Abstract
Background and Objectives
We sought to determine the relationship between mean platelet volume (MPV), platelet distribution width (PDW), and platelet larger cell ratio (P-LCR) with slow coronary flow (SCF).
Subjects and Methods
Eighty participants who underwent coronary angiography were divided into two groups, 50 participants with SCF as case group, and 30 with normal coronary flow (NCF) as control group. Baseline characteristics and laboratory data were collected before angiography.
Results
Platelet volume indices MPV (10.8±1.2 fL), PDW (14.5±2.2 fL), and P-LCR (30.5±8.1%) in the SCF group were significantly (p<0.05) higher than those (10.1±0.9 fL, 13.2±1.8 fL, and 26.8±6.8%, respectively) in the NCF group. The patients with three SCF arteries had significantly higher platelet volume indices compared to those with NCF arteries; however, the patients with one SCF artery did not. Based on linear regression model, MPV, PDW, and P-LCR were independent predictors of mean infarction frame counting (TFC). In multivariate analysis, MPV {odds ratio (OR)=32.393, 95% confidence interval (CI)=1.189-882.606, p=0.039} and P-LCR (OR=0.566, 95% CI=0.330-0.937, p=0.028) were independent predictors of SCF.
Slow coronary flow (SCF) phenomenon is a coronary microvascular disease diagnosed by detection of delayed dyeopacification in coronary arteries during an angiography in the lack of obstructive coronary artery disease. The incidence of SCF has been reported to be approximately 1-7% in patients who undergo a diagnostic coronary angiography due to suspected coronary artery disease.1) Despite being a well-known phenomenon, the pathophysiologic mechanisms of SCF remain unknown. Potential mechanisms involved in SCF are: small vessel and endothelial dysfunctions,2)3) inflammation,4)5) diffuse atherosclerosis,6) and increased platelet aggregability.7)
Platelets have been shown to have an important role in the pathogenesis of acute coronary syndrome. Some mediators involved in inflammatory processes and coagulatory pathways might have contributed to the development of atherosclerotic and atherothrombotic diseases.8)9) Mean platelet volume (MPV), an index of platelet activation, has been shown to be associated with adverse cardiovascular outcomes.10) MPV was found to be elevated in SCF cases compared to normal ones.11) Platelet distribution width (PDW) is found to be increased during platelet activation.12) Platelet larger cell ratio (P-LCR), an idicator of larger platelet circulating (>12 fL) , has also been used to monitor platelet activity.13)
Given the probabale pathophysiologic roles of inflammation and platelet dysfunction in the development of SCF, we sought to determine the relationship between SCF and platelet activation using platelet volume indices MPV, PDW, and P-LCR.
In a case-control study, a total of 1650 consecutive patients who underwent diagnostic coronary angiography due to unstable angina and/or chest discomfort without positive non-invasive tests were evaluated in our two university centers, including Seyyed-al-Shohada Heart Center and Taleghani Hospital from April 2013 to November 2013. The local ethics committee in the Urmia University of Medical Sciences, West-Azerbaijan province, Iran, approved this investigation. Of evaluated participants, 50 diagnosed with SCF based on Thrombolysis in Myocardial Infarction frame counting (TFC) method were used in the case group. Based on angiographic examinations, 30 participants had normal coronary flow (NCF) were considered as control group after fulfilling inclusion and exclusion criteria.
Exclusion criteria were: 1) diagnosed as coronary artery disease; 2) coronary artery stenosis >50% of the coronary artery diameter in angiographic evaluation; 3) peripheral arterial disease; 4) valvular heart disease; 5) thrombocytopenia; 6) hematologic diseases; 7) hepatic diseases; 8) chronic inflammatory disease; 9) malignancies; 10) infectious disease; 11) autoimmune disease; 12) anemia; 13) renal failure; and 14) thyroid diseases.
All patients underwent coronary angiographic examination through femoral artery using Judkins' method (Siemens, Forcheim, Germany). The contrast media of iodixanol (GE Healthcare, Cork, Ireland) was used in all cases. A single catheter size was used in this cohort. Two cardiologists who were blinded to the patients' condition and clinical features evaluated all angiograms to identify SCF using TFC method.14) The numbers of angiographic frames were recorded at 30 frames per second. The coronary flow was calculated as reaching contrast media to the defined distal part of coronary arteries. The end distal parts in the left anterior descending (LAD) and left circumflex (LCX) arteries were distal bifurcation points. The right coronary artery (RCA) was the first posterolateral branch point. The calculated frame counting for LAD artery was divided by 1.7 based on the predefined criteria.14) According to Gibson et al.14) the cut-off values for detecting SCF were ≥36.2±2.6, ≥20.4±3, and ≥22.2±4.1 frames for LAD, RCA, and LCX arteries, respectively. In addition, mean TFC was calculated as the mean of three measured TFCs.
All blood samples were provided through vein puncture before undergoing angiography. Blood were collected into tubes containing ethylenediaminetetraacetic acid. Blood were analyzed 20-30 minutes after sampling. Automated cell count analyzer (Sysmex, Kobe, Japan) was used to measure complete blood count.
Continuous variables were analyzed using t-test, one-way analysis of variance or Mann Whitney U test as appropriate based on the variables' distribution normality. Tukey's post hoc test was used to compare paired groups. Categorical variables were analyzed using chi-squared test. Pearson correlation coefficient was used to identify associations between two continuous variables. Receiver operating characteristic curve was constructed to detect the accuracy of platelet volume indices to differentiate SCF from NCF. Linear regression analysis was used to detect the predictors of mean TFC. Multivariate logistic regression analysis and backward stepwise were conducted to determine the predictors of SCF among our studied cohort. In this analysis, demographics and laboratories were entered into the model as covariates, and the status of SCF was considered as a dependent variable. All analyses were performed using Statistical Package for the Social Sciences (SPSS) version of 18.0 (SPSS Inc., Chicago, IL, USA). A p of <0.05 was considered statistically significant.
Baseline clinical characteristics of patients were summarized in Table 1. A total of 50 patients with SCF and 30 patients with NCF were studied. The mean of age was 54.8±11.1 years, with 53.8% male. Based on the baseline characteristics, patients with SCF were more likely to have diabetes and hypertension than NCF (24% vs. 6.7%, p=0.048 and 50% vs. 23.3%, p=0.018, respectively). The platelet volume indices MPV (p=0.005), PDW (p=0.007), and P-LCR (p=0.039) were significantly higher in the SCF group compared to those in the NCF group (Table 1).
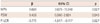
Based on correlation analysis, positive and significant correlations existed between the platelet volume indices and the TFC values in three coronary arteries except between P-LCR and LAD and LCX arteries (Table 2). When comparing the differences of platelet volume indices and the extent of SCF, the amounts of MPV, PDW, and P-LCR were significantly higher in patients with three SCF arteries compared to those of patients without SCF (p=0.004, p=0.005, and p=0.014, respectively). In addition, PDW was significantly (p=0.026) higher in patients with two SCF arteries compared with patients without SCF (Fig. 1). Receiver operating characteristic curve analysis showed that the best cut-off values of MPV, PDW, and P-LCR to distinguish SCF from NCF were 10.4 fL, 13.9 fL, and 28%, respectively (Fig. 2). Accordingly, MPV had significantly higher amount of area under the curve (AUC) (AUC=0.669, p=0.012).
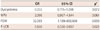
All variables whose p were significant (p<0.05) based on bivariate analysis were entered into the linear regression analysis. According to this model, MPV {β=32.393, 95% confidence interval (CI) 0.678-11.048, p=0.027}, PDW (β=0.428, 95% CI 0.060-3.924, p=0.043), and P-LCR (β=-0.771, 95% CI -1.917 - -0.117, p=0.027) were independent predictors of mean TFC (Table 3). Results of multivariate analysis were summarized in the Table 4. According to this model, MPV {odds ratio (OR)=32.393, 95% CI=1.189-882.606, p=0.039} and P-LCR (OR=0.566, 95% CI=0.330-0.937, p=0.028) were independent predictors of SCF among all variables measured in this study.
In this study, for the first time, we showed that the platelet volume indices MPV, PDW, and P-LCR were significantly higher in the patients with SCF compared to those in the NCF group. In addition, their elevated values were associated with the extent of SCF. There were positive correlations between platelet volume indices and the TFC measured for three coronary arteries. Furthermore, MPV, PDW, and P-LCR were found to be the independent predictors of mean TFC.
Platelets are important blood cells that participate in the processes of atherothrombotic events, coagulation, and inflammation.8) MPV, PDW, and P-LCR are indicators of platelet size, volume, and activation. Elevated MPV value has been shown to be involved in the pathogenesis of atherosclerosis and thrombogenesis.15) Gökçe et al.7) have deomonastrated that platelet aggregability induced by ristocetin, collagen, and adenosine diphosphate was significantly higher in patients with SCF compared to that of NCF, indicating the potential of platelet in SCF pathogenesis. In a case-control study, Celik et al.11) have demonstrated that increased MPV and plasma sP-selectin values are higher in SCF patients compared to those of NCF ones, with positive correlations between MPV values and the TFC of coronary artery. They concluded that the increased platelet activity existed in SCF might be a pathogenesis for SCF development. Elsherbiny et al.16) have shown that MPV is higher in SCF compared to NCF. Nurkelam et al.17) have reported that SCF cases with unstable angina has higher MPV compared to SCF ones with stable coronary artery disease and NCF cases. Other studies have also confirmed that elevated MPV is associated with the presence of SCF.18)19) Furthermore, it has been shown that MPV correlated with the extent of SCF.19) In consistent with those research findings, our results also reveald that MPV was significantly higher in SCF compared to NCF cases. Our results also revealed that MPV was associated with mean TFC of three coronary arteries. In addition, for the first time, we found that PDW and P-LCR were also higher in SCF.
Inflammation is another pathophysiologic mechanism involved in SCF. Li et al.4) found that C-reactive protein (CRP) and interlukin-6 were higher in SCF patients and that SCF was was correlated with mean TFC. In additon, some adhesion molecules, including intercellular adhesion molecule-1, vascular cell adhesion molecule-1, and E-selectin as markers of endothelial activation or inflammation were reported to be significantly higher in patients diagnosed with SCF.5) Given the probable role of inflammation in the SCF pathogenesis, some clinical trials have been conducted. Albayrak et al.20) have demonstrated that Nebivolol reduced CRP level and controlled the chest pain of patients with SCF. The impact of simvastatin on improving myocardial perfusion in SCF is another evidence to support the role of inflammatory processes in the SCF development.6) In addition, platelets involve in inflammatory pathways through releasing mediators, and larger ones contain more mediators and activity. Considering the results of this study and those other studies demonstrating increased platelet indices in SCF patients, further clinical trials are needed to illustrate the effects of anti-platelet and anti-inflammatory agents on SCF and to prove the relationship between platelet-related disorders and SCF pathogenesis.
In order for recurrent chest pain to be controlled, some drugs such as beta-blockers, nitrates, and statins have been used. However, no proper impact of these agents have been demonstrated. In this study, we did not focus on any specific drug effect on SCF. However, due to the above mentioned pathophysiologic mechanisms of SCF, including inflammation, thrombogeneity, and atherosclerosis, and due to the relationship between increased platelet volume indices and SCF, it may be of great benefit to prescribe anti-platelet and anti-inflammatory agents to reduce platelet volume indices. Beside the therapeutic use of these markers, they could be used for risk staritification of SCF cases.
Based on our findings, it can be proposed that increased platelet volume indices MPV, PDW, and P-LCR are inexpensive and widely available tests associated with SCF and that they might be involved in the pathophisiology of SCF. Considering the fact that platelet volume indices were indicators of platelet activation and consequent inflammatory processes, we suggest that increased MPV, PDW, and P-LCR could be indicators of platelet dysfunction and inflammation in patients diagnosed with SCF. Therefore, platelet volume indices MPV, PDW, and P-LCR could be considered for monitoring drug efficacy and risk stratification of such cases.
Some limitations existed in the present study based on its design. Firstly, the small sample size and the lack of some variables, including lipid profile tests and familial history of cardiovascular disease, were the main limitation of this study. Secondly, we did not measure other inflammation and platelet function markers such as CRP, which could provide more information regrding the pathophysilogic mechanisms involved in SCF. Finally, because we chose the participants consecutively based on the inclusion and exclusion criteria, selection bias may have occurred during patients enrollment.
Platelet volume indices MPV, PDW, and P-LCR were significantly higher in SCF patients compared to those in NCF. The increases of platelet volume indices MPV, PDW, and P-LCR were associated with the extent of SCF. Moreover, MPV, PDW, and P-LCR were found to be indipendent predictors of mean TFC.
Figures and Tables
Fig. 1
Relationship between platelet volume indices MPV (A), PDW (B), P-LCR (C), and the extent of SCF. MPV: mean platelet volume, PDW: platelet distribution width, P-LCR: platelet larger cell ratio, SCF: slow coronary flow.

Fig. 2
Receiver operating characteristics curve analysis to detect the best cut-off values of platelet volume indices for differentiation between normal and slow coronary flows. AUC: area under the curve, CI: confidence interval, Sn: sensitivity, Sp: specificity, MPV: mean platelet volume, PDW: platelet distribution width, P-LCR: platelet larger cell ratio.
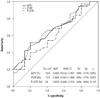
Table 1
Baseline clinical and laboratory features of studied patients
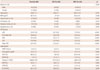
Values are presented as mean±standard deviation and number (percentage). *p were calculated using t-test or Mann-Whitney U teat as appropriate. SCF: slow coronary flow, NCF: normal coronary flow, BMI: body mass index, TFC: Thrombolysis in Myocardial Infarction frame counting, LAD: left anterior descending, RCA: right coronary artery, LCX: left circumflex, WBC: white blood cell count, MCV: mean corpuscular volume, RDW: red cell width distribution, MPV: mean platelet volume, PDW: platelet distribution width, P-LCR: platelet larger cell ratio
Table 2
Correlation between the three coronary arteries TFC and platelet volume indices

Table 3
Linear regression analysis to identify the predictors of mean TCF
| β | 95% CI | p | |
|---|---|---|---|
| MPV | 0.669 | 0.678-11.048 | 0.027 |
| PDW | 0.428 | 0.060-3.924 | 0.043 |
| P-LCR | -0.771 | -1.917- -0.117 | 0.027 |
References
1. Goel PK, Gupta SK, Agarwal A, Kapoor A. Slow coronary flow: a distinct angiographic subgroup in syndrome X. Angiology. 2001; 52:507–514.
2. Tambe AA, Demany MA, Zimmerman HA, Mascarenhas E. Angina pectoris and slow flow velocity of dye in coronary arteries--a new angiographic finding. Am Heart J. 1972; 84:66–71.
3. Mosseri M, Yarom R, Gotsman MS, Hasin Y. Histologic evidence for small-vessel coronary artery disease in patients with angina pectoris and patent large coronary arteries. Circulation. 1986; 74:964–972.
4. Li JJ, Qin XW, Li ZC, et al. Increased plasma C-reactive protein and interleukin-6 concentrations in patients with slow coronary flow. Clin Chim Acta. 2007; 385:43–47.
5. Turhan H, Saydam GS, Erbay AR, et al. Increased plasma soluble adhesion molecules; ICAM-1, VCAM-1, and E-selectin levels in patients with slow coronary flow. Int J Cardiol. 2006; 108:224–230.
6. Cakmak M, Tanriverdi H, Cakmak N, Evrengul H, Cetemen S, Kuru O. Simvastatin may improve myocardial perfusion abnormality in slow coronary flow. Cardiology. 2008; 110:39–44.
7. Gökçe M, Kaplan S, Tekelioğlu Y, Erdoğan T, Küçükosmanoğlu M. Platelet function disorder in patients with coronary slow flow. Clin Cardiol. 2005; 28:145–148.
8. Davì G, Patrono C. Platelet activation and atherothrombosis. N Engl J Med. 2007; 357:2482–2494.
9. van der Loo B, Martin JF. A role for changes in platelet production in the cause of acute coronary syndromes. Arterioscler Thromb Vasc Biol. 1999; 19:672–679.
10. Seyyed-Mohammadzad MH, Eskandari R, Rezaei Y, et al. Prognostic value of mean platelet volume in patients undergoing elective percutaneous coronary intervention. Anadolu Kardiyol Derg. 2014; DOI: 10.5152/akd.2014.5169.
11. Celik T, Yuksel UC, Bugan B, et al. Increased platelet activation in patients with slow coronary flow. J Thromb Thrombolysis. 2010; 29:310–315.
12. Vagdatli E, Gounari E, Lazaridou E, Katsibourlia E, Tsikopoulou F, Labrianou I. Platelet distribution width: a simple, practical and specific marker of activation of coagulation. Hippokratia. 2010; 14:28–32.
13. Grotto HZ, Noronha JF. Platelet larger cell ratio (P-LCR) in patients with dyslipidemia. Clin Lab Haematol. 2004; 26:347–349.
14. Gibson CM, Cannon CP, Daley WL, et al. TIMI frame count: a quantitative method of assessing coronary artery flow. Circulation. 1996; 93:879–888.
15. Chu SG, Becker RC, Berger PB, et al. Mean platelet volume as a predictor of cardiovascular risk: a systematic review and meta-analysis. J Thromb Haemost. 2010; 8:148–156.
16. Elsherbiny IA, Shoukry A, El Tahlawi MA. Mean platelet volume and its relation to insulin resistance in non-diabetic patients with slow coronary flow. J Cardiol. 2012; 59:176–181.
17. Nurkalem Z, Alper AT, Orhan AL, et al. Mean platelet volume in patients with slow coronary flow and its relationship with clinical presentation. Turk Kardiyol Dern Ars. 2008; 36:363–367.
18. Sen N, Basar N, Maden O, et al. Increased mean platelet volume in patients with slow coronary flow. Platelets. 2009; 20:23–28.
19. Isik T, Ayhan E, Uyarel H, et al. Increased mean platelet volume associated with extent of slow coronary flow. Cardiol J. 2012; 19:355–362.
20. Albayrak S, Ordu S, Yuksel H, Ozhan H, Yazgan O, Yazici M. Efficacy of nebivolol on flow-mediated dilation in patients with slow coronary flow. Int Heart J. 2009; 50:545–553.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download