vena cava, RA: right atrium, RV: right ventricle, IVC: inferior vena cava, PA: pulmonary artery, LA: left atrium, LV: left ventricle, AO: aorta, Qp: pulmonary blood flow, Qs: systemic blood flow, L-R: left to right, R-L: right to left




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download