Abstract
Background and Objectives
Metabolic syndrome and high sodium intake are associated with frequent cardiovascular events. Few studies have estimated sodium intake in subjects with metabolic syndrome by 24-hour urine sodium excretion. We evaluated sodium intake in individuals with metabolic syndrome.
Subjects and Methods
Participants were recruited by random selection and through advertisement. Twenty four-hour urine collection, ambulatory blood pressure measurements, and blood test were performed. Sodium intake was estimated by 24-hour urine sodium excretion. Participants receiving antihypertensive medications were excluded from analysis.
Results
Among the 463 participants recruited, subjects with metabolic syndrome had higher levels of 24-hour urine sodium excretion than subjects without metabolic syndrome (p=0.0001). There was a significant relationship between the number of metabolic syndrome factors and 24-hour urine sodium excretion (p=0.001). The proportion of subjects with metabolic syndrome was increased across the tertile groups of 24-hour urine sodium excretion (p<0.0001). The association of high sodium intake and metabolic syndrome was significant only among women. Among the factors related to metabolic syndrome, body mass index had an independent association with 24-hour urine sodium excretion (p<0.0001).
High sodium intake increases blood pressure (BP),1) and eventually leads to a high incidence of cardiovascular events.2)3) Conversely, reductions in sodium intake lowers BP.4)5) In the Dietary Approaches to Stop Hypertension (DASH)-sodium trial, the BP lowering effect of low sodium diet was additive to the effects of DASH diet. Thus, a reduction in sodium intake is the milestone in the management of hypertension.
In addition to hypertension, metabolic syndrome is associated with high rates of cardiovascular events.6-8) Several studies that attempted to identify the link between sodium intake and metabolic syndrome reported a high prevalence of sodium sensitivity in the study populations.9)10) However, the limitation of short-term intervention trials is that the obtained results cannot reflect daily sodium intake in non-research, real-world settings. In a population-based study from South Korea,10) a dietary survey method was used instead of the 24-hour urine method in the estimation of sodium intake. However, dietary survey methods are limited by over- or under-estimation of sodium intake.11-13)
Estimation of sodium intake by 24-hour urine collection is considered the gold standard method by the World Health Organization.14) Furthermore, few studies have estimated sodium intake in subjects with metabolic syndrome by using 24-hour urine sodium excretion. In the present study, we investigated sodium intake by measurement of 24-hour urine sodium excretion in individuals with metabolic syndrome.
The population of the present study was summed from two study populations. The first study (NCT01438619) was designed to improve the measurement method of sodium intake and to evaluate the effect of sodium intake on cardiovascular health. Subjects were recruited by the list-assisted random digit dialing (LARDD) method.15) In brief, LARDD selected a random sample of both listed and unlisted working telephone numbers. Within each of the selected households, a random selection was used to choose between adults aged 20 and 65 years. Of the 10576 telephone numbers, 1623 calls were answered. Among these, 496 participants visited the clinical trial center and provided written informed consent. An additional number of subjects (n=124) were recruited through advertisements.
The second study (NCT01237717) was designed to evaluate the relationship between sodium intake and hemodynamic variables among 200 volunteers recruited from outpatient clinics (35-65 years of age). Among the 820 participants, 531 subjects underwent complete urine collection, 24-hour ambulatory BP measurement, and all blood tests. Subjects who had taken antihypertensive medication within 6 months prior to study participation were excluded to avoid the influence of medications on urine sodium excretion. The final analysis of this study included 463 subjects (Fig. 1).
The first study began in April 2011 and the second study running from May 2010. Both studies were completed in December 2011. Both studies were performed at Dongguk University Ilsan Hospital with the same measurement protocol. The two study designs were reviewed and approved by the Institutional Review Board at Dongguk University Ilsan Hospital.
The protocol for 24-hour urine collection has been described previously.15) Briefly, the participants visited the clinical trial center before 08:30 AM and received detailed instructions about the study procedure and provided informed consent. Fasting blood glucose, total cholesterol, triglyceride, high density lipoprotein-cholesterol (HDL-C), low density lipoprotein-cholesterol (LDL-C), and serum sodium and potassium levels were measured after at least 8 hours of overnight fasting. Body weight, waist circumference, and height were also measured. BP was measured from both arms after the patients were seated for 5 minutes using a validated automatic BP device (WatchBP Office; Microlife, Widnau, Switzerland). The amount of excreted sodium and potassium was measured using a Modular DPE chemistry ion-selective electrode (Roche Diagnostics, Mannheim, Germany). Creatinine level was measured by the Jaffe reaction (Kinetic colorimetric assay; Roche Diagnostics). The validity of 24-hour urine collection was assessed by a combination of self-reported urine loss and 24-hour urine creatinine-based determination, assuming the urinary creatinine excretion rate to be constant. If a self-reported loss of a urine sample was more than 100 mL or more than once, or if a creatinine index {24-hour urine creatinine, (mg/dL)÷(21×body weight)} was <0.7, the collected urine sample was considered an inadequate 24-hour period collection.16)
In each of the patients in both studies, 24-hour ambulatory BP monitoring was performed at 30 minutes intervals, in parallel to the 24-hour urine collection, using a Mobil-O-Graph automated, non-invasive oscillometric device (I.E.M. GmbH, Stolberg, Germany). A valid measurement was defined when >80% of the total readings measured BP. Hypertension was defined as a 24-hour average systolic BP (SBP) ≥130 mm Hg or a 24-hour average diastolic BP (DBP) ≥80 mm Hg.17)
Diagnosis of metabolic syndrome was made when three abnormal findings out of the following five findings were present: triglycerides ≥150 mg/dL (≥1.7 mmol/L); HDL-C <40 mg/dL (<1.0 mmol/L) for men and <50 mg/dL (<1.3 mmol/L) for women; SBP ≥130 and/or DBP ≥85 mm Hg; fasting blood glucose ≥100 mg/dL or receiving drug treatment for elevated blood glucose levels; and waist circumference >90 cm for men and >85 cm for women.18)
All statistical analyses were performed using Statistical Package for the Social Sciences version 20 (IBM, Chicago, IL, USA). Null hypotheses of no difference were rejected if the p was <0.05. Continuous variables were expressed as mean±SD, and categorical variables were described by numbers and percentages. Continuous data were analyzed by Student's t-test for two group comparison, and proportions between groups were compared by the chi-square test. Analysis of variance test were used for evaluation of differences between mean values of groups. As a post-hoc analysis, Tukey's Honestly Significant Difference test was used. The association between tertiles of 24-hour urine sodium excretion and metabolic syndrome factors was assessed by the analysis of covariance (ANCOVA), controlling for gender, levels of body mass index (BMI), triglyceride levels, HDL-C levels, fasting blood glucose levels, the presence of diabetes mellitus, and 24-hour averaged SBP and DBP.
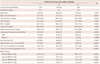
One hundred thirty one (28.3%) of the 463 subjects had metabolic syndrome (Table 1). These subjects had higher mean age, BMI, BP, fasting blood glucose, total cholesterol, LDL-C, and triglyceride levels, but lower HDL-C level, than in those without metabolic syndrome. The 24-hour urine sodium excretion was significantly higher in subjects with metabolic syndrome (p=0.0001), but only among women (p=0.0022) not men (p=0.5297). The 24-hour urine potassium excretion and urine sodium/potassium ratio was greater for subjects with metabolic syndrome (p=0.0184 and p=0.0376, respectively).
To evaluate the relationships between factors important for metabolic syndrome and cardiovascular anomalies, subjects with four or five metabolic syndrome factors were summed for analysis. The number of metabolic syndrome factors was significantly related with BMI, BP, level of total cholesterol, LDL-C, HDL-C, triglyceride, and fasting blood glucose. A significant relationship was found between 24-hour urine sodium excretion and number of metabolic syndrome factors (p<0.0001) (Fig. 2). Subjects with four or more metabolic syndrome factors had higher levels of 24-hour urine sodium excretion compared to those with none or a single factor (p<0.05 by Tukey's HSD test). Subjects with three metabolic syndrome factors also had higher levels of 24-hour urine sodium excretion compared to those with no factors (p=0.034 by Tukey's HSD test). A significant relationship between the level of 24-hour urine sodium excretion and number of metabolic syndrome factors existed among women (p=0.0308) (Fig. 2) but not men (p=0.2235) (Fig. 2). In addition, women with three metabolic syndrome factors also had higher levels of 24-hour urine sodium excretion compared to women with two factors (p=0.0199 by Tukey's HSD test).
Regarding the tertile groups of 24-hour urine sodium excretion, the proportion of subjects with metabolic syndrome and hypertension not receiving antihypertensive medication increased across the tertile groups. Likewise, significant association was found between tertile groups of 24-hour urine sodium excretion and the prevalence of metabolic syndrome among women, but not men (Table 2). Increased BMI and triglyceride levels and decreased HDL-C levels were evident across the tertile groups. ANCOVA performed after adjustment for metabolic syndrome factors indicated an independent association between BMI and the tertile groups of 24-hour urine sodium excretion (p<0.0001). Except for gender and BMI, there was no association between other factors and the tertile groups (p>0.05). Twenty four-hour SBP and average daytime SBP were significantly associated with the tertile groups, and these associations remained significant after adjustment for age, gender, LDL-C level, smoking status, and presence of diabetes mellitus (p=0.0164 and p=0.0021, respectively). However, they were not noted when BMI was entered into the multivariate analysis (p>0.05).
Most studies of sodium intake in the Korean population have been based on the dietary survey data from the Korean Health and Nutrition Examination Survey.10)19) When evaluating the relationship between sodium intake and disease, it is recommended that the data should be obtained using the 24-hour urine collection method.14) This was done in the present study. This is the first study in the Korean population to evaluate the association between metabolic syndrome and sodium intake estimation by 24-hour urine collection.
Subjects with metabolic syndrome had a higher average sodium intake than subjects without metabolic syndrome. The number of metabolic syndrome factors was significantly associated with sodium intake. An additional indicator of high sodium intake in female subjects with metabolic syndrome was the association of numbers of metabolic syndrome factors with sodium intake.
Most studies have evaluated the association of metabolic syndrome with sodium intake by dietary intervention, and have reported increased BP in association with high sodium intake.9) Individuals with metabolic syndrome demonstrated augmented BP to high sodium intake.9) High prevalence of sodium sensitivity in individuals with metabolic syndrome suggests that even small increases in sodium consumption could be an important risk factor of cardiovascular events in this population.20) In addition, evaluation of sodium intake is also important. However, only few studies have evaluated the amount of baseline sodium intake in individuals with metabolic syndrome.21) Hoffmann and Cubeddu21) reported that sodium intake was higher among individuals with metabolic syndrome than among those without metabolic syndrome. In that study population, both genders exhibited significant associations between sodium intake and presence of metabolic syndrome, with the association being stronger for men than for women. On the contrary, the association between sodium intake and metabolic syndrome was significant only among women in our study. The reason for this discrepancy is uncertain. It might reflect differences in study populations, exclusion criteria (no antihypertensive medications in our study), the method of 24-hour urine collection, and/or the statistical power. The lack of association between sodium intake and metabolic syndrome among men in this study will need to be verified in a larger population study. In the present study population, subjects with metabolic syndrome had higher levels of urine sodium/potassium ratio compared to subjects without metabolic syndrome, despite higher levels of potassium excretion. This result suggests high-risk diet patterns among subjects with metabolic syndrome.22) The collective findings from previous and the present studies provide indirect evidence that reduction of sodium consumption is an important preventive goal in reducing cardiovascular event in individuals with metabolic syndrome.
Multivariate analysis revealed a strong association between BMI and 24-hour urine sodium excretion. The mechanism linking obesity and sodium intake is currently unclear.23) One possible explanation is that increased food consumption could lead to high sodium intake. Although the concentration of sodium is low in most foods, increased consumption of food results in relative increases in intake of sodium. Indirect evidence has been reported for the association between increased food consumption and urinary sodium excretion.24) An alternate explanation is that increased consumption of sugar-sweetened soft drinks are accompanied by ingestion of foods with high sodium content.25)26)
Obesity is a well-known risk factor of BP elevation.27) One of the proposed mechanisms causing BP elevation in obesity is an increase in sodium sensitivity.28) Previous studies have reported on the association between metabolic syndrome and sodium sensitivity.9)10) Individuals with sodium sensitivity exhibits a marked elevation of BP with sodium intake, even at relatively low levels, when compared to individuals without sodium sensitivity.29) Individuals with metabolic syndrome are often obese, and this may explain why BP may easily increase in these individuals, even if their sodium intake is relatively low.
The limitation of our study is non-homogeneity of the study population. Among the 463 subjects, 307 subjects were recruited by random selection method (LARDD) to obtain a representative population of the city in which our research institution is located. The remaining 156 participants were volunteers recruited through advertisement. Although a homogenous population would be ideal, the number of women with metabolic syndrome was not adequate in the subset of participants recruited by LARDD (n=18). Among these, only six women had four or five metabolic syndrome factors. Furthermore, we have to consider large daily variations in sodium intake and urinary sodium excretion.30) Thus, a larger study size will be needed to statistically power the study, and two distinct recruitment protocols were used to this end.14)
In conclusion, sodium intake was significantly higher in women with metabolic syndrome than in women without metabolic syndrome. Along with the findings from the study by Hoffmann and Cubeddu,21) our study implicated elevated sodium consumption with metabolic syndrome. While the present study did not evaluate causality between high sodium intake and metabolic syndrome, the high prevalence of sodium sensitivity9) and high sodium intake indicate that dietary education to reduce sodium consumption should be emphasized for patients with metabolic syndrome.
Figures and Tables
Fig. 2
The 24-hour urine sodium excretion compared according to the number of metabolic syndrome factors. In all subjects, a significant relationship was found between 24-hour urine sodium excretion and number of metabolic syndrome factors (p<0.0001). There was a significant difference of 24-hour urine sodium excretion according to the number of metabolic syndrome factors in women (p=0.0308), but not in men (p=0.2235). Data are expressed as mean±standard deviation. Data from subjects with five factors of metabolic syndrome were added to four factors.

Table 1
Comparison of subjects with and without the metabolic syndrome

Data are expressed as mean±standard deviation, or number and percent in parentheses, as appropriate. *p by independent t-test or chi-square test. LDL-C: low density lipoprotein-cholesterol, HDL-C: high density lipoprotein-cholesterol, SBP: systolic blood pressure, DBP: diastolic blood pressure, MS: metabolic syndrome
Table 2
Comparison of metabolic syndrome, hypertension and blood pressures in tertiles of urinary sodium excretion
Acknowledgments
This research was supported by grants from the Korea Food and Drug Administration in 2011 (11162KFDA162) and Korean Society of Cardiology (2010-2).
References
1. Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ. 1988; 297:319–328.
2. Cook NR, Cutler JA, Obarzanek E, et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP). BMJ. 2007; 334:885–888.
3. Tuomilehto J, Jousilahti P, Rastenyte D, et al. Urinary sodium excretion and cardiovascular mortality in Finland: a prospective study. Lancet. 2001; 357:848–851.
4. MacGregor GA, Markandu ND, Sagnella GA, Singer DR, Cappuccio FP. Double-blind study of three sodium intakes and long-term effects of sodium restriction in essential hypertension. Lancet. 1989; 2:1244–1247.
5. Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001; 344:3–10.
6. Jee SH, Jo J. Linkage of epidemiologic evidence with the clinical aspects of metabolic syndrome. Korean Circ J. 2012; 42:371–378.
7. Lakka HM, Laaksonen DE, Lakka TA, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002; 288:2709–2716.
8. Kim D, Choi SY, Choi EK, et al. Distribution of coronary artery calcification in an asymptomatic Korean population: association with risk factors of cardiovascular disease and metabolic syndrome. Korean Circ J. 2008; 38:29–35.
9. Chen J, Gu D, Huang J, et al. Metabolic syndrome and salt sensitivity of blood pressure in non-diabetic people in China: a dietary intervention study. Lancet. 2009; 373:829–835.
10. Kim BK, Lim YH, Kim SG, Kim YM, Shin J. Relationship between sodium intake and blood pressure according to metabolic syndrome status in the Korean National Health and Nutrition Examination Survey. Blood Press Monit. 2012; 17:120–127.
11. Stamler J, Elliott P, Chan Q. the INTERMAP Research Group. INTERMAP appendix table, tables of contents (tables A). J Hum Hypertens. 2003; 17:665–758.
12. Yoshita K, Miura K, Okayama A, et al. A validation study on food composition tables for the international cooperative INTERMAP study in Japan. Environ Health Prev Med. 2005; 10:150–156.
13. Kwon YJ, Kim JY, Kwon KI, et al. Differences between analyzed and estimated sodium contents of food composition table or food exchange list. J Korean Soc Food Sci Nutr. 2010; 39:535–541.
14. World Health Organization. Reducing salt intake in populations: report of a WHO forum and technical meeting 5-7 October 2006, Paris, France. Geneva: World Health Organization;2007.
15. Rhee MY, Shin SJ, Park SH, Kim SW. Sodium intake of a city population in Korea estimated by 24-h urine collection method. Eur J Clin Nutr. 2013; 67:875–880.
16. Knuiman JT, Hautvast JG, van der Heyden L, et al. A multi-centre study on completeness of urine collection in 11 European centres. I. Some problems with the use of creatinine and 4-aminobenzoic acid as markers of the completeness of collection. Hum Nutr Clin Nutr. 1986; 40:229–237.
17. Rabi DM, Daskalopoulou SS, Padwal RS, et al. The 2011 Canadian Hypertension Education Program recommendations for the management of hypertension: blood pressure measurement, diagnosis, assessment of risk, and therapy. Can J Cardiol. 2011; 27:415–433. e1–e2.
18. Lim JH, Kim YK, Kim YS, Na SH, Rhee MY, Lee MM. Relationship between serum uric acid levels, metabolic syndrome, and arterial stiffness in Korean. Korean Circ J. 2010; 40:314–320.
19. Lee JS, Park J, Kim J. Dietary factors related to hypertension risk in Korean adults-data from the Korean national health and nutrition examination survey III. Nutr Res Pract. 2011; 5:60–65.
20. Weinberger MH, Fineberg NS, Fineberg SE, Weinberger M. Salt sensitivity, pulse pressure, and death in normal and hypertensive humans. Hypertension. 2001; 37(2 Pt 2):429–432.
21. Hoffmann IS, Cubeddu LX. Salt and the metabolic syndrome. Nutr Metab Cardiovasc Dis. 2009; 19:123–128.
22. Yang Q, Liu T, Kuklina EV, et al. Sodium and potassium intake and mortality among US adults: prospective data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2011; 171:1183–1191.
23. Baudrand R, Campino C, Carvajal CA, et al. High sodium intake is associated with increased glucocorticoid production, insulin resistance and metabolic syndrome. Clin Endocrinol (Oxf). 2013; [Epub ahead of print].
24. Khaw KT, Bingham S, Welch A, et al. Blood pressure and urinary sodium in men and women: the Norfolk Cohort of the European Prospective Investigation into Cancer (EPIC-Norfolk). Am J Clin Nutr. 2004; 80:1397–1403.
25. He FJ, Marrero NM, MacGregor GA. Salt intake is related to soft drink consumption in children and adolescents: a link to obesity? Hypertension. 2008; 51:629–634.
26. Karppanen H, Mervaala E. Sodium intake and hypertension. Prog Cardiovasc Dis. 2006; 49:59–75.
27. Sung JK, Kim JY. Obesity and preclinical changes of cardiac geometry and function. Korean Circ J. 2010; 40:55–61.
28. Ando K, Fujita T. Pathophysiology of salt sensitivity hypertension. Ann Med. 2012; 44:Suppl 1. S119–S126.
29. Shin SJ, Lim CY, Rhee MY, et al. Characteristics of sodium sensitivity in Korean populations. J Korean Med Sci. 2011; 26:1061–1067.
30. Liu K, Cooper R, McKeever J, et al. Assessment of the association between habitual salt intake and high blood pressure: methodological problems. Am J Epidemiol. 1979; 110:219–226.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download