Abstract
Background and Objectives
Elevated levels of myeloperoxidase (MPO) have been found in patients in different stages of coronary artery disease (CAD). The aim of this study was to assess whether the MPO liberation is increased by stress inducible myocardial ischemia and could be used to improve the diagnostic accuracy of non-invasive evaluation for myocardial ischemia.
Subjects and Methods
Seventy-six patients with suspected myocardial ischemia who underwent stress myocardial perfusion scintigraphy (MPS) were enrolled. 59 patients with an acute coronary syndrome (ACS) who received a percutaneous coronary intervention along with 12 healthy volunteers were also included in the study. In every subject the MPO plasma levels were assessed by enzyme linked immunosorbent assay. In patients undergoing MPS, the MPO levels were measured serially before and after the stress testing.
Results
Of the 76 patients undergoing MPS, 38 were diagnosed with a stress inducible myocardial ischemia. The patients with a stress induced ischemia had significantly higher basal MPO levels than those without it (32±3 ng/mL vs. 24±4 ng/mL, p=0.03). However, there was no relevant change in the MPO levels after the stress test compared to the baseline. The patients with ACS showed significantly higher MPO levels than the patients undergoing MPS (131±14 ng/mL vs. 28±2 ng/mL, p<0.01) and the healthy subjects (131±14 ng/mL vs. 26±2 ng/mL, p<0.01).
Conclusion
Since the MPO plasma levels did not increase after the stress MPS, MPO appears not to be a useful biomarker for detecting a stress inducible myocardial ischemia. Yet, the MPO levels correlate with the different stages of CAD and may hold significance as an indicator for its clinical severity.
Myeloperoxidase (MPO) is a leukocyte enzyme and a part of the innate host defence.1) By generating a highly reactive oxygen species, it contributes to the pathogenesis of atherosclerosis, e.g., by lipoprotein oxidation, matrix metalloprotease degradation and nitric oxide consumption.2) Lately, MPO has been shown to be elevated to different stages of coronary artery disease (CAD),3)4) notably in acute coronary syndrome (ACS).3)5-7) Several studies have identified the elevated MPO levels as an independent predictor of future cardiac events.8-11)
Myeloperoxidase is physiologically secreted by polymorphonuclear neutrophils (PMNs).1) PMNs have been shown to be involved in the pathogenesis of atherosclerotic plaques12-14) and in the reperfusion injury of myocardial tissue after their activation via an ischemia/reperfusion (I/R) reaction in acute ischemic syndromes.15-17)
We hypothesized that I/R reactions in a transient stress induced myocardial ischemia may result in a neutrophil activation and the subsequent secretion of MPO into the circulation. To test this assumption, we investigated whether the MPO plasma levels correlate with the severity of stress inducible myocardial ischemia using myocardial perfusion scintigraphy (MPS) in patients with suspected CAD. If so, MPO might be a useful biomarker for improving the accuracy of non-invasive myocardial ischemia diagnostics in a routine clinical setting and help detect haemodynamically relevant coronary artery stenoses. Additionally, we compared the MPO plasma levels of the patients undergoing MPS and the patients presented with ACS, who received a percutaneous coronary intervention (PCI).
A total of 147 subjects were included in this study; 76 patients with a suspected haemodynamically relevant CAD underwent a stress MPS and another 59 patients with ACS received a coronary angiography and (PCI). 12 healthy volunteers who refrained from taking any medication for at least ten days prior to the study served as a control group. The exclusion criteria were defined as cardiac revascularisation procedures within one month, a severe heart failure (New York Heart Association class III-IV), a haemodynamically relevant cardiac valvular disease, immunosuppressive disorders or medication, acute or chronic inflammatory diseases, an anti-inflammatory medication (except aspirin), severe liver or renal impairment and malignancies. The study was approved by the local ethics committee and written informed consent was obtained from each subject. The study was performed in accordance with the ethical principles outlined in the Declaration of Helsinki.
The patients underwent MPS using a one-day stress/rest protocol. An image acquisition and a tracer application were performed in accordance with the American College of Cardiology/American Heart Association/American Society for Nuclear Cardiology guidelines for the use of a cardiac radionuclide imaging.18) At first, the scintigraphic images for both stress and rest were visually evaluated based on the agreement by two experienced observers who were blinded to the findings of the MPO plasma quantification. The patients whose scans showed reversible perfusion defects were diagnosed with a stress inducible myocardial ischemia. An additional semi-quantitative analysis of the extent of the stress induced ischemia was performed computerized with the Perfit™ (Hermes Medical Solutions Inc.) software.19) The results were expressed in volume % of the left ventricular (LV) myocardium and were categorized as no relevant (<5%), mild to moderate (5-10%) and severe (>10%) myocardial ischemia.
The coronary angiographies and the PCI were followed by the guidelines of the European Society of Cardiology. Angiographies and PCI including stent implantations were performed and interpreted by at least two experienced cardiologists.
The blood samples (7.5 mL each) were drawn into tubes containing 12 mg ethylenediaminetetraacetic acid for anticoagulation. The venous blood samples were collected through a peripheral indwelling catheter immediately before and 45 to 60 minutes after the stress testing in the patients undergoing MPS. For the patients receiving PCI for ACS, blood samples were collected from a femoral sheath before the balloon angioplasty and the stent implantation. The venous blood samples from healthy volunteers were obtained randomly. All blood samples were immediately placed on ice and centrifuged at 1500 g for 15 minutes at 4℃ shortly after the collection. The plasma supernatants were stored at -80℃ until further analysis. The MPO plasma levels were assessed photometrically by a commercially available enzyme-linked immunosorbent assay. Tests were performed according to the manufacturer's instructions (Immundiagnostik AG, Bensheim, Germany). The MPO concentrations were measured in two separate aliquots of each sample. The mean values of MPO plasma concentrations are expressed in ng/mL.
For descriptive purposes, the data are expressed as means±standard error of the mean. Student's t-test was used to compare the continuous variables between the different collectives. The Mann-Whitney U test was applied when a normal distribution was not given. For comparisons within defined collectives, a paired t-tests was performed. In the absence of a normal distribution, the log rank sum test was used. Chi-square tests were applied to categorical variables. The differences were considered significant when the error probability level p was <0.05. All statistical procedures were performed using the SigmaPlot with SigmaStat integration, version 10.0 (Systat Software, Inc.).
The patients suffering from ACS were younger and more often smokers than the patients scheduled for MPS. Heart failure was also more prevalent in the ACS group. The patients with ACS were more likely to be treated with beta blockers, angiotensin converting enzyme inhibitors or angiotensin receptor blockers, statins, as well as an antiplatelet therapy with aspirin and clopidogrel, but were less likely to be on calcium channels blockers or diuretics. White blood cell count (WBC) and low density lipoprotein-cholesterol levels were higher in the ACS patients, while high density lipoprotein-cholesterol levels were higher in the MPS group. To note, C-reactive protein levels did not differ significantly between the groups (Table 1) and WBC did not differ in the subgroups of the patients with MPS, i.e., in patients with or without stress inducible ischemia and patients with no relevant or mild to moderate or severe stress induced ischemia, respectively (data not shown in detail).
The images of the 76 patients undergoing stress MPS were graded as normal in 38 subjects and revealed stress inducible myocardial ischemia in 38 subjects, respectively, by consensus of two experienced observers. Due to the computerized semi-quantitative analysis (Perfit™), 44 scans showed no relevant ischemia (<5% of LV myocardium), 16 mild to moderate (5-10%), and 16 severe (>10%) myocardial ischemia, respectively.
The basal levels of plasma MPO did not differ between the patients undergoing MPS for a suspected haemodynamically relevant CAD (n=76) and the healthy subjects (n=12) (28±2 ng/mL vs. 26±2 ng/mL, p=0.75) (Fig. 1). The patients diagnosed with a stress inducible myocardial ischemia (n=38) showed significantly higher basal plasma levels of MPO per se than those without ischemia (n=38) (32±3 ng/mL vs. 24±4 ng/mL, p=0.03) (Fig. 2). After the stress testing, however, there was no significant change in the MPO levels, neither in those with (32±3 ng/mL vs. 31±3 ng/mL, p=0.87) nor those without (24±4 ng/mL vs. 24±3 ng/mL, p=0.55) the stress induced myocardial ischemia (Fig. 2). Patients with a severe stress induced myocardial ischemia (ischemic volume >10% of LV myocardium, n=16) also had significantly higher MPO plasma levels than those with no stress inducible ischemia (ischemic volume <5% of LV myocardium, n=44), both prior to (37±5 ng/mL vs. 26±2 ng/mL, p=0.03) and after the stress testing (36±5 ng/mL vs. 25±2 ng/mL, p=0.03) (Fig. 3). Yet again, no ischemia induced changes in the MPO plasma levels were detected after MPS in all the subgroups studied (<5%: 26±2 ng/mL vs. 25±2 ng/mL, p=0.40; 5-10%: 24±4 ng/mL vs. 27±4 ng/mL, p=0.33; >10%: 37±5 ng/mL vs. 36±5 ng/mL, p=0.69) (Fig. 3). The highest MPO levels were found in the patients with ACS (n=59). MPO was excessively elevated (approximately 5-fold) when compared to the patients undergoing MPS (n=76) (131±14 ng/mL vs. 28±2 ng/mL, p<0.01) and the healthy subjects (n=12) (131±14 ng/mL vs. 26±2 ng/mL, p<0.01), respectively (Fig. 1).
The aim of our study was to evaluate the ability of MPO in predicting myocardial ischemia in a routine clinical stress testing in order to help detect hemodynamically relevant coronary artery stenosises. Therefore, two serial measurements of the MPO plasma levels were performed in the patients undergoing ischemia testing by MPS for a suspected haemodynamically relevant CAD. The present study showed no increase in the MPO levels, regardless of the extent of the stress induced myocardial ischemia.
To our best knowledge, our work is the first study to specifically test for a myocardial ischemia induced elevation of MPO levels in a longitudinal cohort of patients suspected for CAD. Wiersma et al.20) have recently demonstrated that the MPO plasma levels measured prior to MPS do not correlate with the scintigraphic myocardial perfusion abnormalities in the patients with mild anginal complaints. Of note, this trial was performed solely with type 2 diabetic patients, whereas the collective of our trial was not limited to the patients with diabetes mellitus and, most important, the MPO plasma levels were measured serially both before and after MPS in order to detect a rise in the MPO levels caused by the hypothesized liberation of MPO during a stress induced myocardial ischemia. In our view, only serial measurements before and after the stress testing allow a reliable conclusion on the possibility of an effect of a transient myocardial ischemia on the MPO levels. As stated before, we failed to detect a significant change in the MPO levels post stress induced ischemia. Therefore, MPO does not seem to be sensitive enough to enhance non-invasive myocardial ischemia testing.
Remarkably, the patients with a stress inducible myocardial ischemia have had higher MPO levels even at the baseline, i.e. prior to the stress testing. It would have been interesting to see if these patients indeed had to undergo PCI for significant stenosises more often. Unfortunately, our study cannot provide data on future coronary angiographies for these patients.
Nevertheless, we believe our results may contribute to the understanding of the circulation of MPO in the patients with CAD. MPO was thought to be secreted mainly by activated PMNs1) and an I/R reaction is a major stimulus for the PMN activation.16)17) Considering this, one possible explanation for the non-increase of the MPO levels after MPS might be that the I/R reactions during the transient stress induced myocardial ischemia are simply inadequate to activate the sufficient number of PMNs. However, existing data suggest that ischemia has no relevant effect on the measureable MPO levels.21)22) A work by Yunoki et al.22) found no relation between the elevated MPO levels and the impaired myocardial microcirculation after a reperfusion via PCI in the patients with ACS.
Moreover, the elevation of MPO levels in CAD patients is well established by now.2-4)7)10) In fact, there is a mounting evidence that a considerable amount of MPO originate directly from the atherosclerotic coronary plaque. In experimental studies, MPO was isolated from the atherosclerotic lesions in human arteries.13)23) An acute increase in the MPO levels after a coronary plaque injury from angioplasty and stent implantation has been depicted.24-26) MPO has been shown to be associated with complex lesion morphology27) and plaque erosion28) in ACS patients. In accordance, we found the highest MPO levels in the patients presented with ACS and angiographically confirmed critical CAD. In view of this, it seems likely that against the background of the pathophysiology of CAD, MPO is liberated to a considerable amount from an atherosclerotic plaque, rather than secreted by PMNs.
Based on our findings, there seems to be no increase in the MPO levels after a stress induced myocardial ischemia but the MPO levels are elevated in the patients with a stress inducible ischemia already at the baseline; these findings support the idea that the MPO levels do not correlate with myocardial ischemia but rather with the amount of coronary atherosclerotic plaques. Future investigations which directly quantify the coronary atherosclerotic burden, -e.g., by intravascular ultrasound or optical coherence tomography- and correlate this data with the MPO levels may help enhance our understanding of the role of MPO in CAD.
In conclusion, the plasma MPO levels appear to be an inadequate diagnostic tool for detecting a transient stress inducible myocardial ischemia. However, MPO seems not (only) to be secreted by PMNs but seems to stem from the coronary plaque itself. Since MPO has been shown to be elevated in more advanced stages of CAD, especially in ACS, it may prove to be of interest as an indicator for the clinical severity of CAD and the coronary plaque burden.
Figures and Tables
Fig. 1
Basal MPO plasma levels. The mean MPO plasma levels did not differ between the patients with a suspected haemodynamically relevant CAD undergoing MPS and the healthy subjects {28±2 ng/mL vs. (n=76) 26±2 ng/mL (n=12), p=0.75}. In the patients with angiographically confirmed CAD presented with ACS, the MPO levels were markedly elevated compared to the patients undergoing MPS {131±14 ng/mL (n=59) vs. 28±2 ng/mL (n=76), p<0.01} and the healthy subjects {131±14 ng/mL (n=59) vs. 26±2 ng/mL (n=12), p<0.01}, respectively. Denotes a statistic significant difference. MPO: myeloperoxidase, CAD: coronary artery disease, MPS: myocardial perfusion scintigraphy, ACS: acute coronary syndrome.

Fig. 2
MPO levels and stress induced myocardial ischemia in MPS. The MPO plasma levels were higher in the patients diagnosed with a stress inducible myocardial ischemia in MPS than in the patients without ischemia even before the stress testing was performed {32±3 ng/mL (n=38) vs. 24±4 ng/mL (n=38), p=0.03}. However, there was no significant change in the MPO plasma levels after MPS, neither in the patients without {24±4 ng/mL (n=38) vs. 24±3 ng/mL (n=38), p=0.55} nor in those with {32±3 ng/mL (n=38) vs. 31±3 ng/mL (n=38), p=0.87} a stress inducible ischemia. Denotes a statistic significant difference. MPO: myeloperoxidase, MPS: myocardial perfusion scintigraphy.
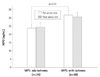
Fig. 3
MPO levels and extent of stress induced myocardial ischemia. Stress induced ischemia was analysed semi-quantitatively and expressed in volume % of the left ventricular (LV) myocardium. Three groups were defined: no relevant ischemia (ischemic volume <5% of LV myocardium), mild to moderate ischemia (5-10%), severe ischemia (>10%). The patients with a severe ischemia showed significantly higher MPO plasma levels both prior to and after the stress testing than the patients with no relevant stress inducible ischemia {37±5 ng/mL (n=16) vs. 26±2 ng/mL (n=44), p=0.03 and 36±5 ng/mL (n=16) vs. 25±2 ng/mL (n=44), p=0.03, respectively}. Again, there were no changes in the MPO levels detected after MPS, regardless of the extent of the myocardial ischemia {<5% (n=44): 26±2 ng/mL vs. 25±2 ng/mL, p=0.40; 5-10% (n=16): 24±4 ng/mL vs. 27±4 ng/mL, p=0.33; >10% (n=16): 37±5 ng/mL vs. 36±5 ng/mL, p=0.69}. Denotes a statistic significant difference. MPO: myeloperoxidase.
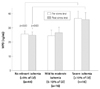
Table 1
Patient characteristics

Data are expressed as means±standard deviation. MPS denotes myocardial perfusion scintigraphy. ACS denotes acute coronary syndrome. ACE denotes angiotensinogen converting enzyme. ARB denotes angiotensin receptor blocker. MPS: myocardial perfusion scintigraphy, ACS: acute coronary syndrome, ACE: angiotensin converting enzyme, ARB: angiotensin receptor blocker, LDL-C: low density lipoprotein-cholesterol, HDL-C: high density lipoprotein-cholesterol
Acknowledgments
This work was supported by a grant from the University of Munich (Friedrich-Baur-Stiftung).
References
1. Klebanoff SJ. Myeloperoxidase: friend and foe. J Leukoc Biol. 2005; 77:598–625.
2. Brennan ML, Hazen SL. Emerging role of myeloperoxidase and oxidant stress markers in cardiovascular risk assessment. Curr Opin Lipidol. 2003; 14:353–359.
3. Ndrepepa G, Braun S, Mehilli J, von Beckerath N, Schömig A, Kastrati A. Myeloperoxidase level in patients with stable coronary artery disease and acute coronary syndromes. Eur J Clin Invest. 2008; 38:90–96.
4. Zhang R, Brennan ML, Fu X, et al. Association between myeloperoxidase levels and risk of coronary artery disease. JAMA. 2001; 286:2136–2142.
5. Eggers KM, Dellborg M, Johnston N, et al. Myeloperoxidase is not useful for the early assessment of patients with chest pain. Clin Biochem. 2010; 43:240–245.
6. Sawicki M, Sypniewska G, Kozinski M, et al. Diagnostic efficacy of myeloperoxidase for the detection of acute coronary syndromes. Eur J Clin Invest. 2011; 41:667–671.
7. Rebeiz AG, Tamim HM, Sleiman RM, et al. Plasma myeloperoxidase concentration predicts the presence and severity of coronary disease in patients with chest pain and negative troponin-T. Coron Artery Dis. 2011; 22:553–558.
8. Brennan ML, Penn MS, Van Lente F, et al. Prognostic value of myeloperoxidase in patients with chest pain. N Engl J Med. 2003; 349:1595–1604.
9. Baldus S, Heeschen C, Meinertz T, et al. Myeloperoxidase serum levels predict risk in patients with acute coronary syndromes. Circulation. 2003; 108:1440–1445.
10. Meuwese MC, Stroes ES, Hazen SL, et al. Serum myeloperoxidase levels are associated with the future risk of coronary artery disease in apparently healthy individuals: the EPIC-Norfolk Prospective Population Study. J Am Coll Cardiol. 2007; 50:159–165.
11. Mocatta TJ, Pilbrow AP, Cameron VA, et al. Plasma concentrations of myeloperoxidase predict mortality after myocardial infarction. J Am Coll Cardiol. 2007; 49:1993–2000.
12. Sugiyama S, Kugiyama K, Aikawa M, Nakamura S, Ogawa H, Libby P. Hypochlorous acid, a macrophage product, induces endothelial apoptosis and tissue factor expression: involvement of myeloperoxidasemediated oxidant in plaque erosion and thrombogenesis. Arterioscler Thromb Vasc Biol. 2004; 24:1309–1314.
13. Daugherty A, Dunn JL, Rateri DL, Heinecke JW. Myeloperoxidase, a catalyst for lipoprotein oxidation, is expressed in human atherosclerotic lesions. J Clin Invest. 1994; 94:437–444.
14. Buffon A, Biasucci LM, Liuzzo G, D'Onofrio G, Crea F, Maseri A. Widespread coronary inflammation in unstable angina. N Engl J Med. 2002; 347:5–12.
15. Naruko T, Ueda M, Haze K, et al. Neutrophil infiltration of culprit lesions in acute coronary syndromes. Circulation. 2002; 106:2894–2900.
16. Jordan JE, Zhao ZQ, Vinten-Johansen J. The role of neutrophils in myocardial ischemia-reperfusion injury. Cardiovasc Res. 1999; 43:860–878.
17. Hansen PR. Role of neutrophils in myocardial ischemia and reperfusion. Circulation. 1995; 91:1872–1885.
18. Klocke FJ, Baird MG, Lorell BH, et al. ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASNC Committee to Revise the 1995 Guidelines for the Clinical Use of Cardiac Radionuclide Imaging). J Am Coll Cardiol. 2003; 42:1318–1333.
19. Slomka PJ, Hurwitz GA, Stephenson J, Cradduck T. Automated alignment and sizing of myocardial stress and rest scans to three-dimensional normal templates using an image registration algorithm. J Nucl Med. 1995; 36:1115–1122.
20. Wiersma JJ, Verberne HJ, Meuwese MC, et al. Myeloperoxidase is not associated with scintigraphic myocardial perfusion abnormalities in type 2 diabetic patients with mild stable anginal complaints. Clin Chim Acta. 2011; 412:86–90.
21. Biasucci LM, D'Onofrio G, Liuzzo G, et al. Intracellular neutrophil myeloperoxidase is reduced in unstable angina and acute myocardial infarction, but its reduction is not related to ischemia. J Am Coll Cardiol. 1996; 27:611–616.
22. Yunoki K, Naruko T, Komatsu R, et al. Relation of elevated levels of plasma myeloperoxidase to impaired myocardial microcirculation after reperfusion in patients with acute myocardial infarction. Am J Cardiol. 2010; 105:922–929.
23. Sugiyama S, Okada Y, Sukhova GK, Virmani R, Heinecke JW, Libby P. Macrophage myeloperoxidase regulation by granulocyte macrophage colony-stimulating factor in human atherosclerosis and implications in acute coronary syndromes. Am J Pathol. 2001; 158:879–891.
24. Aminian A, Boudjeltia KZ, Babar S, et al. Coronary stenting is associated with an acute increase in plasma myeloperoxidase in stable angina patients but not in patients with acute myocardial infarction. Eur J Intern Med. 2009; 20:527–532.
25. Marshall CJ, Nallaratnam M, Mocatta T, et al. Factors influencing local and systemic levels of plasma myeloperoxidase in ST-segment elevation acute myocardial infarction. Am J Cardiol. 2010; 106:316–322.
26. Rudolph V, Steven D, Gehling UM, et al. Coronary plaque injury triggers neutrophil activation in patients with coronary artery disease. Free Radic Biol Med. 2007; 42:460–465.
27. Naruko T, Furukawa A, Yunoki K, et al. Increased expression and plasma levels of myeloperoxidase are closely related to the presence of angiographically-detected complex lesion morphology in unstable angina. Heart. 2010; 96:1716–1722.
28. Ferrante G, Nakano M, Prati F, et al. High levels of systemic myeloperoxidase are associated with coronary plaque erosion in patients with acute coronary syndromes: a clinicopathological study. Circulation. 2010; 122:2505–2513.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download