Abstract
Background and Objectives
Increased bleeding rates with standard dose prasugrel have led to increased questions about the effectiveness and safety of the lower maintenance dose. We compared platelet inhibitory efficacy between low dose prasugrel and standard dose clopidogrel in patients on maintenance dose dual antiplatelet therapy.
Subjects and Methods
Forty-three patients who underwent percutaneous coronary intervention were randomized to receive 75 mg clopidogrel (n=23) or 5 mg prasugrel (n=20). Another 20 patients were allocated to 10 mg prasugrel as a reference comparison group. All patients (weight, ≥60 kg; age, <75 years) had been receiving 100 mg aspirin and 75 mg clopidogrel daily. The platelet function test was performed at baseline and 30 days after randomization. The primary endpoint was P2Y12 reaction unit (PRU) at 30 days between 5 mg prasugrel and 75 mg clopidogrel.
Results
No differences in baseline PRU values were observed among the three groups. The prasugrel (5 mg) group had a significantly lower PRU value compared with that of 75 mg clopidogrel (174.6±60.2 vs. 223.4±72.9, p=0.022) group at 30 days, whereas the 10 mg prasugrel group showed a lower PRU value (71.9±34.4) compared with that of the 5 mg prasugrel (p<0.001). The rate of high on-treatment platelet reactivity (PRU >235) was significant lower in the 5 mg prasugrel group than that in the 75 mg clopidogrel group (15.0% vs. 56.5%, p=0.010).
Dual antiplatelet therapy with aspirin and P2Y12 receptor blockers is recommended for reducing ischemic events in patients with acute coronary syndrome (ACS) who are undergoing percutaneous coronary intervention (PCI).1)2) However, many studies have demonstrated wide inter-individual variability in the platelet response to clopidogrel.3)4) High on-treatment platelet reactivity (HTPR) after receiving clopidogrel has been associated with an increased risk for adverse cardiovascular events in patients who underwent PCI.5)6)7)8)
Prasugrel is a novel thienopyridine adenosine diphosphate (ADP)-receptor antagonist that has been shown to produce higher, more rapid and more consistent levels of platelet inhibition than standard and higher doses of clopidogrel due to the more efficient generation of active metabolite.9)10)11)12) The potent pharmacodynamic effect on platelet aggregation has resulted in improved ischemic outcomes but more bleeding compared with clopidogrel in patients with ACS who underwent PCI.13) Increased bleeding tendency with standard dose prasugrel has led to increased questions about its effectiveness and safety at lower maintenance doses. A previous pharmacodynamic study showed that 5 mg prasugrel was not inferior to 10 mg prasugrel in patients ≥75 years old or weighing <60 kg, in which the lower dose prasugrel was considered to reduce the rate of hemorrhagic complications.14)15) However, pharmacodynamic effects of 5 mg prasugrel in heavier weight and younger patients who underwent percutaneous coronary stent implantation are unknown. Therefore, we compared the platelet inhibitory efficacy determined by the VerifyNow P2Y12 (Accumetrics, San Diego, CA, USA) point-of-care assay between 5 mg prasugrel and 75 mg clopidogrel in nonlow body weight and non-elderly patients in the maintenance phase of dual antiplatelet therapy after percutaneous coronary stent implantation.
This study was a prospective, open-label, randomized, controlled trial conducted to compare platelet inhibitory efficacy between 5 mg prasugrel and 75 mg clopidogrel in patients in the maintenance phase of dual antiplatelet therapy after percutaneous coronary stent implantation. Patients were considered eligible for this study if they were 18-74-years-of-age, ≥60 kg of body weight and were receiving dual antiplatelet therapy with aspirin and clopidogrel for at least 12 months. The main exclusion criteria were as follows: a history of ischemic or hemorrhagic stroke, a history of transient ischemic attack, body weight <60 kg, age ≥75 years, use of oral anticoagulants or NSAIDs, presence of active bleeding or bleeding diathesis, serum creatinine >2 mg/dL, platelet count ≤100000/mm3, serum liver enzymes greater than twice the upper limit of normal values, and clinical instability. Written consent was obtained from each subject, and this study was approved by the local institutional review board and was in accordance with the provisions of the Declaration of Helsinki.
The study design and patient disposition are illustrated in Fig. 1. After assessing adherence to aspirin and clopidogrel therapy at the outpatient clinic to identify a steady-state level of pharmacodynamic effects, all subjects were randomly assigned to one of the following three groups: 75 mg clopidogrel, 5 mg prasugrel, or 10 mg prasugrel. Prasugrel (10 mg) was used as a reference for comparison. All subjects received the assigned drug without a loading dose and 100 mg aspirin once daily for 30 days.
Samples for the platelet function test were collected at baseline and 30 days after randomization. Blood samples were taken through a short venous catheter inserted into a forearm vein after assessing compliance to the allocated antiplatelet drugs and were processed for platelet function test within 60 minutes after the draw. Platelet function was assessed using the VerifyNow P2Y12 assay (Accumetrics), which is a turbidimetry-based optical detection device that measures responsiveness to clopidogrel, prasugrel, and other platelet ADP P2Y12 receptor antagonists. Results are expressed in P2Y12 reaction units (PRU), determined by the measurement of platelet aggregation in response to ADP, BASE, and percent inhibition.16) The percent platelet inhibition is calculated as: {(BASE-PRU)/BASE}×100.
The primary endpoint was PRU values between the 75 mg clopidogrel and 5 mg prasugrel groups 30 days after randomization. The secondary endpoints included the percent change in the PRU calculated as the relative difference in PRUs at baseline and at 30 days: {(PRU at baseline-PRU at 30 days)/(PRU at baseline)}×100, the rates of HTPR defined as >235 PRU, and percent platelet inhibition.17)18) Safety regarding bleeding events was also assessed based on the incidence of adverse events, signs and symptoms, laboratory data, and vital signs. Bleeding was classified as major, minor, or insignificant according to the Thrombolysis in Myocardial Infarction (TIMI) criteria.13)
We previously performed a pilot study to compare PRU values between 5 mg prasugrel and 75 mg clopidogrel in 20 patients who were <75 years and weighed ≥60 kg. PRU values were 171.6±52.1 and 208±87.6 in the 5 mg prasugrel and 75 mg clopidogrel groups, respectively. We hypothesized that 5 mg prasugrel would result in a reduction of 37 PRU compared with 75 mg clopidogrel with a difference of the standard deviation between the two groups to be 35. Therefore, considering a dropout rate of approximately of 10%, 20 patients in each group were needed to provide at least a 90% power to detect significant differences between treatment groups with a two-tailed alpha value <0.05. Continuous variables are presented as means±standard deviations. Categorical variables are presented as frequencies and group percentages. Analysis of variance or the Kruskal-Wallis test was used for comparing baseline continuous variables among the three groups. Student's t-test or the Mann-Whitney U-test was used for comparing continuous variable between two groups 30 days after randomization. Fisher's exact test was used to compare categorical variables. All statistical tests were two-tailed and a p<0.05 was considered significant. All calculations were performed using Statistical Package for the Social Sciences 14 (SPSS Inc., Chicago, IL, USA).
From June 2012 to August 2012, 75 patients were screened and 68 patients were enrolled in the study. Of these, 63 patients (23 patients on 75 mg clopidogrel, 20 patients each on 5 mg and 10 mg prasugrel) completed the study and were included in the pharmacodynamic analysis to assess the study endpoints. The patient's baseline clinical characteristics and medication 30 days after randomization are shown in Table 1 and 2, respectively. No significant differences were observed in the baseline characteristics among the three groups.
Baseline PRU values and percent platelet inhibition were not different among the three groups. At 30 days after randomization, the 5 mg prasugrel group had significantly lower PRU value compared with that of the 75 mg clopidogrel group (174.6±60.2 vs. 223.4±72.9, p=0.022), whereas the 10 mg prasugrel group showed a lower PRU value (71.9±34.4) compared with that of the 5 mg prasugrel group (p<0.001) (Fig. 2). Similarly, the 5 mg prasugrel group demonstrated a higher percent platelet inhibition compared to that of the 75 mg clopidogrel group at 30 days (Table 3). In addition, the percent change in the PURs was significantly higher in the 5 mg prasugrel than that in the 75 mg clopidogrel group (18.7±20.8 vs. -1.17±18.9, p=0.002) and higher in the 10 mg prasugrel (61.7±20.5) than that in the 5 mg prasugrel group (p<0.001). The proportion of baseline HTPR was similar in each group (p=0.392). At 30 days after switching to the study drugs, the rate of HTPR was significantly lower in the 5 mg prasugrel than that in the 75 mg clopidogrel group 15.0% vs. 56.5%, p=0.010) (Fig. 3). When we used a more sensitive PRU cut-off value (>208) predicting ischemic events, there were still differences in the rate of HTPR (30.0% vs. 60.9%) although statistical significance was borderline (p=0.067).
Thrombolysis in Myocardial Infarction major bleeding or life threatening bleeding events did not occur during the study period in any of the treatment groups. Three insignificant bleeding events occurred, including two episodes of recurrent bruising and one episode of epistaxis in the 10 mg prasugrel group. An episode of self-limiting bruising was also observed in the 75 mg clopidogrel and 5 mg prasugrel groups. One patient experience headache on 5 mg prasugrel and discontinued the drug. The other adverse events were mild or not considered to be related to the study drug.
The present randomized study is the first to assess the platelet inhibitory efficacy of a lower maintenance dose (5 mg daily) of prasugrel compared with a standard dose of clopidogrel and 10 mg prasugrel in patients <75 years and ≥60 kg who underwent PCI. The results of our trial demonstrated that the 5 mg prasugrel dose provided stronger platelet inhibition than that of 75 mg clopidogrel in this cohort of patients in the maintenance phase with aspirin and clopidogrel after PCI. Furthermore, the rate of HTPR, defined as a PRU value >235, was significantly lower in patients treated with 5 mg prasugrel compared with those treated with 75 mg clopidogrel; however, no significant TIMI bleeding was observed in patients who received 5 mg prasugrel or 75 mg clopidogrel.
Prasugrel has a more potent, rapid, and consistent antiplatelet effect than that of clopidogrel, although both drugs have similar binding affinities to the P2Y12 receptor, it is associated with more efficient generation of active metabolites.9)10)11)12) The stronger antiplatelet effect of 10 mg prasugrel provides the clinical benefit of reducing ischemic events but more bleeding events occur compared with that of 75 mg clopidogrel in ACS patients undergoing PCI.13) In contrast, 10 mg prasugrel does not significantly reduce the frequency of major ischemic events compared with 75 mg clopidogrel in patients with ACS without revascularization.19) In addition, the high platelet reactivity of clopidogrel was inversely related to bleeding but was not related to mortality.20) With growing concern about bleeding risk, the US Food and Drug Administration and the European Medicine Agency added warnings that prasugrel can cause serious bleeding and 10 mg prasugrel is generally not recommended in patients ≥75 years and weighing <60 kg. For elderly or lower body weight patients, 5 mg prasugrel daily is recommended as a maintenance dose to decrease bleeding complications.22) The incidence and clinical significance of bleeding have been underestimated in patients treated with PCI. Most randomized trials did not include patients with high risk of bleeding, such as renal failure on dialysis and bleeding diathesis, so they did not reflect the bleeding rate in real clinical practice. Furthermore, a recent study showed that bleeding events, even TIMI minor bleeding, are significantly associated with higher short and long-term mortality in patients with ACS.23)24)25) Additionally, Wiviott et al.13)26) reported significantly greater TIMI major and minor bleeding with 10 mg prasugrel than that with clopidogrel (3.9% vs. 3.0%, hazard ratio, 1.26; 95% confidence interval, 1.02-1.57, p=0.033) in the TRITON-TIMI population even <75 years old and weighing ≥60 kg, although the net clinical benefit favors 10 mg prasugrel compared with clopidogrel in those groups. There has been growing questions about 5 mg prasugrel as a maintenance dose to reduce bleeding complications and whether it provides an adequate antiplatelet inhibitory effect in patients at high risk for bleeding. Up to now, the platelet inhibitory effect or clinical efficacy of 5 mg prasugrel in non-low body weight and non-elderly patients after PCI has not been well established. The recent platelet function substudy of the TRIOLOGY ACS trial showed that the antiplatelet efficacy of 5 mg prasugrel was significantly greater than that of 75 mg clopidogrel using the VerifyNow P2Y12 assay in non-elderly patients (<75 years old) with low body weight (<60 kg) and in elderly patients (≥75 years) with non-low body weight. Within those groups, median PRU values were 139 vs. 209 (p<0.001) and 164 vs. 222 (p<0.001), which was lower than that of 5 mg prasugrel in our results.27) However, these pharmacodynamic results do not apply to younger and heavier patients, because body weight and age are the most important factors influencing the metabolism of prasugrel.28)29) Our study show that the lower maintenance dose of 5 mg prasugrel had a more potent platelet inhibitory effect with a lower mean PRU and lower HTPR rate compared with 75 mg clopidogrel in patients <75 years and >60 kg who underwent PCI. Interestingly, the mean PRU value of 5 mg prasugrel was between those of 10 mg prasugrel and 75 mg clopidogrel, which may indicate that 5 mg prasugrel provides a more potent platelet inhibitory effect compared with that of 75 mg clopidogrel and has a lower risk for bleeding compared to that of 10 mg prasugrel.
Although no TIMI major or minor bleeding events were observed during the study, 10 mg prasugrel tended to cause more bleeding events with high platelet inhibition compared with that of lower dose prasugrel and 75 mg clopidogrel. Bleeding complications were similar in 5 mg prasugrel and 75 mg clopidogrel groups, although 5 mg prasugrel manifested a greater antiplatelet effect.
These results provide pharmacodynamic evidence that 5 mg prasugrel can be alternative maintenance therapy to 75 mg clopidogrel or 10 mg prasugrel for reducing hemorrhagic complications with adequate platelet inhibition in patients <75 years and ≥60 kg who are at high risk for bleeding, such patients with renal failure, previous bleeding events, or hematologic disease, as well as older or lower body weight patients.
There are several limitations to this study. First, we measured platelet reactivity by only one method, which was the VerifyNow P2Y12 point-of-care assay. According to the POPULAR study, which performed a head-to-head comparison between the various methods for assessing platelet reactivity, VerifyNow P2Y12 point-of-care assay is one of the available platelet function tests for detecting high platelet reactivity or predicting clinical outcomes.30) Second, the follow-up platelet function test was performed only 30 days after taking the study drugs. Therefore, we could not show the early platelet inhibitory effect by 5 mg prasugrel compared with 75 mg clopidogrel. Third, this study was conducted only in patients on the maintenance phase at least 12 months after PCI. Thus, these data cannot be generalized to all patients on the maintenance phase of antiplatelet therapy. Fourth, our study population consisted of patients with ACSs, as well as patients with stable angina. However, all patients had been in the stable state for at least 1 year since the index procedure was performed. Therefore, we do not think that difference in the clinical presentation at the index PCI affected the final results. Last, our trial was designed to compare platelet inhibitory efficacy between study drugs and was not powered to assess clinical events or safety. Hence, the results of bleeding complications or clinical adverse events should be interpreted with caution for applying to real clinical practice.
In conclusion, the results of this study demonstrate that 5 mg prasugrel is associated with greater platelet inhibition with lower rates of HTPR compared with a standard dose of clopidogrel in patients <75 years old and weighing ≥60 kg after undergoing PCI. These results show that 5 mg prasugrel may be a better alternative maintenance antiplatelet therapy in non-low body weight and non-elderly patients who need more potent platelet inhibitory effect. The clinical implication of our data should be investigated in a future clinical trial.
Figures and Tables
Fig. 2
Platelet inhibitory effects assessed by the VerifyNow P2Y12 assay. Comparisons of P2Y12 reaction unit (A) and percentage platelet inhibition (B) between treatment groups at baseline and 30 days after randomization. Baseline p indicates comparisons among the three groups by analysis of variance.

Table 1
Baseline clinical characteristics of the study population

*p between 75 mg clopidogrel and 5 mg prasugrel, †p between 5 mg prasugrel and 10 mg prasugrel, ‡Creatinine clearance calculated by the Cockcroft and Gault method. CrCl: creatinine clearance, PCI: percutaneous coronary intervention, MI: myocardial infarction, LVEF: left ventricle ejection fraction, NST-ACS: non ST-segment elevation acute coronary syndrome, STEMI: ST-segment elevation myocardial infarction
Table 2
Medications 30 days after randomization
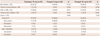
Table 3
Results of VerifyNow P2Y12 point-of-care assay

References
1. Hamm CW, Bassand JP, Agewall S, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2011; 32:2999–3054.
2. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011; 124:2574–2609.
3. Serebruany VL, Steinhubl SR, Berger PB, Malinin AI, Bhatt DL, Topol EJ. Variability in platelet responsiveness to clopidogrel among 544 individuals. J Am Coll Cardiol. 2005; 45:246–251.
4. Mega JL, Close SL, Wiviott SD, et al. Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med. 2009; 360:354–362.
5. Buonamici P, Marcucci R, Migliorini A, et al. Impact of platelet reactivity after clopidogrel administration on drug-eluting stent thrombosis. J Am Coll Cardiol. 2007; 49:2312–2317.
6. Cuisset T, Frere C, Quilici J, et al. Predictive values of post-treatment adenosine diphosphate-induced aggregation and vasodilator-stimulated phosphoprotein index for stent thrombosis after acute coronary syndrome in clopidogrel-treated patients. Am J Cardiol. 2009; 104:1078–1082.
7. Jin HY, Yang TH, Kim DI, et al. High post-clopidogrel platelet reactivity assessed by a point-of-care assay predicts long-term clinical outcomes in patients with ST-segment elevation myocardial infarction who underwent primary coronary stenting. Int J Cardiol. 2013; 167:1877–1881.
8. Parodi G, Marcucci R, Valenti R, et al. High residual platelet reactivity after clopidogrel loading and long-term cardiovascular events among patients with acute coronary syndromes undergoing PCI. JAMA. 2011; 306:1215–1223.
9. Brandt JT, Payne CD, Wiviott SD, et al. A comparison of prasugrel and clopidogrel loading doses on platelet function: magnitude of platelet inhibition is related to active metabolite formation. Am Heart J. 2007; 153:66.e9–66.e16.
10. Jernberg T, Payne CD, Winters KJ, et al. Prasugrel achieves greater inhibition of platelet aggregation and a lower rate of non-responders compared with clopidogrel in aspirin-treated patients with stable coronary artery disease. Eur Heart J. 2006; 27:1166–1173.
11. Wiviott SD, Trenk D, Frelinger AL, et al. Prasugrel compared with high loading- and maintenance-dose clopidogrel in patients with planned percutaneous coronary intervention: the Prasugrel in Comparison to Clopidogrel for Inhibition of Platelet Activation and Aggregation-Thrombolysis in Myocardial Infarction 44 trial. Circulation. 2007; 116:2923–2932.
12. Michelson AD, Frelinger AL 3rd, Braunwald E, et al. Pharmacodynamic assessment of platelet inhibition by prasugrel vs. clopidogrel in the TRITON-TIMI 38 trial. Eur Heart J. 2009; 30:1753–1763.
13. Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007; 357:2001–2015.
14. Erlinge D, Ten Berg J, Foley D, et al. Reduction in platelet reactivity with prasugrel 5 mg in low-body-weight patients is noninferior to prasugrel 10 mg in higher-body-weight patients: results from the FEATHER trial. J Am Coll Cardiol. 2012; 60:2032–2040.
15. Erlinge D, Gurbel PA, James S, et al. Prasugrel 5 mg in the very elderly attenuates platelet inhibition but maintains noninferiority to prasugrel 10 mg in nonelderly patients: the GENERATIONS trial, a pharmacodynamic and pharmacokinetic study in stable coronary artery disease patients. J Am Coll Cardiol. 2013; 62:577–583.
16. Varenhorst C, James S, Erlinge D, et al. Assessment of P2Y(12) inhibition with the point-of-care device VerifyNow P2Y12 in patients treated with prasugrel or clopidogrel coadministered with aspirin. Am Heart J. 2009; 157:562.e1–562.e9.
17. Price MJ, Endemann S, Gollapudi RR, et al. Prognostic significance of post-clopidogrel platelet reactivity assessed by a point-of-care assay on thrombotic events after drug-eluting stent implantation. Eur Heart J. 2008; 29:992–1000.
18. Bonello L, Tantry US, Marcucci R, et al. Consensus and future directions on the definition of high on-treatment platelet reactivity to adenosine diphosphate. J Am Coll Cardiol. 2010; 56:919–933.
19. Roe MT, Armstrong PW, Fox KA, et al. Prasugrel versus clopidogrel for acute coronary syndromes without revascularization. N Engl J Med. 2012; 367:1297–1309.
20. Stone GW, Witzenbichler B, Weisz G, et al. Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): a prospective multicentre registry study. Lancet. 2013; 382:614–623.
21. Unger EF. Weighing benefits and risks--the FDA's review of prasugrel. N Engl J Med. 2009; 361:942–945.
22. Wiviott SD, Antman EM, Braunwald E. Prasugrel. Circulation. 2010; 122:394–403.
23. Fifth Organization to Assess Strategies in Acute Ischemic Syndromes Investigators. Yusuf S, Mehta SR, et al. Comparison of fondaparinux and enoxaparin in acute coronary syndromes. N Engl J Med. 2006; 354:1464–1476.
24. Eikelboom JW, Mehta SR, Anand SS, Xie C, Fox KA, Yusuf S. Adverse impact of bleeding on prognosis in patients with acute coronary syndromes. Circulation. 2006; 114:774–782.
25. Mehran R, Pocock SJ, Stone GW, et al. Associations of major bleeding and myocardial infarction with the incidence and timing of mortality in patients presenting with non-ST-elevation acute coronary syndromes: a risk model from the ACUITY trial. Eur Heart J. 2009; 30:1457–1466.
26. Wiviott SD, Desai N, Murphy SA, et al. Efficacy and safety of intensive antiplatelet therapy with prasugrel from TRITON-TIMI 38 in a core clinical cohort defined by worldwide regulatory agencies. Am J Cardiol. 2011; 108:905–911.
27. Gurbel PA, Erlinge D, Ohman EM, et al. Platelet function during extended prasugrel and clopidogrel therapy for patients with ACS treated without revascularization: the TRILOGY ACS platelet function substudy. JAMA. 2012; 308:1785–1794.
28. Small DS, Farid NA, Payne CD, et al. Effect of intrinsic and extrinsic factors on the clinical pharmacokinetics and pharmacodynamics of prasugrel. Clin Pharmacokinet. 2010; 49:777–798.
29. Li YG, Ni L, Brandt JT, et al. Inhibition of platelet aggregation with prasugrel and clopidogrel: an integrated analysis in 846 subjects. Platelets. 2009; 20:316–327.
30. Breet NJ, van Werkum JW, Bouman HJ, et al. Comparison of platelet function tests in predicting clinical outcome in patients undergoing coronary stent implantation. JAMA. 2010; 303:754–762.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download