Abstract
Background and Objectives
Milrinone is often used in children to treat acute heart failure and prevent low cardiac output syndrome after cardiac surgery. Due to the lack of studies on the long-term milrinone use in children, the objective of this study was to assess the safety and efficacy of the current patterns of milrinone use for ≥3 days in infants and children with heart diseases.
Subjects and Methods
We retrospectively reviewed the medical records of patients aged <13 years who received milrinone for ≥3 days from January 2005 to December 2012. Patients' characteristics including age, sex, height, weight, and body surface area were recorded. The following parameters were analyzed to identify the clinical application of milrinone: initial infusion rate, maintenance continuous infusion rate, total duration of milrinone therapy, and concomitantly infused inotropes. The safety of milrinone was determined based on the occurrence of adverse events such as hypotension, arrhythmia, chest pain, headache, hypokalemia, and thrombocytopenia.
Results
We assessed 730 admissions (684 patients) during this period. Ventricular septal defects were the most common diagnosis (42.4%) in these patients. Milrinone was primarily used after cardiac surgery in 715 admissions (97.9%). The duration of milrinone treatment varied from 3 to 64.4 days (≥7 days in 149 admissions). Ejection fraction and fractional shortening of the left ventricle improved in patients receiving milrinone after cardiac surgery. Dose reduction of milrinone due to hypotension occurred in only 4 admissions (0.5%). Although diverse arrhythmias occurred in 75 admissions (10.3%), modification of milrinone infusion to manage arrhythmia occurred in only 3 admissions (0.4%). Multivariate analysis indicated that the development of arrhythmia was not influenced by the pattern of milrinone use.
Conclusion
Milrinone was generally administered for ≥3 days in children with heart diseases. The use of milrinone for ≥3 days was effective in preventing low cardiac output after cardiac surgery when combined with other inotropes, suggesting that milrinone could be safely employed in pediatric patients with heart diseases.
Milrinone, a phosphodiesterase III inhibitor currently used to treat pediatric patients with cardiac diseases, increases the level of cyclic adenosine monophosphate in the myocardium and vascular smooth muscle. High levels of cyclic adenosine monophosphate enhance the contractility of the myocardium by increasing calcium influx and relaxing vascular smooth muscles,1) therefore increasing cardiac output and decreasing afterload. Milrinone also has a lusitropic property, which improves myocardial relaxation.2) Unlike other inotropes such as dopamine, dobutamine, and epinephrine, milrinone is not associated with an increase in myocardial oxygen consumption.3)
Milrinone is widely used due to its inotropic, vasodilatory, and lusitropic properties. It is frequently prescribed after cardiac surgery due to its efficacy in preventing low cardiac output syndrome.4) Milrinone is also commonly administered to pediatric patients with myocarditis as a bridge therapy for patients with heart failure who are waiting for cardiac transplantation.5)6) Milrinone has been shown to improve heart contractility in patients with septic shock.7)
Milrinone is currently one of the most commonly used off-label cardiovascular medications in children.8) Although a few reports showed the efficacy and safety of short-term milrinone treatment (for about 35 hours) in children with heart disease,9)10) the safety and efficacy of long-term use of milrinone in children is limited due to a lack of sufficient evidence-based studies in pediatric populations. Currently, milrinone is widely used for ≥3 days, which is usually based on extrapolation from studies in adults or clinical experience. Therefore, the objective of this study was to evaluate the safety and efficacy of the current pattern of milrinone administration for ≥3 days in pediatric patients.
A retrospective analysis was conducted using data collected from patients who received milrinone treatment for ≥3 days at the Seoul National University Children's Hospital from January 2005 to December 2012. Patients aged <13 years were included in the study. Patients were divided into two groups based on the indication for milrinone treatment: group A consisted of patients who received milrinone to prevent low cardiac output syndrome after cardiac surgeries whereas group B consisted of patients who received milrinone treatment due to acute heart failures from causes other than cardiac surgeries.
Patients with the following conditions or those who underwent the following treatments were excluded from the study: 1) severe left ventricular outflow obstructive diseases such as aortic stenosis; 2) hypertrophic or restrictive cardiomyopathies; 3) milrinone administration immediately after cardiopulmonary resuscitation; 4) multi-organ failures; 5) simultaneous administration of ≥3 inotropes other than milrinone to increase blood pressure; 6) renal replacement therapies including peritoneal dialysis; 7) myocardial infarctions; 8) univentricular heart surgeries. However, patients receiving ≥3 inotropes were included if inotropes were added after an interval of >2 hours consecutively.
Patients' characteristics including age, sex, height, weight, and body surface area were recorded. The following parameters were analyzed to identify the clinical application of milrinone: 1) initial infusion rate; 2) maintenance continuous infusion rate; 3) total duration of milrinone therapy; 4) concomitantly infused inotropes. The operation and anesthesiology records of patients who had undergone cardiac surgeries were also studied to identify data related to anatomic diagnosis, type of surgery, time of cardiopulmonary bypass, and time of aortic cross-clamping.
Systolic blood pressure, heart rate, and echocardiographic data (the left ventricular internal dimension at end-diastole, ejection fraction, and fractional shortening) obtained before or immediately after starting milrinone treatment were compared to the values prior to treatment cessation. In cases where appropriate echocardiographic data could not be obtained on the day milrinone treatment was discontinued, echocardiographic data obtained within a week of the treatment endpoint were used.
The safety of milrinone was determined based on the occurrence of adverse events such as hypotension, arrhythmia, chest pain, headache, hypokalemia, and thrombocytopenia. Hypotension was defined as a sudden decrease in blood pressure within two hours after starting milrinone that necessitated the addition of inotropes or cessation of milrinone. The documentation of arrhythmias over the entire milrinone treatment period was analyzed. Twelve-lead electrocardiogram and rhythm strips were reviewed. Arrhythmia was classified as supraventricular tachycardia, ectopic atrial tachycardia, atrial fibrillation/flutter, accelerated junctional rhythm, junctional ectopic tachycardia, ventricular tachycardia, or ventricular fibrillation. Evidence of chest pains or headache during milrinone use were collected from the patient's chart. Potassium levels and platelet counts 24 to 48 hours after starting milrinone infusion were estimated. Hypokalemia was defined when serum potassium level of <3.5 mmol/dL. Thrombocytopenia was defined when platelet count of <50000/dL.
Changes in hemodynamic parameters and echocardiographic data were analyzed using a pairwise comparison test and the Wilcoxon signed-rank test. The frequency of hypokalemia and thrombocytopenia after milrinone infusion was analyzed using the McNemar test. Univariate and multivariate logistic regression analysis was used to evaluate the relationships between diverse variables, including the practical use of milrinone and the development of arrhythmia. For statistical analyses, descriptive data are presented as means and standard deviation, whereas categorical variables are presented as proportions. Data manipulation and statistical analyses were performed with Statistical Package for the Social Sciences (SPSS) 19.0 for Windows (SPSS Inc., Somers, NY, USA) and Excel 2010 (Microsoft). Observations with a p of <0.05 were considered statistically significant. The study protocol was approved by the Institutional Review Board of Seoul National University Hospital and patient consent was waived due to the study's retrospective design.
In total, 2299 eligible admissions were identified during the study period. Of these admissions, a total of 730 admissions (684 patients) met the inclusion criteria and were selected for the present study. Twenty-seven patients received milrinone twice and one patient received milrinone thrice after serial cardiac surgeries. Most patients (715, 97.9%) received milrinone to prevent low cardiac output after cardiac surgeries. There were 715 admissions in group A and 15 admissions in group B. The male to female ratio was 5.6:1. The mean age of patients at the time of milrinone infusion was 0.82 years (Table 1). In total, 429 admissions (60%) in group A underwent cardiac surgeries at less than 3 months of age.
The most common cardiac defect was ventricular septal defect in group A (42.4%), followed by tetralogy of Fallot (11%) and coarctation of the aorta with ventricular septal defect (6.4%) (Table 2). Accordingly, the most common type of surgery was closure of the ventricular septal defect, followed by repair of tetralogy of Fallot and coarctoplasty. In group B, 12 patients were diagnosed with a dilated cardiomyopathy and 3 with acute myocarditis.
The duration of milrinone treatment ranged from 3 to 64.4 days. In 149 (20.4%) admissions, patients received milrinone infusion for ≥7 days. The mean initial infusion rate of milrinone was 0.51±0.15 mcg/kg per minute. The mean maintenance continuous infusion rate was 0.51±0.11 mcg/kg per minute. Other inotropes were used in 691 (94.7%) admissions. Two or more inotropes other than milrinone were used in 425 (59.4%) admissions. The most commonly infused inotrope in group A was dopamine (83.4%), whereas all patients in group B received dobutamine (Table 3).
Systolic blood pressure, fractional shortening, and ejection fraction after milrinone treatment were significantly (p<0.05) increased in group A when compared to values obtained immediately after cardiac surgeries. However, there was no significant difference in systolic blood pressure, fractional shortening, and ejection fraction before and after milrinone treatment in group B. In both groups, heart rate was significantly (p<0.05) reduced after milrinone use (Table 4).
There were no reports of adverse events in the majority of admissions (78.7%) (Table 5). Only 4 admissions (0.5%) had dose reduction of milrinone due to hypotension. One patient had complaint of chest pain. Three patients experienced headaches.
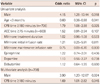
Although diverse arrhythmias occurred in 75 (10.3%) admissions, only 3 (0.4%) required reduction or discontinuation of milrinone infusion to alleviate arrhythmia. Two of them developed junctional ectopic tachycardia and one of them developed ectopic atrial tachycardia. One-third of patients in group B as well as approximately 10% of patients in group A developed arrhythmia. In total, 41 (58.6%) of the 70 arrhythmias in group A were classified as junctional ectopic tachycardia, whereas the most common arrhythmia identified in group B was ventricular tachycardia. The development of arrhythmia was not influenced by the initial infusion rate, maintenance continuous infusion rate, or duration of milrinone treatment. Based on univariate logistic regression analysis of group A data, the following parameters were associated with the development of arrhythmia: male gender, age ≥3 months, and cardiopulmonary bypass time ≥180 minutes. Multivariate analysis of group A data in-dicated that male gender and cardiopulmonary bypass time ≥180 minutes influenced the development of arrhythmia.
The incidence of hypokalemia was not rare. However, the incidence rate did not increase significantly (p=0.390), which was 108/730 (14.4%) at the initial point and 118/730 (16.2%) at 24 to 48 hours after starting milrinone treatment. Thrombocytopenia did increase slightly but significantly (p=0.039), which occurred in 4/729 (0.5%) at the initial point and 12/729 (1.6%) at 24 to 48 hours after starting milrinone treatment. Most patients in group A with thrombocytopenia required only a few platelet transfusions after cardiac surgeries. Platelet count was increased and maintained ≥50000/dL spontaneously in 2 admissions, after 1 platelet transfusion in 6 admissions, and after ≥2 platelet transfusion in 2 admissions. The cardiopulmonary bypass time (249.2±72.8 minutes vs. 153.1±70.4 minutes; p=0.000) and aorta cross-clamping time (141.1±59.9 minutes vs. 85.6±42.1 minutes; p=0.004) were significantly longer in group A patients with thrombocytopenia than in patients without thrombocytopenia. The initial infusion rate, maintenance continuous infusion rate, and duration of milrinone treatment were not associated with thrombocytopenia. Two patients in group B had a low platelet count due to additional medical illnesses such as hemophagocytic lymphohistiocytosis and fungal infection.
In the present study, we reviewed the current patterns of milrinone use that continued for ≥3 days. We also evaluated the efficacy and safety of such treatment in pediatric patients. Of a total of 2299 eligible admissions in which milrinone was used, 730 (31.8%) admissions involved the use of milrinone for ≥3 days. The mean duration of milrinone use was 6.1±4.5 days. Although the Korean national insurance covers only 35 hours of milrinone use, we found that milrinone was frequently prescribed for a longer duration in actual settings, suggesting a significant off-label use.
Most (97.9%) admissions involved patients who received milrinone after cardiac surgeries. The frequent use of milrinone in pediatric patients undergoing heart surgery was supported by the findings of the Prophylactic Intravenous use of Milrinone After Cardiac Operation in Pediatrics (PRIMACORP) trial, which demonstrated that low cardiac output syndromes could be prevented by high-dose milrinone infusion after pediatric cardiac surgeries.10) Although the initial and maintenance milrinone infusion rates determined in the present study were lower than those previously reported in the PRIMACORP study, our values were similar to those reported in other European practices.4)10)
In terms of efficacy issue, fractional shortening and ejection fraction were both improved after milrinone infusion in group A patients, which is in consistent with previous findings.9)11) Chang et al.9) reported that milrinone treatment in neonates with low cardiac output after congenital heart surgery improved the cardiac index without changing myocardial oxygen consumption. Duggal et al.11) documented that milrinone therapy improved the left and right myocardial performance index, a reliable index that reflects myocardial contractility.
Our findings revealed no significant changes in fractional shortening and ejection fraction after milrinone infusion in group B, which is in contrary to previously reported data in adults.12) The severity of the disease in group B is likely to have some influence on the results. Seven (46.7%) of the 15 admissions in group B involved patients who died due to underlying cardiac disease itself, reflecting the severity of disease in group B.
In terms of safety, several adult studies have shown detrimental effects of milrinone on hemodynamic stability in chronic heart failures. The Prospective Randomized Milrinone Survival Evaluation13) trial revealed that oral administration of milrinone to patients with heart failure increased mortality and induced serious adverse cardiovascular events including hypotension. The Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure trial reported that sustained hypotension requiring additional treatment was more common in patients who received milrinone infusion for exacerbation of chronic heart failure.14) However, in the present study, only 1 (6.7%) of 15 admissions in group B needed a reduction in milrinone dose due to a decrease in blood pressure, with the incidence of hypotension being lower than that reported previously in adult data. Furthermore, only 3 (0.4%) of the 715 admissions in group A experienced hypotension that required a reduction in milrinone infusion rate. This result was in consistent with previous pediatric data that reported an infrequent occurrence of hypotension in the milrinone treatment group after cardiac surgery.10)
Milrinone use has been known to be associated with postoperative arrhythmia in adults that increased mortality and morbidity after cardiac surgery.15) Arrhythmia is a concern following milrinone use in the pediatric population as well. Smith et al.16) recently reported that approximately half of the pediatric patients receiving milrinone after cardiac surgery experienced arrhythmia. In the present study, various arrhythmias occurred in 70 (9.8%) of 715 admissions in group A. However, only 3 (0.4%) admissions required modification of milrinone infusion to manage arrhythmias. Our finding is in consistent with that from other studies,17)18) indicating that the incidence of arrhythmia due to milrinone use in pediatric patients is relatively low after cardiac surgery.
It should be noted that postoperative arrhythmias are common after cardiac surgery. Postoperative arrhythmia is associated with age, cardiopulmonary time, aortic cross clamping time, and type of repair.19)20) In the present study, the initial infusion rate, maintenance infusion rate, and duration of milrinone treatment were not associated with the development of arrhythmia. However, in consistent with the previous findings, a longer cardiopulmonary time affected the development of arrhythmia in group A (Table 6).
Junctional ectopic tachycardia is the most common type of arrhythmia after cardiac surgery.20) In the present study, the incidence rate of junctional ectopic tachycardia in group A was 5.7%. This result is in accordance with previous studies, which reported that the incidence rate of junctional ectopic tachycardia after cardiac surgery range from 1.4% to 14.7%.21)22) The relationship between junctional ectopic tachycardia and milrinone use has not been elucidated thus far.23)
A study in adults showed that atrial arrhythmia developed more frequently in patients with chronic heart failure who received milrinone treatment.14) However, the independent cause-effect relationship of milrinone with arrhythmia in pediatric patients with heart failure has not yet been established. Five (33.3%) of the 15 admissions in group B involved patients who mainly developed ventricular arrhythmia. In the present study, there was no significant difference in initial infusion rate, maintenance infusion rate, or duration of milrinone treatment between patients with or without arrhythmia in group B. In fact, heart failure due to myocarditis or dilated cardiomyopathy itself increased the vulnerability of the patients to tachyarrhythmia and conduction disturbance.24) Ichikawa et al.25) reported that 3 of 7 patients with fulminant myocarditis developed ventricular tachycardia or ventricular fibrillation. Friedman et al.26) also documented the high incidence rate of arrhythmia in pediatric idiopathic dilated cardiomyopathy.
The incidence rate of thrombocytopenia in the present study was lower than that in previous studies. Ten (1.4%) of the 715 admissions in group A involved patients who developed thrombocytopenia after milrinone treatment, which required a few platelet transfusions. Ramamoorthy et al.17) previously reported that milrinone treatment resulted in a high incidence (58%) of thrombocytopenia (platelet count <100000/dL) that did not often necessitate platelet transfusions. Bishara et al.18) further documented that 12.7% of admissions developed thrombocytopenia with milrinone treatment. However, it is difficult to identify milrinone-induced thrombocytopenia, because various factors could confound the observations, including the cardiac surgery itself.
Cardiopulmonary bypass is known to be associated with thrombocytopenia that results from hemodilution and mechanical disruption.27) In the present study, patients who developed thrombocytopenia had a longer cardiopulmonary bypass time and aorta-clamping time. Thus, patients with a more complex heart disease and longer bypass times during cardiac surgery would be more likely to develop thrombocytopenia. In contrast to amrinone, the first phosphodiesterase inhibitor used that was known to have adverse effect on platelets, milrinone did not alter platelet count or function in patients after cardiac surgery.28) The fact that two (13.3%) patients in group B developed thrombocytopenia could be due to complications such as hemophagocytic lymphohistiocytosis and fungal sepsis, rather than due to milrinone use.
Few studies have sufficiently investigated long-term milrinone use thus far. The utility of chronic continuous milrinone infusion for heart failure as bridge therapy to heart transplantation was proposed in a recent adult study.6) McMahon et al.29) demonstrated that long-term support with milrinone was safe and effective in infants with cardiomyopathy awaiting heart transplantation. Outpatient continuous parenteral inotropic therapy, including milrinone, has also been used in inotropic-dependent children with advanced heart failure.30) Although these studies used small patient populations, the incidence of complications was sufficiently low to indicate the safe and effective potential of milrinone use in infants and children with heart diseases.
This study has several possible limitations. This study had a retrospective design which did not have a control group containing patients who did not receive milrinone. Moreover, all arrhythmias could not be included due to the study's retrospective nature. Furthermore, because the exclusion criteria of this study were relatively strict to appropriately clarify the efficacy and safety of milrinone use and reduce confounding factors, the patients who would be more susceptible to milrinone use could not be included. In surgically treated patients with congenital heart disease, we should have also considered the natural improvement of cardiac function after the corrective operation, which could be a confounding factor for evaluating the efficacy of milrinone use in this study. Finally, only a few echocardiographic data including ejection fraction and fractional shortening were used to evaluate milrinone efficacy due to the retrospective study design. If other echocardiographic data, such as tissue Doppler imaging findings, were available, a more accurate evaluation of the hemodynamic effects of milrinone would have been possible.
This is the largest retrospective study, to date, to evaluate the safety and efficacy of long-term milrinone use (≥3 days) in pediatric patients with cardiac diseases. Such long-term milrinone use is common in actual clinical practice, and milrinone is generally used for >35 hours in infants and children with heart disease. Our data revealed that the use of milrinone for ≥3 days was effective in preventing low cardiac output after cardiac surgery when combined with other inotropes. Therefore, milrinone could be safely used in pediatric patients with heart diseases.
Figures and Tables
Table 1
Demographic data of subjects used in this study
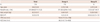
Table 2
List of congenital heart diseases treated by cardiac surgeries in the 715 admissions included in group A

Table 3
Milrinone use patterns in study subjects
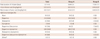
Table 4
Hemodynamic measurements before and after milrinone use

Table 5
Adverse events that occurred during inotropic treatment (including milrinone)
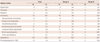
Table 6
Variables related to postoperative arrhythmia in group A
Acknowledgments
This study was supported by a 2012 grant (12172MFDS231) from Ministry of Food and Drug safety.
References
1. Colucci WS. Cardiovascular effects of milrinone. Am Heart J. 1991; 121(6 Pt 2):1945–1947.
2. Monrad ES, McKay RG, Baim DS, et al. Improvement in indexes of diastolic performance in patients with congestive heart failure treated with milrinone. Circulation. 1984; 70:1030–1037.
3. Monrad ES, Baim DS, Smith HS, Lanoue A, Brauwald E, Grossman W. Effects of milrinone on coronary hemodynamics and myocardial energetics in patients with congestive heart failure. Circulation. 1985; 71:972–979.
4. Vogt W, Läer S. Drug use patterns for the prevention of paediatric low cardiac output syndrome in Europe. Intensive Care Med. 2011; 37:1390–1391.
5. Klugman D, Berger JT, Sable CA, He J, Khandelwal SG, Slonim AD. Pediatric patients hospitalized with myocarditis: a multi-institutional analysis. Pediatr Cardiol. 2010; 31:222–228.
6. Assad-Kottner C, Chen D, Jahanyar J, et al. The use of continuous milrinone therapy as bridge to transplant is safe in patients with short waiting times. J Card Fail. 2008; 14:839–843.
7. Lindsay CA, Barton P, Lawless S, et al. Pharmacokinetics and pharmacodynamics of milrinone lactate in pediatric patients with septic shock. J Pediatr. 1998; 132:329–334.
8. Pasquali SK, Hall M, Slonim AD, et al. Off-label use of cardiovascular medications in children hospitalized with congenital and acquired heart disease. Circ Cardiovasc Qual Outcomes. 2008; 1:74–83.
9. Chang AC, Atz AM, Wernovsky G, Burke RP, Wessel DL. Milrinone: systemic and pulmonary hemodynamic effects in neonates after cardiac surgery. Crit Care Med. 1995; 23:1907–1914.
10. Hoffman TM, Wernovsky G, Atz AM, et al. Efficacy and safety of milrinone in preventing low cardiac output syndrome in infants and children after corrective surgery for congenital heart disease. Circulation. 2003; 107:996–1002.
11. Duggal B, Pratap U, Slavik Z, Kaplanova J, Macrae D. Milrinone and low cardiac output following cardiac surgery in infants: is there a direct myocardial effect? Pediatr Cardiol. 2005; 26:642–645.
12. Seino Y, Momomura S, Takano T, Hayakawa H, Katoh K. Multicenter, double-blind study of intravenous milrinone for patients with acute heart failure in Japan. Japan Intravenous Milrinone Investigators. Crit Care Med. 1996; 24:1490–1497.
13. Packer M, Carver JR, Rodeheffer RJ, et al. The PROMISE Study Research Group. Effect of oral milrinone on mortality in severe chronic heart failure. N Engl J Med. 1991; 325:1468–1475.
14. Cuffe MS, Califf RM, Adams KF Jr, et al. Short-term intravenous milrinone for acute exacerbation of chronic heart failure: a randomized controlled trial. JAMA. 2002; 287:1541–1547.
15. Fleming GA, Murray KT, Yu C, et al. Milrinone use is associated with postoperative atrial fibrillation after cardiac surgery. Circulation. 2008; 118:1619–1625.
16. Smith AH, Owen J, Borgman KY, Fish FA, Kannankeril PJ. Relation of milrinone after surgery for congenital heart disease to significant postoperative tachyarrhythmias. Am J Cardiol. 2011; 108:1620–1624.
17. Ramamoorthy C, Anderson GD, Williams GD, Lynn AM. Pharmacokinetics and side effects of milrinone in infants and children after open heart surgery. Anesth Analg. 1998; 86:283–289.
18. Bishara T, Seto WT, Trope A, Parshuram CS. Use of milrinone in critically ill children. Can J Hosp Pharm. 2010; 63:420–428.
19. Delaney JW, Moltedo JM, Dziura JD, Kopf GS, Snyder CS. Early postoperative arrhythmias after pediatric cardiac surgery. J Thorac Cardiovasc Surg. 2006; 131:1296–1300.
20. Grosse-Wortmann L, Kreitz S, Grabitz RG, et al. Prevalence of and risk factors for perioperative arrhythmias in neonates and children after cardiopulmonary bypass: continuous holter monitoring before and for three days after surgery. J Cardiothorac Surg. 2010; 5:85.
21. Zampi JD, Hirsch JC, Gurney JG, et al. Junctional ectopic tachycardia after infant heart surgery: incidence and outcomes. Pediatr Cardiol. 2012; 33:1362–1369.
22. Makhoul M, Oster M, Fischbach P, Das S, Deshpande S. Junctional ectopic tachycardia after congenital heart surgery in the current surgical era. Pediatr Cardiol. 2013; 34:370–374.
23. Hoffman TM, Bush DM, Wernovsky G, et al. Postoperative junctional ectopic tachycardia in children: incidence, risk factors, and treatment. Ann Thorac Surg. 2002; 74:1607–1611.
24. Miyake CY, Teele SA, Chen L, et al. In-hospital arrhythmia development and outcomes in pediatric patients with acute myocarditis. Am J Cardiol. 2014; 113:535–540.
25. Ichikawa R, Sumitomo N, Komori A, et al. The follow-up evaluation of electrocardiogram and arrhythmias in children with fulminant myocarditis. Circ J. 2011; 75:932–938.
26. Friedman RA, Moak JP, Garson A Jr. Clinical course of idiopathic dilated cardiomyopathy in children. J Am Coll Cardiol. 1991; 18:152–156.
27. Weerasinghe A, Taylor KM. The platelet in cardiopulmonary bypass. Ann Thorac Surg. 1998; 66:2145–2152.
28. Kikura M, Lee MK, Safon RA, Bailey JM, Levy JH. The effects of milrinone on platelets in patients undergoing cardiac surgery. Anesth Analg. 1995; 81:44–48.
29. McMahon CJ, Murchan H, Prendiville T, Burch M. Long-term support with milrinone prior to cardiac transplantation in a neonate with left ventricular noncompaction cardiomyopathy. Pediatr Cardiol. 2007; 28:317–318.
30. Price JF, Towbin JA, Dreyer WJ, et al. Outpatient continuous parenteral inotropic therapy as bridge to transplantation in children with advanced heart failure. J Card Fail. 2006; 12:139–143.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download