Abstract
Behçet's disease (BD) is a multisystem vascular inflammatory disease. BD can affect blood vessels of nearly all sizes and types. Arterial involvement is a rare but serious condition in the course of BD. Here, we report a case of stenosis at the iliac artery bifurcation which was treated with percutaneous balloon angioplasty and stent implantation in a 37-year-old patient with BD.
Behçet's disease (BD) is a multisystem inflammatory disorder characterized by recurrent ulcers affecting the mouth and genitals, various skin lesions, and vasculitis.1)2) The prevalence of vascular complications in BD ranges from 6% to 38%.3)4) Vascular involvement can include all types and sizes of blood vessels.5)6) Nevertheless, arteries are less frequently affected than veins, and iliac artery stenosis in BD is very rare. Here, a case of iliac artery bifurcation stenosis treated with stent implantation in a 37-year-old patient with BD is reported.
A 37-year-old man was admitted to our hospital with claudication and progressive, cramp-like pain in both thighs and lower legs. The pain was rated 6-7 on a scale of 1 to 10. In his medical history, he had been diagnosed and treated with deep vein thrombosis and pulmonary embolism 10 years prior. He had been suffering from recurrent painful oral and genital ulcers and migrating erythema nodosum since the age of 30, and he had been diagnosed with BD. However, he had never regularly taken medication for BD. He was a lifelong non-smoker and he did not drink alcohol.
On physical examination, his bilateral femoral, popliteal, tibial, and dorsalis pedis arterial pulses were weakly palpable. There were aphthous ulcers on his buccal mucosa and the inferior surface of his tongue. His blood pressure was 110/80 mm Hg, his heart rate was 80 beats per minute, and his respiration rate was 18 breaths per minute.
On laboratory examination, his white blood cell count was 8700/mm3, hemoglobin was 14.4 g/dL, hematocrit was 43.4%, platelet count was 230000/mm3, and erythrocyte sedimentation rate was 14 mm/h. Activated partial thromboplastin time was 35.6 seconds and prothrombin time was 12.1 seconds. Serum complement levels were normal, there were no anti-nuclear antibodies, and rheumatoid factor was negative.
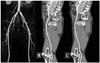
Ankle-brachial index (ABI) was 0.86 on the right side and 0.79 on the left side. Lower extremity computed tomography (CT) angiogram of both legs showed significant stenosis at the aortoiliac bifurcation (Fig. 1). Chest CT angiogram and abdominal CT revealed normal renal and subclavian arteries, and no stenosis in any other arteries.
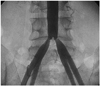
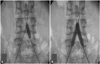
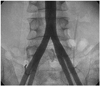
Since the patient was symptomatic and suffering from progressive symptoms, angiography was performed. Aortogram via both femoral arteries showed significant stenosis (90%) at the bifurcation of both aortoiliac arteries (Fig. 2). Percutaneous transluminal angioplasty for aortoiliac bifurcation was performed with two 7×20 mm Synergy balloons (Boston Scientific, Natick, MA, USA) (Fig. 3A) and demonstrated residual stenosis of about 60%. We then performed stent implantation for the common iliac artery bifurcation using two 10×37 mm sized Express stents (Boston Scientific, Natick, MA, USA) (Fig. 3B) simultaneously with a kissing stent technique. The final aortogram showed markedly decreased stenosis at the common iliac artery bifurcation (Fig. 4).
After the intervention, the patient had no pain and the femoral, poplitial, tibial, and dorsalis pedal pulses were improved. Follow-up ABI showed 1.06 on the right side and 0.99 on the left side. The patient was discharged on the third hospital day without any complications. He was prescribed aspirin, clopidogrel, and cilostazol. His ABIs were checked 13 months after intervention, which showed 1.09 on the right side and 1.04 on the left side.
Behçet's disease is common in the Middle East and Central Asia, and it tends to develop in people during their twenties or thirties, however, people of all ages can develop this disease. BD is an autoimmune disease that results from damage to blood vessels throughout the body, although the etiology of BD remains uncertain. It has been speculated that genetics and HLA type, infectious agents, autoantigens, cellular and humoral immunological hyperactivity, endothelial cell dysfunction, and oxidative stress play roles in its causation.4)7) BD has the ability to involve blood vessels of nearly all sizes and types, as well as both veins and arteries. Due to the diversity and size of the blood vessels affected, manifestations of BD may occur at many sites throughout the body. Vasculitis is thought to be an important underlying basis of the pathologic lesions in BD, but the etiology is likely multifactorial.5)8) Perhaps the most unique feature of the vasculitis in BD is the venous vascular involvement thought to be responsible for thrombosis. Regarding arterial involvement in BD, the inflammatory changes in the large arteries are typical of a vasculitis, but the lack of wall thickening, the absence of granulomatous inflammation, and the tendency for aneurysm formation are distinctive.5)
Arterial involvement is a rare but serious condition in the course of BD. The aorta and pulmonary arteries are most commonly invo-lved,3)4) and pseudoaneurysm and aneurysm9)10)11) are typical presentations. Arterial stenosis is thought to be rare in BD, however, a few cases have been reported.12)13)14) BD with multiple artery stenosis15) (branches of aortic arch, abdominal aorta, and left renal artery) was reported in 2001 and BD with subclavian artery stenosis was reported in 2005. Renal artery stenosis with BD was reported in Turkey16) and the patient was treated with angioplasty and stent implantation. Several cases of BD with coronary artery stenosis have been reported. Additionally, BD with right common iliac artery stenosis17) was reported in 2011. Here, our case which presented with BD and iliac artery bifurcation stenosis is the first case of this type reported, to our knowledge. The patient had been suffering from claudication and lower leg cramping. If the patient had no symptoms, medical treatment such as corticosteroids and immunosuppressive agents would be chosen as a therapeutic option. However, due to his persistent symptoms, stent implantation of the iliac arteries was performed as it is an effective treatment and is less invasive with lower morbidity than the open surgical technique.10)18) Long term results of iliac artery stenting is safe and stent patency at 10-year follow-up is adequate.19) After the procedure, he had no pain and ABIs were improved. We checked follow-up ABIs 13 months after intervention, which showed 1.09 on the right side and 1.04 on the left side.
This patient had a history of DVT and pulmonary embolism, and common iliac artery stenosis occurred ten years later. This emphasizes that careful monitoring for vascular complications in BD patients is prudent. Non-invasive angioplasty and stent implantation are appropriate therapeutic choices for occlusive arterial complications of BD.
Figures and Tables
Fig. 1
Computed tomography angiogram showed significant stenosis at the iliac artery bifurcation. R: right, L: left.
References
1. Criteria for diagnosis of Behçet's disease. International Study Group for Behçet's Disease. Lancet. 1990; 335:1078–1080.
2. Behcet H. Some observations on the clinical picture of the so-called triple symptom complex. Dermatologica. 1940; 81:73–83.
3. Düzgün N, Ateş A, Aydintuğ OT, Demir O, Olmez U. Characteristics of vascular involvement in Behçet's disease. Scand J Rheumatol. 2006; 35:65–68.
4. Ideguchi H, Suda A, Takeno M, Ueda A, Ohno S, Ishigatsubo Y. Characteristics of vascular involvement in Behçet's disease in Japan: a retrospective cohort study. Clin Exp Rheumatol. 2011; 29:4 Suppl 67. S47–S53.
5. Melikoglu M, Kural-Seyahi E, Tascilar K, Yazici H. The unique features of vasculitis in Behçet's syndrome. Clin Rev Allergy Immunol. 2008; 35:40–46.
6. Ko GY, Byun JY, Choi BG, Cho SH. The vascular manifestations of Behçet's disease: angiographic and CT findings. Br J Radiol. 2000; 73:1270–1274.
7. Sarica-Kucukoglu R, Akdag-Kose A, KayabalI M, et al. Vascular involvement in Behçet's disease: a retrospective analysis of 2319 cases. Int J Dermatol. 2006; 45:919–921.
8. O'Duffy JD. Vasculitis in Behçet's disease. Rheum Dis Clin North Am. 1990; 16:423–431.
9. Ugurlucan M, Sayin OA, Surmen B, et al. Complication of Behcet's disease: spontaneous aortic pseudoaneurysm. J Card Surg. 2006; 21:589–591.
10. Kaouel K, Mechergui S, Ben Mrad I, et al. [Endovascular treatment of an aneurysm of the abdominal aorta secondary to Behcet's disease]. Tunis Med. 2013; 91:423–424.
11. Cakir O, Eren N, Ulkü R, Nazaroğlu H. Bilateral subclavian arterial aneurysm and ruptured abdominal aorta pseudoaneurysm in Behçet's disease. Ann Vasc Surg. 2002; 16:516–520.
12. Sonia H, Khaldoun BH, Sylvia M, Faouzi M, Habib G, Mohamed BF. Stenosis and aneurysm of coronary arteries in a patient with Behçet's Disease. Open Cardiovasc Med J. 2008; 2:118–120.
13. Park TK, Yang JH, Yoo H, et al. A retrograde approach to coronary ostial stenosis after a bentall procedure in a patient with Behçet's disease. Korean Circ J. 2013; 43:277–280.
14. Drobinski G, Wechsler B, Pavie A, et al. Emergency percutaneous coronary dilatation for acute myocardial infarction in Behçet's disease. Eur Heart J. 1987; 8:1133–1136.
15. Nakamura H, Ueki Y, Horikami K, et al. Vasculo-Behçet's syndrome with widespread arterial involvement. Mod Rheumatol. 2001; 11:332–335.
16. Toprak O, Ersoy R, Uzum A, Memis A, Cirit M, Akpolat T. An unusual vascular involvement in a patient with Behcet's disease: renal artery stenosis. Am J Med Sci. 2007; 334:396–398.
17. Ulusan Z, Karadag AS, Harman A, Boyvat F, Bilgic S. Right common iliac artery stenosis and stent insertion in Behçet's disease. Cardiovasc J Afr. 2011; 22:e4–e6.
18. Tekbas G, Oguzkurt L, Gur S, Onder H, Andic C. Endovascular treatment of veno-occlusive Behcet's disease. Cardiovasc Intervent Radiol. 2012; 35:826–831.
19. Uher P, Nyman U, Lindh M, Lindblad B, Ivancev K. Long-term results of stenting for chronic iliac artery occlusion. J Endovasc Ther. 2002; 9:67–75.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download