Abstract
Background and Objectives
Although prasugrel allows for rapid and potent platelet inhibition, the efficacy and safety of lower doses of prasugrel for patients of East Asian ethnicity has not yet been investigated. We compared the effect of a lower loading dose (LD) of prasugrel with conventional LDs of clopidogrel and prasugrel in Korean patients.
Subjects and Methods
Forty-three Korean patients undergoing coronary angiography were enrolled in the study. Participants were randomly administered LDs of clopidogrel 600 mg, prasugrel 30 mg or prasugrel 60 mg prior to coronary angiography. Platelet reactivity was assessed at baseline and at the time of peak platelet inhibition using light transmission aggregometry (LTA), the VerifyNow assay, and multiple electrode aggregometry.
Results
Although baseline platelet reactivity between the groups showed no significant differences, at the time of peak platelet inhibition, the prasugrel 30 mg (18.9±10.0%) and 60 mg groups (13.8±10.8%) showed significantly more potent platelet inhibition than the clopidogrel 600 mg group (52.9±15.8%; p<0.001) by LTA. However, there were no significant differences between the prasugrel 30 mg and 60 mg groups (p=0.549).
Although clopidogrel and aspirin have been the backbone of antiplatelet therapy for coronary artery disease (CAD) patients, clopidogrel has several limitations including delayed onset of peak concentration and pharmacodynamic inter-patient variability, which can result in high on-treatment platelet reactivity (HPR). These drawbacks are known to be associated with adverse cardiovascular outcomes.1) In comparison to clopidogrel, prasugrel has a more advantageous metabolic pathway, allowing for more rapid and potent platelet inhibition.2) Updated guidelines recommend prasugrel as a first line antiplatelet agent3)4) or stipulate its preference over clopidogrel5) for patients with acute coronary syndrome.
However, a number of concerns have been raised in relation to the differences in pharmacodynamic and pharmacokinetic responses to prasugrel in East Asian ethnicities.6)7) It has been demonstrated that a lower prasugrel loading dose (LD) can result in more potent pharmacodynamic effects than clopidogrel 600 mg with comparable efficacy in comparison to conventional prasugrel LD when administered to healthy Korean subjects.8)
We compared the antiplatelet effects of a lower prasugrel LD (30 mg) with both a conventional clopidogrel LD of 600 mg and prasugrel 60 mg in Korean patients undergoing elective coronary angiography.
Patients between 18 and 80 years of age with stable or unstable angina undergoing elective coronary angiography were eligible for the study. Those with a previous history of transient ischemic attack or stroke, intracranial neoplasm, or uncontrolled malignant disease were excluded. Additionally, those with a history of antiplatelet or anticoagulation treatment within the previous month, contraindications to the study drug, bleeding diathesis, hemoglobin <10 g/dL, platelet count <100000/mm3, significant renal insufficiency defined as a glomerular filtration rate <60 mL/min/1.73 m2, significant hepatic impairment defined as serum liver enzyme or bilirubin >3 times normal limit, and body weight less than 50 kg were also ineligible. All of the subjects who participated in the study provided written informed consent prior to participation.
This study was designed as a prospective, randomized, open-label active controlled study to compare the pharmacodynamic effects of LD of clopidogrel 600 mg, prasugrel 30 mg, and prasugrel 60 mg. Enrolled patients were randomly assigned to either the clopidogrel 600 mg group, prasugrel 30 mg group or prasugrel 60 mg group on a 1:1:1 ratio using Excel (Microsoft Corporation, Redmont, DC, USA).
Platelet reactivity was measured at baseline and at the time of peak platelet inhibition. The time of peak platelet inhibition was defined as 2 hours after administration of LD for the prasugrel groups and 6 hours after LD for the clopidogrel group.8) Coronary angiography with or without percutaneous coronary intervention (PCI) was performed in accordance with the current recommended guidelines.
The study design was approved by the Institutional Review Board of Dong-A University Hospital and was registered at www.clinicaltrials.gov (NCT02070159).
Platelet reactivity was measured using three different methods; light transmission aggregometry (LTA), the VerifyNow assay (Accumetrics, San Diego, CA, USA), and multiple electrode aggregometry (MEA, Dynabyte Medical, Munich, Germany). Blood samples for the assessment of platelet reactivity were collected via direct venipuncture at the antecubital fossa or via the arterial sheath in patients who had already been punctured via the radial or femoral arterial sheath at the time of assessment. The numerical results of LTA were expressed as a percentage, VerifyNow assay as P2Y12 reaction units (PRU), and the MEA, as arbitrary units (U).
For comparisons of the extent of platelet inhibition using LTA, VerifyNow, and MEA devices, we compared the percent inhibition for each unit. Percent inhibition was calculated using the following formula: % inhibition={(baseline reactivity unit-peak reactivity unit)/baseline reactivity unit}×100.
The incidence of HPR and low on-treatment platelet reactivity (LPR) in each group were also compared. The HPR was defined as the results of LTA ≥48%9) or ≥55%,10)11) PRU ≥2429) or ≥275,11)12)13)14) and MEA assay MEA 37 U9) or 54 U15) at the time of peak platelet inhibition. The LPR was defined as LTA <12,16)17) PRU <85,16) MEA <19.16)
The primary endpoint was the difference in platelet reactivity between the study groups at the time of peak platelet inhibition. Secondary endpoints included differences in percent inhibition, as well as incidence of HPR and LPR between study groups. Safety outcomes included peri-procedural complications, adverse reactions to the study drug, and bleeding events.
After the assessment of platelet function, patients in the prasugrel 30 mg group who were indicated for maintenance on dual antiplatelet therapy continued to receive conventional maintenance doses (MD) of clopidogrel or prasugrel as per the decision of the primary physician. Participants of the study were observed for adverse clinical events for 24 hours and followed-up 7 days later via an outpatient visit or telephone interview.
The results of platelet reactivity was expected to be normally distributed with a standard deviation of less than 0.2, and the difference in platelet inhibition between the clopidogrel 600 mg group and the prasugrel 30 mg group was assumed to be 30%.8) Considering a 30% higher concentration of active metabolites in East Asian ethnicity on average6) and an approximately 20% difference in platelet inhibition between 10 mg and 20 mg prasugrel LDs,7) the response difference between the prasugrel 30 mg and 60 mg groups was also assumed to be 30%. The minimum number of subjects in each group required was calculated to be nine subjects in order to provide a 90% power to detect the mean differences. Regarding the scarcity of previous studies on lower LDs of prasugrel and possible data loss, we decided to allocate at least 13 subjects in each group.
Results were expressed as mean±standard deviation and multiple comparisons including platelet reactivity for each group were analyzed by 1-way analysis of variance followed by Dunnett's T3 post hoc test. Values of p<0.05 were considered significant. In addition, we also performed independent t-tests and Kruskal-Wallis tests with Dunnett's T3 post hoc test for confirmation. For comparisons of nominal variables, a cross-tabulation with a Fisher's exact test was used. Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) Version 14 (SPSS Inc., Chicago, IL, USA). All statistical tests were carried out at the 0.05 significance level.
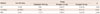
Between January 2012 and January 2013, 54 patients were screened for eligibility. Of the screened subjects, three were excluded due to age greater than 80 years, three due to a history of stroke, one due to significant kidney dysfunction, and four declined to participate. In total, 43 patients were randomized, all of whom completed the study. The mean age was 63.4±10.2 years, mean body weight was 66.0±10.7 kg and 36 patients (83.7%) were male. By random assignment, 14 patients (32.6%) were allocated to the clopidogrel group, 15 patients (34.9%) to the prasugrel 30 mg group, and 14 patients (32.6%) to the prasugrel 60 mg group. Hypertension was reported for 25 patients (58.1%), 17 patients had diabetes mellitus (39.5%), and 23 patients (53.5%) were smokers. PCIs were performed in 28 patients (65.1%), of which the incidence showed no significant difference between study groups. Adverse cardiovascular events including stent thrombosis, bleeding, and adverse drug reactions were not observed during the study period. There were no significant differences in clinical characteristics of the enrolled patients between study groups (Table 1).
The mean baseline platelet reactivity of the enrolled patients was 65.0±11.9% by LTA, 323.1±68.2 PRU by VerifyNow, and 57.9±20.8 U by MEA, and platelet reactivity was significantly reduced at the time of peak platelet inhibition; 28.3±21.2% by LTA, 145.1±105.3 PRU by VerifyNow, and 26.3±14.6 U by MEA (p<0.001 for all methods). The results of platelet reactivity at baseline and at the time of peak platelet inhibition in each study group are shown in Table 2. Baseline platelet reactivity between study groups using LTA (Fig. 1A), VerifyNow (Fig. 1B), and MEA (Fig. 1C) were not significantly different, whereas platelet reactivity at peak platelet inhibition using LTA (Fig. 1D), VerifyNow (Fig. 1E), and MEA (Fig. 1F) were significantly different. In the post hoc analysis, significant differences were observed between the clopidogrel 600 mg group and both prasugrel groups. However, there was no significant difference between the prasugrel 30 mg and 60 mg groups. Independent t-tests also showed consistent results.
The overall inhibition rate in the enrolled patients was 57.8±29.5% as measured by LTA, 54.1±33.4% by VerifyNow, and 52.5±33.4% by MEA. The inhibition rate in the clopidogrel 600 mg, prasugrel 30 mg, and prasugrel 60 mg groups were 22.8±19.3%, 70.8±14.6%, 78.9±14.9% by LTA (p<0.001), 12.3±15.9%, 67.8±19.1%, 81.1±8.8% by VerifyNow (p<0.001), and 32.3±17.1%, 66.2±13.8%, 58.1±19.5% by MEA (p<0.001), respectively. Post hoc analysis revealed significant differences between the clopidogrel group and both prasugrel groups, whereas no significant difference was present between the prasugrel 30 mg and 60 mg groups (Fig. 2).
Details of predefined HPR incidence are shown in Table 3. There was one case of HPR in the prasugrel 30 mg group when HPR was defined as PRU ≥242, and HPR was not observed in the prasugrel 60 mg group. Although the prasugrel groups showed very low incidence of HPR, the clopidogrel 600 mg group showed various incidence of HPR according to different methods and cut-off values.
Incidences of predefined LPR are shown in Table 4. Although the clopidogrel 600 mg group showed very low incidence of LPR, both prasugrel groups exhibited a relatively higher incidence of LPR. Incidence in the prasugrel 30 mg group was lower than in the prasugrel 60 mg with LTA and VerifyNow methods, whereas it was higher when using the MEA assay.
Although prasugrel treatment reaches a higher active metabolite peak concentration more rapidly, higher platelet inhibition after prasugrel LDs and MDs has been reported in patients of East Asian ethnicity over their Caucasian counterparts in pharmacodynamic and pharmacokinetic studies.6) Subsequently, lower LDs and MDs of prasugrel were shown to exhibit lower platelet reactivity when compared with clopidogrel 300 mg LD and 75 mg/day MD in Japanese CAD patients.7) Previously, we reported a more rapid, potent, and consistent platelet inhibition when using 30 mg LD of prasugrel compared with 600 mg LD of clopidogrel, with comparable platelet inhibition to 60 mg LD of prasugrel in healthy Korean subjects.8) In this study, which was conducted with Korean CAD patients undergoing elective coronary angiography, we confirmed these findings. The mean value of platelet reactivity in the prasugrel 30 mg group was not significantly different from the prasugrel 60 mg group. The prasugrel 30 mg and 60 mg groups showed significantly lower platelet reactivity than the clopidogrel 600 mg group. In addition, a 30 mg LD of prasugrel did not increase the incidence of HPR. The highest incidence rate of HPR was observed in the clopidogrel group.
In the study of Yokoi et al.,7) they prospectively compared a lower LD and MD of prasugrel with an LD of clopidogrel 300 mg and MD of clopidogrel 75 mg/day in Japanese CAD patients. Platelet inhibition with a much lower LD of prasugrel (15 mg) exhibited similar effects to an LD of clopidogrel 300 mg. More recently, MD of prasugrel 5 mg/day in Korean CAD patients was shown to be more potent than clopidogrel 75 mg/day in Korean CAD patients. However, in regards of LD, a 600 mg LD of clopidogrel is known to be superior to 300 mg LD of clopidogrel, and is frequently used in many centers.18) Therefore, in the present study, we compared a 30 mg LD of prasugrel with a 600 mg LD of clopidogrel, a higher dose than previously studied. We decided to use 30 mg as LD of prasugrel because it is the same dose used in our previous study in healthy Korean subjects.8) We compared it with a conventional 60 mg prasugrel LD group, revealing a similar platelet inhibition in both groups in Korean CAD patients.19)
In our previous study, peak inhibition of platelet reactivity was achieved 2 hours after administration of LD prasugrel and 6 hours after the clopidogrel LD administration.8) Platelet reactivity remained at a steady state thereafter. Therefore, we did not serially measure the platelet reactivity, but measured at baseline, at 2 hours after prasugrel LD, and 6 hours after clopidogrel LD
To determine HPR incidence, we used two cut-off values based on previous publications.9)10)11)12)13)14)15) However, they are higher than those used in other reports and the general consensus.16) This was in consideration of ethnic differences, which have reported higher cut-off values for patients of East Asian ethnicity.11)12)13)14) However, the results were consistent with lower cut-off values for HPR with a PRU of 220; HPR was detected in 13 patients (92.9%) in the clopidogrel 600 mg group and 2 patients (13.3%) in the prasugrel 30 mg group, while no incidences were detected in the prasugrel 60 mg group.
It has been demonstrated that LPR is associated with an increased risk of bleeding.20)21) Additionally, LPR arising from prasugrel treatment has specifically been linked with an increased risk of bleeding events.22)23)24)25) We defined LPR using the cut-off value in a recently adopted consensus report.16) The prasugrel 30 mg group showed a lower incidence of LPR than the prasugrel 60 mg group. There was no incidence of LPR in the clopidogrel group.
In terms of potency, consistency, and rapid onset, prasugrel is superior to clopidogrel. Although HPR was a major concern with the use of clopidogrel, prasugrel showed lower platelet reactivity and a reduced incidence rate of ischemic events.26) However, the ideal antiplatelet effect of prasugrel can be achieved when the risk of ischemic events is reduced without an increase in the risk of bleeding. Although the current recommended LD of 60 mg prasugrel lowered the risk of ischemic events, the potent antiplatelet efficacy of prasugrel resulted in an increased risk of bleeding events. Lower platelet reactivity is associated with an increased risk of bleeding20)24) and it is consistent with the use of prasugrel.25) In the present study, the lower LD of 30 mg prasugrel resulted in potent platelet inhibition without significant differences to conventional 60 mg LD prasugrel. In addition, the lower LD of prasugrel did not increase the incidence of HPR and reduced the incidence of LPR as measured by LTA and VerifyNow.
We note several limitations in the present study. First, the total number of enrolled patients is relatively small and other possible confounding factors such as smoking and PCI were not controlled. However, the platelet reactivity was assessed using three different methods, and the results were consistent. Analyses using various non-parametric statistical tests confirmed the consistency. Second, we only evaluated pharmacodynamics and did not measure concentrations of the active metabolite, nor clinical outcomes. Also, it is thought that the pharmacodynamic effect of prasugrel does not have a linear relationship with the active metabolite, especially at higher dosages. Therefore, the present study does not explain why the lower dose of prasugrel exhibited a similar antiplatelet effect. Additionally, with the small sample size, adverse cardiovascular events hardly occur. Third, the significant inhibition of platelets by prasugrel does not denote a reduction of ischemic event and mortality.27) However, recent data from Japan stated that a lower dose of prasugrel (20 mg LD followed by 3.75 mg MD) in acute coronary syndrome patients treated with PCI resulted in a low incidence of ischemic and bleeding events.28) Therefore, prasugrel doses resulting in minimal incidence of HPR and a low incidence of LPR without an additional risk of bleeding might be the ideal dose, especially in East Asian people. Fourth, the LD of 30 mg was arbitrary. Although we used the LD of 30 mg based on the previous study conducted in Korean healthy volunteers,8) follow-up studies evaluating the appropriate dose for East Asian ethnicities are required.
The present randomized, controlled, open-label study comparing the pharmacodynamic effects of prasugrel 30 mg, with clopidogrel 600 mg and prasugrel 60 mg in Korean CAD patients undergoing elective coronary angiography revealed a significantly higher platelet inhibition in the 30 mg LD prasugrel group compared to the 600 mg LD clopidogrel group. The LD of prasugrel 30 mg was found to cause similar platelet inhibition to 60 mg LD prasugrel. Additionally, the incidence of HPR in the prasugrel 30 mg group did not increase, resulting in a lower overall incidence of LPR. A large prospective study evaluating the clinical outcomes of lower LD prasugrel with long-term observation is needed to confirm the clinical benefits of a lower prasugrel LD.
Figures and Tables
Fig. 1
Platelet reactivity at baseline and peak platelet inhibition. Platelet reactivity measured at baseline (A, B, and C) and at the time of peak platelet inhibition (D, E, and F) using LTA, VerifyNow, and MEA. The baseline platelet reactivity values were statistically identical between study groups, whereas platelet reactivity at the time of peak platelet inhibition exhibited significant differences. Although platelet reactivity values for the clopidogrel 600 mg group were significantly higher than both prasugrel groups, there was no statistical difference between the prasugrel 30 mg and 60 mg groups. LTA: light transmission aggregometry, MEA: multiple electrode aggregometry.

Fig. 2
Comparison of inhibition (%) between study groups. Percent inhibition was significantly lower in the clopidogrel 600 mg group than for both prasugrel groups. However, there was no statistical difference between the prasugrel groups. LTA: light transmission aggregometry, MEA: multiple electrode aggregometry.

Table 1
Baseline clinical characteristics of the enrolled patients

Data are expressed as number of cases (percentage) or mean±standard deviation. *The majority of enrolled patients presented with stable angina. Patients with evidence of myocardial infarction were not included in the study. Hb: hemoglobin, Hct: hematocrit, PLT: platelet, TC: total cholesterol, LDL-C: low density lipoprotein-cholesterol, DM: diabetes mellitus, HTN: hypertension, PCI: percutaneous coronary intervention
Table 2
Platelet function at baseline and peak platelet inhibition in each study group

Table 3
Incidence of predefined HPR in each study group

Acknowledgments
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI14C1063) and funded by the Ministry of Education, Science and Technology (No. 2012R1A1A1A20 05932), Republic of Korea.
References
1. Gurbel PA, Bliden KP, Hiatt BL, O'Connor CM. Clopidogrel for coronary stenting: response variability, drug resistance, and the effect of pretreatment platelet reactivity. Circulation. 2003; 107:2908–2913.
2. Sugidachi A, Ogawa T, Kurihara A, et al. The greater in vivo antiplatelet effects of prasugrel as compared to clopidogrel reflect more efficient generation of its active metabolite with similar antiplatelet activity to that of clopidogrels active metabolite. J Thromb Haemost. 2007; 5:1545–1551.
3. 2012 Writing Committee Members. Jneid H, Anderson JL, et al. 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/Non-ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2012; 126:875–910.
4. O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013; 127:e362–e425.
5. Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Steg PG, James SK, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012; 33:2569–2619.
6. Small DS, Kothare P, Yuen E, et al. The pharmacokinetics and pharmacodynamics of prasugrel in healthy Chinese, Japanese, and Korean subjects compared with healthy Caucasian subjects. Eur J Clin Pharmacol. 2010; 66:127–135.
7. Yokoi H, Kimura T, Isshiki T, Ogawa H, Ikeda Y. Pharmacodynamic assessment of a novel P2Y12 receptor antagonist in Japanese patients with coronary artery disease undergoing elective percutaneous coronary intervention. Thromb Res. 2012; 129:623–628.
8. Kim MH, Zhang HZ, Jung DK. Pharmacodynamic comparisons for single loading doses of prasugrel (30 mg) and clopidogrel (600 mg) in healthy Korean volunteers. Circ J. 2013; 77:1253–1259.
9. Zhang HZ, Kim MH, Han JY, Jeong YH. Defining predictive values using three different platelet function tests for CYP2C19 phenotype status on maintenance dual antiplatelet therapy after PCI. Platelets. 2014; 25:285–291.
10. Marcucci R, Gori AM, Paniccia R, et al. High on-treatment platelet reactivity by more than one agonist predicts 12-month follow-up cardiovascular death and non-fatal myocardial infarction in acute coronary syndrome patients receiving coronary stenting. Thromb Haemost. 2010; 104:279–286.
11. Zhang HZ, Kim MH, Jeong YH. Predictive values of post-clopidogrel platelet reactivity assessed by different platelet function tests on ischemic events in East Asian patients treated with PCI. Platelets. 2014; 25:292–299.
12. Park KW, Jeon KH, Kang SH, et al. Clinical outcomes of high on-treatment platelet reactivity in Koreans receiving elective percutaneous coronary intervention (from results of the CROSS VERIFY study). Am J Cardiol. 2011; 108:1556–1563.
13. Ko YG, Suh JW, Kim BH, et al. Comparison of 2 point-of-care platelet function tests, VerifyNow Assay and Multiple Electrode Platelet Aggregometry, for predicting early clinical outcomes in patients undergoing percutaneous coronary intervention. Am Heart J. 2011; 161:383–390.
14. Jin HY, Yang TH, Kim DI, et al. High post-clopidogrel platelet reactivity assessed by a point-of-care assay predicts long-term clinical outcomes in patients with ST-segment elevation myocardial infarction who underwent primary coronary stenting. Int J Cardiol. 2013; 167:1877–1881.
15. Siller-Matula JM, Christ G, Lang IM, Delle-Karth G, Huber K, Jilma B. Multiple electrode aggregometry predicts stent thrombosis better than the vasodilator-stimulated phosphoprotein phosphorylation assay. J Thromb Haemost. 2010; 8:351–359.
16. Tantry US, Bonello L, Aradi D, et al. Consensus and update on the definition of on-treatment platelet reactivity to adenosine diphosphate associated with ischemia and bleeding. J Am Coll Cardiol. 2013; 62:2261–2273.
17. Tsukahara K, Kimura K, Morita S, et al. Impact of high-responsiveness to dual antiplatelet therapy on bleeding complications in patients receiving drug-eluting stents. Circ J. 2010; 74:679–685.
18. Angiolillo DJ, Fernández-Ortiz A, Bernardo E, et al. High clopidogrel loading dose during coronary stenting: effects on drug response and interindividual variability. Eur Heart J. 2004; 25:1903–1910.
19. Jin HY, Yang TH, Choi KN, et al. Randomized comparison of the platelet inhibitory efficacy between low dose prasugrel and standard dose clopidogrel in patients who underwent percutaneous coronary intervention. Korean Circ J. 2014; 44:82–88.
20. Cuisset T, Cayla G, Frere C, et al. Predictive value of post-treatment platelet reactivity for occurrence of post-discharge bleeding after non-ST elevation acute coronary syndrome. Shifting from antiplatelet resistance to bleeding risk assessment? EuroIntervention. 2009; 5:325–329.
21. Serebruany V, Rao SV, Silva MA, et al. Correlation of inhibition of platelet aggregation after clopidogrel with post discharge bleeding events: assessment by different bleeding classifications. Eur Heart J. 2010; 31:227–235.
22. Cayla G, Cuisset T, Silvain J, et al. Prasugrel monitoring and bleeding in real world patients. Am J Cardiol. 2013; 111:38–44.
23. Grosdidier C, Quilici J, Loosveld M, et al. Effect of CYP2C19*2 and *17 genetic variants on platelet response to clopidogrel and prasugrel maintenance dose and relation to bleeding complications. Am J Cardiol. 2013; 111:985–990.
24. Bonello L, Mancini J, Pansieri M, et al. Relationship between post-treatment platelet reactivity and ischemic and bleeding events at 1-year follow-up in patients receiving prasugrel. J Thromb Haemost. 2012; 10:1999–2005.
25. Parodi G, Bellandi B, Venditti F, et al. Residual platelet reactivity, bleedings, and adherence to treatment in patients having coronary stent implantation treated with prasugrel. Am J Cardiol. 2012; 109:214–218.
26. Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007; 357:2001–2015.
27. Roe MT, Armstrong PW, Fox KA, et al. Prasugrel versus clopidogrel for acute coronary syndromes without revascularization. N Engl J Med. 2012; 367:1297–1309.
28. Saito S, Isshiki T, Kimura T, et al. Efficacy and safety of adjusted-dose prasugrel compared with clopidogrel in Japanese patients with acute coronary syndrome: the PRASFIT-ACS study. Circ J. 2014; 78:1684–1692.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download