Abstract
Background and Objectives
Contrast-induced nephropathy (CIN) is associated with increased morbidity and mortality. This observational, non-randomized study evaluated the effect of rosuvastatin loading before percutaneous coronary intervention (PCI) on the incidence of CIN in patients with acute coronary syndrome (ACS).
Subjects and Methods
A total of 824 patients who underwent PCI for ACS were studied (408 patients in the statin group=40 mg rosuvastatin loading before PCI; 416 patients of control group=no statin pretreatment). Serum creatinine concentrations were measured before and 24 and 48 hours after PCI. The primary endpoint was development of CIN defined as an increase in serum creatinine concentration of ≥0.5 mg/dL or ≥25% above baseline within 72 hours after PCI.
Results
The incidence of CIN was significantly lower in the statin group than that in the control group (18.8% vs. 13.5%, p=0.040). The maximum percent changes in serum creatinine and estimated glomerular filtration rate in the statin group within 48 hours were significantly lower than those in the control group (5.84±22.59% vs. 2.43±24.49%, p=0.038; -11.44±14.00 vs. -9.51±13.89, p=0.048, respectively). The effect of rosuvastatin on preventing CIN was greater in the subgroups of patients with diabetes, high-dose contrast medium, multivessel stents, high baseline C-reactive protein, and myocardial infarction. A multivariate analysis revealed that rosuvastatin loading was independently associated with a decreased risk for CIN (odds ratio, 0.64; 95% confidence interval, 0.43-0.95, p=0.026).
With an increasing number of patients undergoing coronary angiography and percutaneous coronary intervention (PCI), the prevalence of contrast-induced nephropathy (CIN) is also increasing. Patients with acute coronary syndrome (ACS) have a three-fold higher risk of developing CIN, and CIN is associated with prolonged hospitalization, increased costs, and increased short- and long-term morbidity and mortality.1) Although the underlying mechanism of CIN is not fully understood, the pathophysiology may be related to direct renal tubular toxicity, vasoconstriction, and high oxidative stress.2)3)
Several studies have suggested that statins may reduce the incidence of CIN through their beneficial effects on endothelial function, nitric oxide production, and oxidative stress.1)3) However, the results of clinical studies are inconsistent.4)
Therefore, we conducted an observational study involving consecutive patients with ACS who underwent PCI. The purpose of this study was to evaluate the effect of pretreatment with rosuvastatin loading before PCI on the incidence of CIN in patients with ACS.
We analyzed a single center, consecutive ACS and PCI cohort from December 2009 to December 2012. During the study period, 1037 consecutive patients were recruited and followed-up during their clinical course to document patient characteristics, acute therapy, PCI data, and hospital outcomes. Exclusion criteria were current statin treatment, high-risk features warranting emergency coronary angiography (within 2 hours), acute renal failure or end-stage renal disease requiring dialysis, serum creatinine >3 mg/dL, contrast medium administration within the past 10 days, or lack of laboratory data including serum creatinine. As a result, 824 patients were analyzed: 408 patients received 40 mg rosuvastatin loading before PCI (statin group) and 416 patients did not receive the statin pretreatment (control group). Rosuvastatin loading was performed at the on-call physician's discretion. All patients gave informed consent for processing of their anonymous data, according to a protocol approved by the Institutional Review Board of Wonkwang University Hospital.
Aspirin (300 mg/day) and clopidogrel (300 mg/day) were loaded in all patients before the procedure. An intravenous bolus of 5000 U unfractionated heparin was given, and additional heparin boluses were given to maintain activated clotting time >300 seconds during the procedure. Coronary angiography and stent implantation were performed using standard interventional techniques. Platelet glycoprotein IIb/IIIa inhibitors were administered according to operator preference. Aspirin (100 mg/day), clopidogrel (75 mg/day), and statins were prescribed to all patients after the procedure.
Hydration therapy (0.9% sodium chloride, 1 mL/kg/h) was performed during the pre- and post-PCI periods at the physician's discretion. Hydration rate was reduced to 0.5 mL/kg/h for patients with a left ventricular ejection fraction (EF) <40%.
Blood samples were taken to measure serum creatinine concentrations before rosuvastatin loading and at 24 and 48 hours after contrast media administration. Additional samples were obtained if a patient showed signs or symptoms of CIN. The peak post-procedural serum creatinine value was used for the primary endpoint evaluation. Renal function was measured using estimated glomerular filtration rate (eGFR), calculated with the Modification of Diet in Renal Disease formula, in all patients.5) Levels of high-sensitivity C-reactive protein (hsCRP) and lipid profiles were also measured using commercial kits.
The primary endpoint was development of CIN, defined as an increase in serum creatinine concentration ≥0.5 mg/dL or ≥25% above baseline within 72 hours after contrast agent administration.6) Additional endpoints included maximal increases in serum creatinine levels and maximal decreases in eGFR within 48 hours after the procedure.
Based on a previous study, the incidence of CIN was approximately 15% in the control group.7) Sample size was selected to demonstrate an incidence reduction of 2% in the statin group. Accordingly, a minimal sample size of 135 patients was required in each group to provide 80% power with a two-sided alpha of 0.05.
All measurements are represented as means±standard deviations or absolute numbers (percentages). The inter-group analysis was performed using the independent t-test and χ2 test, which were conducted using SPSS 19.0 for Windows (SPSS Inc., Chicago, IL, USA). A multivariate logistic regression model was constructed to predict the development of CIN. The following variables, selected according to a significant univariate analysis (p<0.1), were inserted into the logistic regression analysis; rosuvastatin loading, age, diabetes, levels of hemoglobin and hsCRP, contrast volume, myocardial infarction presentation, baseline eGFR, and EF. The efficacy of rosuvastatin was also evaluated in pre-specified subgroups (age, gender, EF, diabetes, contrast dose, multivessel stent, myocardial infarction presentation, and baseline hsCRP and eGFR levels). The first or third tertile of the continuous variables was used as a cut-off point in the logistic regression analysis. The adjust effect was controlled for the same prognostic and confounding factors, but the specific variable related to each individual subgroup was excluded from the model for that subgroup. Statistical significance was set at p<0.05.
The baseline clinical characteristics of the patients in the control and statin groups are shown in Table 1. Risk factors, baseline laboratory findings, and angiographic and procedural data were similar between the groups. However, the control group showed lower EF (51.4±12.9% vs. 54.4±11.9%, p=0.001), higher levels of low density lipoprotein-cholesterol (118.3±37.0 mg/dL vs. 109.4±35.0 mg/dL, p=0.001), and a lower incidence of myocardial infarction (42.1% vs. 51.7%, p=0.006) than those in the statin group.
Contrast-induced nephropathy occurred in 133 patients (16.1%). The incidence of CIN was significantly lower in the statin group than that in the control group (18.8% vs. 13.5%, p=0.040) (Fig. 1). The incidence of increased serum creatinine concentrations ≥0.5 mg/dL and an increase ≥25% above baseline within 72 hours was also lower in the statin group (8.2% vs. 4.7%, p=0.040; 18.5% vs. 13.5%, p=0.049, respectively) than those in the control group. When the patients were divided into three groups according to baseline hsCRP <1.0 mg/L, 1.0-3.0 mg/L, and >3.0 mg/L, the incidence rates of CIN were 10.7%, 16.1%, and 21.6%, respectively (p=0.002).
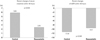
The maximal percent changes in serum creatinine concentration and eGFR in the statin group within 48 hours were significantly lower than those in the control group (5.84±22.59% vs. 2.43±24.49%, p=0.038; -11.44±14.00 vs. -9.51±13.89, p=0.048, respectively) (Fig. 2).
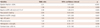
The multivariate analysis revealed that rosuvastatin loading was independently associated with a decreased risk for CIN (odds ratio, 0.64; 95% confidence interval, 0.43-0.95, p=0.026) (Table 2). The independent predictors of CIN included low EF, diabetes, age, and a decreased baseline eGFR.
The benefit of rosuvastatin loading therapy was not different according to age, gender, EF, or hemoglobin level. However, the effect of rosuvastatin on preventing CIN was augmented in the subgroups of patients with diabetes, high contrast doses, multivessel stents, high baseline hsCRP levels, and myocardial infarction. In contrast, the effect of the statin was attenuated in the subgroup with a low baseline eGFR (Fig. 3).
We demonstrated that rosuvastatin loading before PCI was associated with a significantly lower incidence of CIN in patients with ACS. This result is of clinical significance because CIN is an independent risk for adverse short- and long-term outcomes.
The benefits of statins in cardiovascular diseases can be explained not only by their lipid-lowering potential but also by non-lipid-related mechanisms or so-called pleiotropic effects.8) The pleiotropic effects encompass non-lipid-related mechanisms that modify endothelial function, inflammatory responses, and thrombus formation.9) Given their pleiotropic effects, statins could reduce acute iatrogenic renal injury, following iodinated contrast medium admi-nistration.1) However, the results of studies and meta-analyses of short-term high-dose statin administration before contrast injection have been disappointing.4)10)11)
Although the pathogenesis of CIN is unclear, inflammation plays an important role. In our results, the incidence of CIN increased strikingly with increasing baseline hsCRP level. Therefore, a potent statin with potent anti-inflammatory effects may be more beneficial than one with less potent anti-inflammatory effects. However, the results of lipophilic statin use on preventing CIN are inconsistent. Xinwei et al.12) reported that high-dose simvastatin (80 mg) was more effective than low-dose simvastatin (20 mg) in protecting against renal dysfunction after PCI. Similarly, Quintavalle et al.13) reported that high-dose atorvastatin (80 mg) administered within 24 hours before contrast injection was effective for reducing the incidence of CIN. However, other studies using simvastatin and atorvastatin failed to demonstrate a beneficial effect on preventing CIN.4)11)
Two prospective trials showed the protective effects of rosuvastatin on CIN. Leoncini et al.14) reported that high-dose rosuvastatin (40 mg) administered before PCI prevented CIN in patients with non-ST-segment elevation ACS. Han et al.15) also reported that a 5-day rosuvastatin treatment significantly reduced the risk of CIN in patients with diabetes and chronic kidney disease undergoing contrast medium injection. Our results confirm and extend these data on the beneficial effect of rosuvastatin.
Rosuvastatin is a potent hydrophilic statin with acute pleiotrophic effects.16) Rosuvastatin loading therapy before PCI shows several beneficial effects, including reduced periprocedural myonecrosis, improved clinical outcome, and reduced infarct size.17)18)19) This statin also has beneficial clinical effects in patients with eGFR <60 mL/min/1.73 m2.20) Short-term treatment with rosuvastatin may improve eGFR, independent of lipid changes, suggesting a pleiotropic mechanism of action that provides beneficial renal effects.21) Furthermore, rosuvastatin has particularly potent inhibitory activity against 3-hydroxy-3-methylglutaryl-coenzyme A reductase, reducing renal tubular protein reabsorption and preventing lipid accumulation in renal tubules.22)23) In the present study, high-dose rosuvastatin loading reduced the incidence of CIN by 36%, with an absolute reduction of 5.3%. However, the effect of the statin was attenuated in the subgroup with a low baseline eGFR, particularly in patients with eGFR <60 mL/min/1.73 m2 who showed poorer outcomes than those with a higher eGFR. Therefore, use of high-dose rosuvastatin in patients with chronic kidney disease should be considered.
In our results, the benefit of a statin on CIN prevention was distinct in patients with evidence of high inflammatory status such as myocardial infarction or high baseline hsCRP levels. Statins decrease the inflammatory response during PCI, as reflected by decreased hsCRP levels.18)24) As inflammation is a pathogenic factor of kidney injury, decreasing systemic inflammation and hsCRP levels might be part of the mechanism explaining the reduced CIN incidence after rosuvastatin loading. However, we could not conclude this because hsCRP was not measured serially after PCI. Further study is needed to clarify the mechanism.
Our study had several limitations. This study was not randomized, and the sample size was small. We may have underestimated the incidence of CIN because we did not check routine serum creatinine 72 hours after PCI. Moreover, routine hydration could not be carried out. These discrepancies should be considered in future investigations. We did not address other important variables related to CIN, such as hydration volume, urine output, hemodynamic parameters, and nephrotoxic medications. This is a major limitation of our study.
In conclusion, high-dose rosuvastatin loading before PCI was associated with a significantly lower incidence of CIN in patients with ACS. The protective effect of this statin seems be prominent in patients with high inflammatory status.
Figures and Tables
Fig. 1
Incidence of contrast-induced nephropathy. The incidence of the primary endpoint was significantly lower in the rosuvastatin group than that in the control group (13.5% vs. 18.8%, p=0.040). OR: odds ratio, CI: confidence interval.
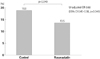
Fig. 3
Odds ratios (OR) for the occurrence of contrast-induced nephropathy in specific risk subgroups. CI: confidence interval, hsCRP: high-sensitivity C-reactive protein, MI: myocardial infarction, UAP: unstable angina pectoris, eGFR: estimated glomerular filtration rate.
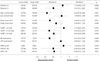
Table 1
Baseline characteristics
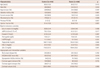
MI: myocardial infarction, PCI: percutaneous coronary intervention, eGFR: estimated glomerular filtration rate, hsCRP: high-sensitivity C-reactive protein, HDL: high density lipoprotein-cholesterol, LDL-C: low density lipoprotein-cholesterol, ACC/AHA: American College of Cardiology/American Heart Association lesion classification
Table 2
Predictive factors for contrast-induced nephropathy after percutaneous coronary intervention according to a multivariate analysis
References
1. McCullough PA. Contrast-induced acute kidney injury. J Am Coll Cardiol. 2008; 51:1419–1428.
2. Giusti-Paiva A, Martinez MR, Felix JV, et al. Simvastatin decreases nitric oxide overproduction and reverts the impaired vascular responsiveness induced by endotoxic shock in rats. Shock. 2004; 21:271–275.
3. Wong PC, Li Z, Guo J, Zhang A. Pathophysiology of contrast-induced nephropathy. Int J Cardiol. 2012; 158:186–192.
4. Jo SH, Koo BK, Park JS, et al. Prevention of radiocontrast medium-induced nephropathy using short-term high-dose simvastatin in patients with renal insufficiency undergoing coronary angiography (PROMISS) trial--a randomized controlled study. Am Heart J. 2008; 155:499.e1–499.e8.
5. Levey AS, Coresh J, Balk E, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003; 139:137–147.
6. Budano C, Levis M, D'Amico M, et al. Impact of contrast-induced acute kidney injury definition on clinical outcomes. Am Heart J. 2011; 161:963–971.
7. Dangas G, Iakovou I, Nikolsky E, et al. Contrast-induced nephropathy after percutaneous coronary interventions in relation to chronic kidney disease and hemodynamic variables. Am J Cardiol. 2005; 95:13–19.
8. Takemoto M, Liao JK. Pleiotropic effects of 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitors. Arterioscler Thromb Vasc Biol. 2001; 21:1712–1719.
9. Sposito AC, Chapman MJ. Statin therapy in acute coronary syndromes: mechanistic insight into clinical benefit. Arterioscler Thromb Vasc Biol. 2002; 22:1524–1534.
10. Pappy R, Stavrakis S, Hennebry TA, Abu-Fadel MS. Effect of statin therapy on contrast-induced nephropathy after coronary angiography: a meta-analysis. Int J Cardiol. 2011; 151:348–353.
11. Toso A, Maioli M, Leoncini M, et al. Usefulness of atorvastatin (80 mg) in prevention of contrast-induced nephropathy in patients with chronic renal disease. Am J Cardiol. 2010; 105:288–292.
12. Xinwei J, Xianghua F, Jing Z, et al. Comparison of usefulness of simvastatin 20 mg versus 80 mg in preventing contrast-induced nephropathy in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Am J Cardiol. 2009; 104:519–524.
13. Quintavalle C, Fiore D, De Micco F, et al. Impact of a high loading dose of atorvastatin on contrast-induced acute kidney injury. Circulation. 2012; 126:3008–3016.
14. Leoncini M, Toso A, Maioli M, Tropeano F, Villani S, Bellandi F. Early high-dose rosuvastatin for contrast-induced nephropathy prevention in acute coronary syndrome: results from the PRATO-ACS Study (Protective Effect of Rosuvastatin and Antiplatelet Therapy On contrast-induced acute kidney injury and myocardial damage in patients with Acute Coronary Syndrome). J Am Coll Cardiol. 2014; 63:71–79.
15. Han Y, Zhu G, Han L, et al. Short-term rosuvastatin therapy for prevention of contrast-induced acute kidney injury in patients with diabetes and chronic kidney disease. J Am Coll Cardiol. 2014; 63:62–70.
16. Liuni A, Luca MC, Gori T, Parker JD. Rosuvastatin prevents conduit artery endothelial dysfunction induced by ischemia and reperfusion by a cyclooxygenase-2-dependent mechanism. J Am Coll Cardiol. 2010; 55:1002–1006.
17. Yun KH, Jeong MH, Oh SK, et al. The beneficial effect of high loading dose of rosuvastatin before percutaneous coronary intervention in patients with acute coronary syndrome. Int J Cardiol. 2009; 137:246–251.
18. Yun KH, Oh SK, Rhee SJ, Yoo NJ, Kim NH, Jeong JW. 12-month follow-up results of high dose rosuvastatin loading before percutaneous coronary intervention in patients with acute coronary syndrome. Int J Cardiol. 2011; 146:68–72.
19. Kim JW, Yun KH, Kim EK, et al. Effect of high dose rosuvastatin loading before primary percutaneous coronary intervention on infarct size in patients with ST-segment elevation myocardial infarction. Korean Circ J. 2014; 44:76–81.
20. Ridker PM, MacFadyen J, Cressman M, Glynn RJ. Efficacy of rosuvastatin among men and women with moderate chronic kidney disease and elevated high-sensitivity C-reactive protein: a secondary analysis from the JUPITER (Justification for the Use of Statins in Prevention-an Intervention Trial Evaluating Rosuvastatin) trial. J Am Coll Cardiol. 2010; 55:1266–1273.
21. Vidt DG, Harris S, McTaggart F, Ditmarsch M, Sager PT, Sorof JM. Effect of short-term rosuvastatin treatment on estimated glomerular filtration rate. Am J Cardiol. 2006; 97:1602–1606.
22. Agarwal R. Statin induced proteinuria: renal injury or renoprotection? J Am Soc Nephrol. 2004; 15:2502–2503.
23. Gotoh K, Masaki T, Chiba S, et al. Effects of hydrophilic statins on renal tubular lipid accumulation in diet-induced obese mice. Obes Res Clin Pract. 2013; 7:e342–e352.
24. Yun KH, Shin IS, Shin SN, et al. Effect of previous statin therapy in patients with acute coronary syndrome and percutaneous coronary intervention. Korean Circ J. 2011; 41:458–463.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download