Abstract
Background and Objectives
The aim of this study was to investigate the balloon occlusive diameter (BOD) of non-circular defects in the transcatheter closure of atrial septal defect (ASD).
Subjects and Methods
A total of 67 patients who had undergone transcatheter closure of an ASD were reviewed retrospectively. A non-circular defect was defined as the ratio of the short diameter to the long diameter of the defect on the en-face image less than 0.75. The BOD was compared with the long diameter of the defect and then compared between the two groups.
Results
There were 22 patients with circular defects and 45 patients with non-circular defects. The difference in BOD measuring from the long diameter of the defect was quite different between the two groups and significantly smaller in non-circular morphology (0.1±4.0 vs. 2.3±2.1, p=0.006). The difference in BOD measurement from the long diameter of ASD showed a positive correlation with the ratio of the short diameter to the long diameter of ASD (b/a) (r2=0.102, p=0.008). In the non-circular morphology of ASD, the difference in BOD measured from the long diameter had a significant negative correlation with the long diameter of ASD (r2=0.230, p=0.001), whereas in circular ASD, no significant correlation was found between the difference in BOD and the long diameter of ASD (p=0.201).
Transcatheter closure of the atrial septal defect (ASD) using an Amplatzer septal occlude (ASO) (AGA medical, Golden Valley, MN, USA) has become a competitive alternative to surgery in selected patients and has demonstrated very good clinical outcomes.1-3) Nowadays, successful device closure is reported even in small children.4) For successful device closure of the ASD, a detailed anatomical evaluation of the size, morphology, and spatial relationship with the surrounding structures is crucial. In general, ASD provides various shapes, including circular, ovoid, and complex morphology.5-7) Therefore, there have been various studies addressing the usefulness of real-time three-dimensional (3D) transesophageal echocardiography (TEE) in evaluating the morphology of ASD and in the guidance of device closure.5)6)8-10) En-face images from 3D TEE are helpful to evaluate the morphology of ASD.11-13)
The balloon occlusive diameter (BOD) in ASD is a standard method to determine device size.2)14) It is well known that balloons can overestimate the ASD size in some patients. Therefore, we used BOD with caution in balloon sizing. However, the BOD can be affected by the morphology of ASD, and this has not been well evaluated. Therefore, the aim of this study was to compare the BOD of non-circular ASD with that of circular ASD.
This was a retrospective study of patients who had undergone a percutaneous closure of ASD with ASO (AGA Medical, Golden Valley, MN, USA) at the Samsung Medical Center from January 2010 to September 2012. ASD was diagnosed by transthoracic echocardiography. Thereafter, TEE was performed for the further evaluation of ASD. The criteria for the transcatheter closure of ASD with ASO were 2' ASD, with the evidence of right ventricular volume overload. However, the degree of pulmonary arterial hypertension was not too significant so as not to be irreversible and 2' ASD with appropriate surrounding rims were used for the device.
The morphology of ASD and intact size were evaluated with TEE. The long diameter (a) and short diameter (b) were measured at the end-systolic phase from reconstructed en-face images on 3D TEE (Fig. 1). The ratio of the short diameter to the long diameter (b/a) was calculated, and non-circular morphology was defined as b/a < 0.75,5) whereas circular morphology was defined as b/a ≥0.75. The device size was the waist diameter of ASO.
Transesophageal echocardiography studies were recorded with a commercially available ultrasound system (Philips iE33; Philips Medical Systems, Andover, MA, USA) using a matrix-array 3D TEE probe (X7-2t; Philips Medical Systems). Patients were sedated with intravenous midazolam during image recording. First, routine two-dimensional (2D) TEE was performed with a color Doppler image. Biplane imaging (a side-by-side display of a pair of 2D TEE images that are 90 apart) was then obtained to measure the diameter of ASD. Next, full-volume imaging was acquired with 4 beat captures. Measurement was performed off-line using QLAB Cardiac Analysis (Philips Medical Systems). On multiplanar reconstruction images, longitudinal planes of the long and short diameters were identified using guidance on the en-face of the defect from the right atrial side.
Balloon sizing for deciding device size was applied under the guidance of intracardiac echocardiography during the procedure. Balloon inflation was ceased just at the moment when the shunt flow disappeared or at the moment when most of the shunt disappeared, despite a minimal visible shunt. Making a waist in sizing balloon on angiography was avoided due to it being regarded as oversizing. The same size device or a 1-2 mm larger size device was chosen. If successful implantation failed or oversizing was suggested, we changed the device to another size. Residual shunt and complications were checked via a follow-up trans-thoracic echocardiogram the next day and again 3 months later. All patients were recommended to take 100 mg/day of aspirin for 6 month after implantation.
Data are expressed as mean±standard deviation. To compare the results of two groups, the parametric Student t-test and chi-square test in Statistical Package for the Social Sciences (SPSS)19.0 (SPSS Inc., Chicago, IL, USA) were used. Linear regression analysis was applied to prove the linear correlation of BOD and defect morphology. A p<0.05 was considered to be statistically significant.
We stated that the locally appointed ethics committee approved the research protocol, and informed consent was waived.
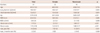
All the data are described in Table 1. A total of 45 patients had non-circular ASD and 22 patients had circular ASD. They consisted of 18 male and 49 female patients. The range of patient ages was from 15.0 to 74.0 years old. The mean long diameter (a) and short diameter (b) were 19.6 (8.1-36.1) mm and 13.6 (5.7-24.4) mm, respectively. The ratio of the short diameter to the long diameter (b/a) was 0.70±0.10 (0.50-0.90). The median size of ASO was 20 mm (8-34 mm). The BOD was 20.4±5.0 (8.5-37.0) mm, and the difference of BOD from the long diameter was from 10.6 to 7.7 mm. The difference of the device size from the long diameter of ASD was 1.7±3.5 mm, whereas the ratio of the device size to the long diameter was 1.11±1.18. Echocardiography performed the next day and 3 months after the procedure revealed a small leak in 19 (28.4%) patients and 2 (3.0%) patients, respectively.
In patients with ASD of non-circular morphology, the long diameter was significantly longer than that of circular ASD, but those of the short diameter and BOD did not differ. The difference of BOD from the long diameter of ASD was quite different between the two groups and significantly smaller in non-circular morphology (0.1±4.0 vs. 2.3±2.1, p=0.006). As a result, the difference of device size from the long diameter of ASD and the ratio of the device size to the long diameter were significantly smaller in non-circular ASD (p<0.01). The difference of BOD from the long diameter of ASD showed a positive correlation with the ratio of the short diameter to the long diameter of ASD (b/a) (r2=0.102, p=0.008) (Fig. 2A). Regarding the non-circular morphology of ASD, the difference of BOD from the long diameter had a significant negative correlation with the long diameter of ASD (r2=0.230, p=0.001) (Fig. 2C), whereas in circular ASD, no significant correlation between the differences in BOD and long diameters of ASD was observed (p=0.201) (Fig. 2B).
The residual leakage rates immediately (12/45 vs. 7/22) and 6 months later (2/45 vs. 0/22) did not differ between the groups (p>0.05). However, both two patients with residual leakage 6 months later had non-circular morphology. No embolization was found in our series.
In our study, the sizes of ASDs varied widely, and non-circular defects were predominant. When we defined non-circular ASD as the short diameter that is <75% of the long diameter measured from the en-face image on 3D TEE, non-circular ASD comprised 67.2% of our total patients. Jhori et al.5) reported 42% oval and 33% complex shapes of ASD in 25 total ASDs using real-time 3D echocardiogram. Therefore, obtaining an accurate dimension in relation to the shape of the defect is considered to be important for successful transcatheter closure, because the ASO is uniform. In general, multiplane 2D TEE can assess the size, anatomy, and suitability of the lesion for closure. 2D TEE can mentally integrate multiple image planes for the operator to reconstruct the 3D anatomy of ASD, but has limitations of visualizing the accurate shape of the defect. However, 2D TEE cannot accurately define non-circular shaped ASD and can underestimate the area of complex shaped ASD, which can result in a residual shunt or embolization.5) There were some studies5)6)12)15) describing the complex shapes of ASD using 3D TEE. However, TEE can cause patient discomfort and has the potential to damage the esophagus. Cardiac CT can be considered as an alternative because Ko et al.16) reported that cardiac CT is very helpful in the noninvasive evaluation of the ASO implantation of ASD. However, the general concern about cardiac CT is exposure to harmful radiation. En-face imaging and measuring the defect area using 3D TEE can be obtained easily using commercially available software programs. The maximal diameter of the defect should be measured at the end-systolic phase. Regarding the device size, balloon sizing has been considered an integral part of the transcatheter closure of ASD with ASO. In special cases of non-circular ASD, the effect of balloon inflation would alter the shape of the defect to conform to the relatively circular shape of the balloon. Moreover, based on Zanchetta's study,17) the device size in the non-circular ASD may be smaller than the long diameter: c=√(a×b). The effect of balloon inflation on the non-circular defect would be to decrease the maximal diameter and increase the minimal diameter, while preserving the overall area. We observed that the difference between the BOD and the long diameter of the non-circular defect was smaller than that of the circular defect. The more severe the non-circularity (lower b/a), the smaller the difference of BOD from the long diameter (r2=0.102, p=0.008). Therefore, it was clear that the device size implanted in the non-circular defect was smaller than that in the circular defect when compared to the long diameter. Balloon sizing in our procedure was conducted very carefully to prevent oversizing. In this period, it is recommended that oversizing be avoided due to the risks of mushrooming deformity and the impingement of cardiovascular structures along with other serious complications.18)19) This is the reason why the BOD is preferred to the stretched balloon diameter. Sadeghian et al.20) reported that the BOD was larger than the ASD size measured by TEE, but the difference between BOD and TEE values became smaller when TEE sizing was larger. Seo et al.13) reported that the size difference between the stretched balloon diameter and ASD maximal diameter measured by TEE was smaller in oval shaped large ASD than round shaped ASD. We also found similar findings in our study.
ASD had a longer diameter and non-circular morphology by 3D TEE had a smaller difference of BOD from the long diameter of ASD than the others. This suggests that oversized devices can be implanted in non-circular ASD closure with ASO, if the morphology of ASD is not considered.
Our data showed successful ASO implantation in non-circular ASD closure, as well as in circular ASD. Residual leakage 6 months after the procedure did not differ between the groups. Moreover, no significant residual shunt was observed in our patients. In another study,1) a residual shunt one day after device closure was found in 8.6% of subjects, and a residual shunt three months after closure was found only in 1.3% of patients. There were no differences in the occurrence of complications.
The main limitations of our study are the small number of patients and that it was not a randomized control study. This retrospective analysis was based on patients who had undergone transcatheter closure of ASD, with ASO performed by fully experienced operators. En-face images from 3D TEE require experience and expertise. The device size, chosen by these operators, was not based on a constant equation, but on personal experience. Although it was not rare, we did not address when 3D reconstruction was inadequate in cases of complex atrial septum. It may have been better if we were able to suggest other ways, such as cardiac CT, when 3D images from TEE were not adequate. The last thing was that we could not define an exact rule for was in choosing the adequate device size from balloon sizing methods. However, we were able to experience that the transcatheter closure of ASD with ASO was safe and effective, even for non-circular ASD.
In conclusion, BOD compared with the long diameter measured from 3D TEE was smaller in non-circular ASD than in circular ASD. The difference was much smaller in non-circular ASD with a large long diameter. Therefore, we can suggest that a pre-procedural 3D TEE image for non-circular ASD can help expect relatively smaller BOD and smaller devices than those for circular ASD.
Figures and Tables
Fig. 1
The reconstructed en-face image from three-dimensional transesophageal echocardiography shows a circular defect (A) and a non-circular defect (B). a: the long diameter, b: the short diameter.

Fig. 2
The difference of the balloon occlusive diameter from the long diameter of the atrial septal defect (ASD) had a significant positive correlation with the ratio of the short diameter to the long diameter (A). The difference of balloon occlusive diameter from the defect size did not have a significant correlation with the long diameter in ASD with circular morphology (p=0.201) (B), whereas the difference in balloon occlusive diameter had a significant negative correlation with the long diameter in ASD with non-circular morphology (p=0.001) (C). BOD: balloon occlusive diameter.

References
1. Masura J, Gavora P, Podnar T. Long-term outcome of transcatheter secundum-type atrial septal defect closure using Amplatzer septal occluders. J Am Coll Cardiol. 2005; 45:505–507.
2. Majunke N, Bialkowski J, Wilson N, et al. Closure of atrial septal defect with the Amplatzer septal occluder in adults. Am J Cardiol. 2009; 103:550–554.
3. Yew G, Wilson NJ. Transcatheter atrial septal defect closure with the Amplatzer septal occluder: five-year follow-up. Catheter Cardiovasc Interv. 2005; 64:193–196.
4. Kim NK, Park SJ, Choi JY. Transcatheter closure of atrial septal defect: does age matter? Korean Circ J. 2011; 41:633–638.
5. Johri AM, Witzke C, Solis J, et al. Real-time three-dimensional transesophageal echocardiography in patients with secundum atrial septal defects: outcomes following transcatheter closure. J Am Soc Echocardiogr. 2011; 24:431–437.
6. Roberson DA, Cui W, Patel D, et al. Three-dimensional transesophageal echocardiography of atrial septal defect: a qualitative and quantitative anatomic study. J Am Soc Echocardiogr. 2011; 24:600–610.
7. Ferreira SM, Ho SY, Anderson RH. Morphological study of defects of the atrial septum within the oval fossa: implications for transcatheter closure of left-to-right shunt. Br Heart J. 1992; 67:316–320.
8. van den Bosch AE, Ten Harkel DJ, McGhie JS, et al. Characterization of atrial septal defect assessed by real-time 3-dimensional echocardiography. J Am Soc Echocardiogr. 2006; 19:815–821.
9. Bhaya M, Mutluer FO, Mahan E, et al. Live/Real time three-dimensional transesophageal echocardiography in percutaneous closure of atrial septal defects. Echocardiography. 2013; 30:345–353.
10. Nasis A, Harper RW, Mottram PM. Real-time three-dimensional transoesophageal echocardiography for guidance of transcatheter closure of a complex multifenestrated atrial septal defect. Heart Lung Circ. 2011; 20:343–344.
11. Marx GR, Fulton DR, Pandian NG, et al. Delineation of site, relative size and dynamic geometry of atrial septal defects by real-time three-dimensional echocardiography. J Am Coll Cardiol. 1995; 25:482–490.
12. Huang X, Shen J, Huang Y, et al. En face view of atrial septal defect by two-dimensional transthoracic echocardiography: comparison to real-time three-dimensional transesophageal echocardiography. J Am Soc Echocardiogr. 2010; 23:714–721.
13. Seo JS, Song JM, Kim YH, et al. Effect of atrial septal defect shape evaluated using three-dimensional transesophageal echocardiography on size measurements for percutaneous closure. J Am Soc Echocardiogr. 2012; 25:1031–1040.
14. Chan KC, Godman MJ, Walsh K, Wilson N, Redington A, Gibbs JL. Transcatheter closure of atrial septal defect and interatrial communications with a new self expanding nitinol double disc device (Amplatzer septal occluder): multicentre UK experience. Heart. 1999; 82:300–306.
15. Acar P. Three-dimensional echocardiography in transcatheter closure of atrial septal defects. Cardiol Young. 2000; 10:484–492.
16. Ko SF, Liang CD, Yip HK, et al. Amplatzer septal occluder closure of atrial septal defect: evaluation of transthoracic echocardiography, cardiac CT, and transesophageal echocardiography. AJR Am J Roentgenol. 2009; 193:1522–1529.
17. Zanchetta M. On-line intracardiac echocardiography alone for Amplatzer Septal Occluder selection and device deployment in adult patients with atrial septal defect. Int J Cardiol. 2004; 95:61–68.
18. Amin Z, Hijazi ZM, Bass JL, Cheatham JP, Hellenbrand WE, Kleinman CS. Erosion of Amplatzer septal occluder device after closure of secundum atrial septal defects: review of registry of complications and recommendations to minimize future risk. Catheter Cardiovasc Interv. 2004; 63:496–502.
19. Divekar A, Gaamangwe T, Shaikh N, Raabe M, Ducas J. Cardiac perforation after device closure of atrial septal defects with the Amplatzer septal occluder. J Am Coll Cardiol. 2005; 45:1213–1218.
20. Sadeghian H, Hajizeinali A, Eslami B, et al. Measurement of Atrial Septal Defect Size: A Comparative Study between Transesophageal Echocardiography and Balloon Occlusive Diameter Method. J Tehran Heart Cent. 2010; 5:74–77.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download