Abstract
Background and Objectives
Prolonging of the corrected QT interval (QTc) has been reported after cardiac surgery in some studies. However, there have not been many studies on infant open cardiac surgery for ventricular septal defect (VSD) repair. This study was performed to define the changes in QTc and to find related post-surgery factors in this patient group.
Subjects and Methods
From 2008 to 2012, 154 infants underwent VSD repair at the Severance Cardiovascular Hospital. This study includes 105 of these cases. QTc was measured in these patients retrospectively. Demographic data and peri-procedural data, such as Aristotle score, cross-clamp time and bypass time, were analyzed. The exclusion criteria included multiple and small VSDs that underwent direct closure.
Results
Mean post-operative QTc was increased compared to the pre-operative measurements (from 413.6±2.3 to 444.9±2.5, p<0.001). In multiple linear regression, the comprehensive Aristotle score was associated with increasing QTc (p=0.047). The incidence of transient arrhythmia, such as atrial tachycardia, junctional ectopic tachycardia, premature atrial contraction, or premature ventricular contraction, was associated with QTc prolongation (p=0.005). Prolonged QTc was also associated with cross-clamp time (p=0.008) and low weight (p=0.042). Total length of stay at the intensive care unit and intubation time after surgery were not associated with QTc prolongation.
Conclusion
Prolonged QTc could be seen after VSD repair in infants. This phenomenon was associated with peri-procedural factors such as the Aristotle score and cross-clamp time. Patients with QTc prolongation after cardiac surgery had an increased tendency towards arrhythmogenicity in the post-operative period.
Cardiopulmonary bypass with subsequent chemical changes is caused by electrophysiological changes in the ventricle.1-3) Correction of congenital heart disease, due to hemodynamic changes, can cause changes in the electrocardiogram (ECG).4-7) ECG changes after the correction of congenital heart disease, especially changes in the corrected QT interval (QTc) have not been sufficiently studied,7) especially in patients who underwent ventricular septal defect (VSD) surgery at less than one year of age. This study was performed to examine the progress of patients with increased QTc after VSD patch repair and to identify associated factors.
The study time period was a total of five years, from January 2008 to December 2012. During this period, a total of 154 patients less than one year of age underwent VSD patch repair at the Severance cardiovascular hospital. Among them, 105 patients who did not have any missing data were analyzed retrospectively. Pre- and post-operative and one-month follow-up ECGs were analyzed. Patient demographics {height, weight, and body surface area (BSA)} were investigated. The electrolyte data (Na, K, Ca, Mg) were obtained post-operation. Through the patients' records, the Aristotle score (basic and comprehensive), cross-clamp time, and bypass time were investigated. The basic Aristotle score is a procedure-adjusted complexity and only applies to procedures. The comprehensive Aristotle score includes patient-adjusted complexity. It includes two categories of complexity factors: 1) procedure-dependent factors that adjust each patient's procedure to a specific complexity (anatomical factors, associated procedures, age); and 2) procedure-independent factors that adjust for each patient's clinical status and specific complexity (general factors, clinical factors, extra-cardiac factors, surgical factors). Each factor is scored for contribution to mortality, morbidity, and difficulty. During the post-operative course, intubation time, intensive care unit (ICU) stay, and incidence of arrhythmia were investigated.
Pre-operative 12-lead ECG was performed in all patients, and the ECG performed closest to the surgery was taken as the pre-operative ECG. The post-operative ECG was performed within 24 hours after surgery. The one-month follow-up ECG was performed in the outpatient clinic. In the ECG analysis, the RR duration, QTc duration, PR interval, QRS duration, and QTc change were investigated.
The standard 12-lead ECG was performed. The beginning of the QRS and the end of the T wave had to be clearly visible in more than three leads, including lead II. The QRS duration and QTc interval were measured from the individual lead at three different points and were averaged. The QTc was defined as the beginning of the QRS to the end of the T wave. The QTc was measured in all leads and corrected by heart rate using Bazett's formula.
The collected pre- and post-operative ECG data, clinical characteristics, and possible related factors were compared. The pre- and post-operative QTc values and the one-month follow-up ECG data were compared via repeated-measure analysis of variance. The other factors that may have affected the ECG change were analyzed via multiple linear regression. The data were analyzed using Statistical Package for the Social Sciences 20.0 for Windows software (IBM, Chicago, IL, USA).
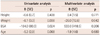
The mean height of the patients was 50.8±7.8 cm; the mean weight: 5.1±1.0 kg; the mean BSA: 0.27±0.1 m2; and the mean age: 0.20±0.12 years. The sex ratio (male : female) of the patients was 49 : 56. The patients' VSD types were: subaortic (18 patients), perimembranous (83 patients), and muscular (4 patients) (Table 1).
The patients with lower weights showed statistically significant QTc prolongation (p=0.008 in the univariate analysis; p=0.042 in the multivariate analysis). The patients with lower BSA also showed a tendency towards prolonged QTc intervals (p=0.024 in the univariate analysis; p=0.206 in the multivariate analysis). The QTc changes due to the heights and ages of the patients were not statistically significant (Table 2).
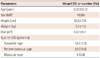
The average pre-operative QTc was 413.6±2.3 milliseconds (ms), and the average post-operative QTc was 444.9±3.5 ms; 31.3±5.8 ms longer than the average pre-operative QTc (p<0.001). Five patients with novel QTc prolongation greater than 500 ms were noted in the immediate post-operative ECG (Fig. 1). In the ECG performed one month after the surgery, the average QTc was 433.0±3.6 ms, which showed a reduction (-11.9±7.1 ms) compared to the immediate post-operative ECG (p=0.007). In the one-month follow-up ECG, however, the average QTc increased compared to the pre-operative value (p<0.001). In the ECG performed one year after the surgery, the average QTc was 436.4±30.2 ms, which did not show any significant change compared to the average QTc one month after surgery (Fig. 2).
The Aristotle score is a scoring system that predicts the relevance of the difficulty of surgery and of the post-operative mortality and morbidity. In this study, the patients with a higher basic score had a tendency of prolonged QTc (p=0.061 in the univariate analysis; p=0.809 in the multivariate analysis). As for the comprehensive Aristotle score, which includes not only the diagnosis and the surgical technique, but also other factors that may be involved in the outcome of the surgery, the increased score pointed to a statistically significant increase in the QTc prolongation (p<0.01 in the univariate analysis; p=0.047 in the multivariate analysis).
Transient arrhythmia, such as atrial tachycardia, junctional ectopic tachycardia (JET), premature atrial contraction (PAC), or premature ventricular contraction (PVC), occurred in 12 patients. There was a statistically significant correlation between the change in QTc pre- and post-operatively in these 12 patients (p<0.001 in the univariate analysis; p=0.005 in the multivariate analysis).
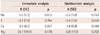
The cross-clamp time and bypass time, which are associated with myocardial ischemia time during surgery, were investigated. Increased cross-clamp time showed a statistically significant correlation with QTc prolongation (p<0.001 in the univariate analysis; p=0.008 in the multivariate analysis). The increased bypass time showed a tendency towards QTc prolongation, but the tendency was not statistically significant (p<0.001 in the univariate analysis; p=0.785 in the multivariate analysis). Intubation time and ICU stay did not show statistically significant correlations with QTc prolongation (Table 3).
There have been many studies on the relationship between ST-segment change and myocardial ischemia,8-10) but research on QTc prolongation, which is associated with depolarization and damage to the heart muscles, have not been studied intensively.6)7)
A unique aspect of our study is the homogeneity of the patient population in terms of the patients' ages, diseases and surgeries, as well as the fact that this study analyzed the QTc changes after surgery and studied their relationship to other factors.
The patients, all less than one year of age, who underwent surgery for VSD had post-operative QTc prolongation. This study was conducted to identify the factors influencing QTc prolongation.
There have been reports that cross-clamp time and bypass time may prolong the QTc interval after surgery. Prolonged cross-clamp time may cause transient myocardial ischemia, which may affect the depolarization of the heart.7)11)
Some studies show that early transmural ischemia results in QTc prolongation.6)12-14) In this study, prolonging of cross-clamp time showed a definite correlation to QTc prolongation, and prolonged bypass time also showed a tendency towards QTc prolongation.
In general, QTc prolongation is known to increase the risk of arrhythmia-related mortality and sudden cardiac death, and it also increases the risk of ventricular arrhythmias.5)7)15)16)
In this study, ventricular arrhythmia was not detected, but the relatively small patient population was not sufficient for establishing the validity of the result. Thus, further research using a large population is needed to determine the relationship between post-operative QTc prolongation and ventricular tachycardia.
In this study, transient arrhythmia occurred in 12 patients (11.4%) after surgery, and atrial tachycardia, JET, frequent PAC, and frequent PVC occurred in 4, 1, 5, and 2 patients, respectively. These patients showed QTc prolongation immediately after the surgery, but in the one-month follow-up ECG, they returned to their pre-operative state, which indicates that the change is reversible.
One month after the surgery, it was found that the QTc interval had not returned to its pre-operative level because one month is not sufficient for full recovery from the post-operative situation. Even in the one-year follow-up, it was found that the QTc interval had not returned to its pre-operative state. It was estimated that the changes in the QTc interval were due to the changes in the heart rate as the infants grew.
Change in the QTc is known to be affected by many factors. Anesthetic and antiarrhythmic drugs inhibit potassium channels in myocytes, resulting in a prolonged QTc interval.17) There is a high incidence of ventricular arrhythmia from QTc prolongation caused by drug administration.18)19)
In this study, however, no change in QTc was detected after the administration of an anesthetic drug.
In the demographic data, weight and BSA were associated with the change in QTc interval, but age and height were less relevant to the change. In the case of age, a relatively homogeneous group of patients less than one year of age was evaluated in the study. Patients' height was also not reflective of heart failure. Thus, age and height did not show a significant correlation with the QTc interval changes.
Electrolyte levels, intubation time and length of ICU stay also did not show (Table 4) a statistically significant correlation in QTc prolongation as these factors were considered in the development of operation and the development of ICU care.
There are reports that show a correlation between the Aristotle score and the occurrence of arrhythmia after surgery.6)20) In this study, the Aristotle score, based on the scoring system that predicts the mortality and morbidity after surgery, showed a positive correlation with QTc prolongation.
The comprehensive Aristotle score was more statistically significant than the basic Aristotle score. The comprehensive Aristotle score reflects the patient's characteristics (weight less than 2.5 kg, preterm birth), pre-operative clinical factors (heart, lungs, infections, GIT, blood, kidneys, nervous, endocrine anomalies), extracardiac factors (such as genetic and chromosomal), and other surgical procedures (including minimally invasive procedures).
This study has a number of limitations. First, it was conducted retrospectively and ECGs were obtained based on clinical indications, rather than by a study design. Second, the QTc interval may vary depending on different factors, such as the heart rate, autonomic nervous system, body temperature, electrolyte concentration, and drugs given. This phenomenon is due to the change in the myocardial refractory period in accordance with the change in the heart rate. QTc intervals, however, are also affected by several other factors. When the QTc changes due to a change in the heart rate, it occurs over a relatively long period of time, changing slowly over several minutes, which indicates that correcting the QTc by simply looking at the heart rate may be inaccurate.21) In this study, Bazett's formula was used, which reflects only the changes in the heart rate and does not accurately reflect the condition of the patient at the time when the ECG was performed.
In conclusion, QTc prolongation was seen after VSD repair in infants. This phenomenon was associated with peri-procedural factors such as the Aristotle score and cross-clamp time. The patients with prolonged QTc after cardiac surgery in this study showed an increased tendency towards arrhythmogenicity in the post-operative period.
Figures and Tables
Fig. 1
Post-operation electrocardiogram and QTc prolongation (QTc 516 ms). HR 149, RR interval 472 ms, PR interval 98, QRS duration 58 ms, QT interval 326 ms.
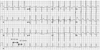
Fig. 2
Change in QTc over time. The average pre-operative QTc was 413.6±2.3 milliseconds (ms). The average post-operative QTc was 444.9±3.5 ms, 31.3±5.8 ms longer than the average pre-operative QTc (p<0.001). In the ECG performed one month after the surgery, the average QTc was 433.0±3.6 ms, which showed a reduction (-11.9±7.1 ms) compared to the immediate post-operative ECG (p=0.007). In the ECG performed one year after surgery, however, the average QTc was 436.4±30.2 ms, which did not show a significant change compared to the average QTc one month after the surgery (p=0.273). n=105. ECG: electrocardiogram.

Acknowledgments
The authors wish to thank SJ Park, Division of Pediatric Cardiology of Sejong General Hospital for language consultation.
References
1. Kim YH, Choi HJ, Kim GJ, Cho JY, Hyun MC, Lee SB. The changes in signal-averaged electrocardiogram after surgical correction of congenital heart disease. Korean J Pediatr. 2009; 52:1364–1369.
2. Creswell LL, Schuessler RB, Rosenbloom M, Cox JL. Hazards of postoperative atrial arrhythmias. Ann Thorac Surg. 1993; 56:539–549.
3. Ascione R, Lloyd CT, Underwood MJ, Lotto AA, Pitsis AA, Angelini GD. Inflammatory response after coronary revascularization with or without cardiopulmonary bypass. Ann Thorac Surg. 2000; 69:1198–1204.
4. Vetter VL, Horowitz LN. Electrophysiologic residua and sequelae of surgery for congenital heart defects. Am J Cardiol. 1982; 50:588–604.
5. Delaney JW, Moltedo JM, Dziura JD, Kopf GS, Snyder CS. Early postoperative arrhythmias after pediatric cardiac surgery. J Thorac Cardiovasc Surg. 2006; 131:1296–1300.
6. Rekawek J, Kansy A, Miszczak-Knecht M, et al. Risk factors for cardiac arrhythmias in children with congenital heart disease after surgical intervention in the early postoperative period. J Thorac Cardiovasc Surg. 2007; 133:900–904.
7. Punn R, Lamberti JJ, Balise RR, Seslar SP. QTc prolongation in children following congenital cardiac disease surgery. Cardiol Young. 2011; 21:400–410.
8. MacLeod RS, Shome S, Stinstra J, Punske BB, Hopenfeld B. Mechanisms of ischemia-induced ST-segment changes. J Electrocardiol. 2005; 38:4 Suppl. 8–13.
9. Bae MH, Cheon SS, Song JH, et al. Etiologies and predictors of ST-segment elevation myocardial infarction. Korean Circ J. 2013; 43:370–376.
10. Jain U, Wallis DE, Moran JF. Significance of electrocardiographic ST elevation during coronary artery bypass surgery. Anesth Analg. 1994; 78:638–643.
11. Ali N, Rizwi F, Iqbal A, Rashid A. Induced remote ischemic pre-conditioning on ischemia-reperfusion injury in patients undergoing coronary artery bypass. J Coll Physicians Surg Pak. 2010; 20:427–431.
12. Kenigsberg DN, Khanal S, Kowalski M, Krishnan SC. Prolongation of the QTc interval is seen uniformly during early transmural ischemia. J Am Coll Cardiol. 2007; 49:1299–1305.
13. Vrtovec B, Ryazdanbakhsh AP, Pintar T, Collard CD, Gregoric ID, Radovancevic B. QTc interval prolongation predicts postoperative mortality in heart failure patients undergoing surgical revascularization. Tex Heart Inst J. 2006; 33:3–8.
14. Aburawi EH, Souid AK, Liuba P, Zoubeidi T, Pesonen E. Early changes in myocardial repolarization and coronary perfusion after cardiopulmonary bypass surgery for ASD repair in children. BMC Cardiovasc Disord. 2013; 13:67.
15. Elming H, Brendorp B, Køber L, Sahebzadah N, Torp-Petersen C. QTc interval in the assessment of cardiac risk. Card Electrophysiol Rev. 2002; 6:289–294.
16. Trinkley KE, Lee Page R 2nd, Lien H, Yamanouye K, Tisdale JE. QT interval prolongation and the risk of torsades de pointes: essentials for clinicians. Curr Med Res Opin. 2013; [Epub ahead of print].
17. Nagele P, Pal S, Brown F, Blood J, Miller JP, Johnston J. Postoperative QT interval prolongation in patients undergoing noncardiac surgery under general anesthesia. Anesthesiology. 2012; 117:321–328.
18. Roden DM. Drug-induced prolongation of the QT interval. N Engl J Med. 2004; 350:1013–1022.
19. Reingardiene D, Vilcinskaite J. [QTc-prolonging drugs and the risk of sudden death]. Medicina (Kaunas). 2007; 43:347–353.
20. Manrique AM, Arroyo M, Lin Y, et al. Magnesium supplementation during cardiopulmonary bypass to prevent junctional ectopic tachycardia after pediatric cardiac surgery: a randomized controlled study. J Thorac Cardiovasc Surg. 2010; 139:162–169.
21. Davey P. How to correct the QT interval for the effects of heart rate in clinical studies. J Pharmacol Toxicol Methods. 2002; 48:3–9.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download