Abstract
Background and Objectives
We investigated the effect of the additional use of abciximab during percutaneous coronary intervention (PCI) on the level of procoagulant microparticles (MPs) in patients with ST-segment elevation myocardial infarction (STEMI) who had undergone primary PCI.
Subjects and Methods
In this study, we studied 86 patients with STEMI (72 men, age 58±13) who had undergone primary PCI. The decision to administer abciximab immediately prior to PCI was left to the discretion of the operator. Blood samples for analysis of MPs were obtained from the femoral artery before and after PCI. MPs with procoagulant potential were measured using a commercial kit. The cellular origins of MPs were determined by antigenic capture with specific antibodies.
Results
Procoagulant MPs captured onto annexin V were not changed significantly after PCI {13.4±13.2 nM vs. 13.2±16.1 nM phosphatidylserine equivalent (PS eq), p=0.479}. Abciximab was used in 30 of 86 patients (35%) immediately prior to PCI. In patients who had undergone PCI without abciximab, no significant change in the level of MPs was observed after PCI. However, in the abciximab group, the level of circulating MPs was significantly decreased after PCI (12.0±10.7 nM vs. 7.8±11.7 nM PS eq, p=0.018). Levels of endothelial- and platelet-derived MPs also showed a significant reduction after PCI in the abciximab group.
Microparticles (MPs) shed from activated or apoptotic cells contain complex procoagulant and proinflammatory properties.1)2) MPs released from various vascular or peripheral blood cells circulate in the blood and can be sequestered in complicated atherosclerotic plaques. The accumulated MPs within atherosclerotic plaques can also be exposed to blood circulation by plaque erosion or rupture.3) Therefore, the levels of circulating procoagulant MPs are elevated in patients with acute coronary syndrome (ACS).4)5) Recently, it has been reported that procoagulant MPs are elevated in the culprit coronary artery in patients with ST-segment elevation myocardial infarction (STEMI), and are reduced after successful primary percutaneous coronary intervention (PCI) with intracoronary aspiration.6)7)
Regarding the effect of the additional use of a GlycoProtein (GP) IIb/IIIa antagonist during primary PCI on the level of MPs, Morel et al.8) reported that in the early period after PCI, lower levels of procoagulant MPs were achieved using abciximab treatment compared with eptifibatide therapy or primary PCI only, without the administration of a GP IIb/IIIa antagonist. However, no data are available that compare MPs levels before and after PCI with additional abciximab treatment. In a subgroup analysis of our recent data, the level of procoagulant MPs in the peripheral arteries was significantly decreased after PCI, compared with the pre-PCI level only in patients who had undergone primary PCI with additional abciximab treatment.7)
In the present study, we investigated the effect of the additional use of abciximab during PCI on the level of procoagulant MPs in patients with STEMI who had undergone primary PCI. The cellular origins of the MPs were determined by antigenic capture with specific antibodies. In addition, we also evaluated whether additional intracoronary aspiration during PCI could reduce the level of post-PCI procoagulant MPs.
We prospectively enrolled 86 consecutive patients with STEMI who had undergone primary PCI from January 2010 to August 2011 at Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. STEMI was defined as resting chest pain lasting ≥30 minutes, together with new or presumed new ST-segment elevation in ≥2 contiguous leads with the cut-off points ≥0.2 mV in leads V1, V2, or V3 and ≥0.1 mV in other leads.9) In all patients, myocardial damage was confirmed by an elevation of creatine kinase-MB (CK-MB) (>2 times the upper reference limit) during the hospital stay. Patients with chronic kidney disease (serum creatinine >2.0 mg/dL), apparent infectious disease, malignancy, or chronic inflammatory disorders were excluded from the study.
The study protocol was approved by our local Institutional Review Board (Gangnam Severance Hospital, Yonsei University College of Medicine), and written informed consent was obtained from each participant.
All patients received a loading dose of oral aspirin (300 mg), clopidogrel (600 mg), and intravenous heparin (10000 IU) prior to PCI. Where necessary, a repeat bolus of heparin was administered to maintain an activated clotting time of 250 to 300 seconds. Coronary angiography was performed by conventional methods through femoral access. A first 20 mL blood sample was obtained through the femoral sheath prior to PCI. Primary PCI was performed according to standard techniques. In some patients, intracoronary aspiration using a monorail aspiration catheter (Export, Medtronic, Minneapolis, MN, USA) was conducted at the discretion of the operator. Any additional use of intravenous GP IIb/IIIa inhibitor was also left to the discretion of the operator during the procedure. Post-PCI blood samples were obtained at the end of PCI from the femoral artery through the vascular sheath.
All blood samples were drawn into evacuated collection tubes containing sodium citrate (0.109 M). The plasma supernatant was quickly decanted following a 15-minute centrifugation at 1500×g at room temperature, and was then again quickly centrifuged for 2 minutes at 13000×g at room temperature. The platelet-poor plasma containing circulating MPs obtained by double centrifugation was then stored in a frozen state at -80℃.
The frozen samples were thawed for 15 minutes at 37℃ immediately prior to analysis. MPs with procoagulant potential were measured using a solid-phase capture assay from a commercial kit (ZYMUPHEN MP-Activity kit; Hyphen BioMed, Neuville-sur-Oise, France). Briefly, MPs were isolated by capture onto immobilized annexin V, and the amount of captured MPs was determined by a prothrombinase assay using their procoagulant potential.10) The cell origins of the MPs were determined by antigenic capture with insolubilized specific antibodies instead of annexin V, using similar solidphase capture methods.10) In this study, the following biotinylated monoclonal antibodies were used: anti-CD31 (endothelial cells), anti-CD42b (endothelial cells) (Abcam, Cambridge, UK), and anti-CD146 (platelets) (Millipore, Billerica, MA, USA). Results were expressed as phosphatidylserine equivalents (PS eq), calculated using the standard calibration curve constructed using liposomes of known concentrations. All tests were performed in duplicate.
Continuous data are expressed as mean±SD and categorical data are presented as numbers and percentages. Differences in categorical variables were analyzed using the chi-square test, and differences in continuous variables were compared between the 2 groups using the unpaired Student's t-test. Levels of MPs before and after PCI were compared using the Wilcoxon's signed rank test. A 2-tailed p of <0.05 was considered to be statistically significant. All statistical analyses were performed with PASW statistics version 18.0 (Statistical Package for the Social Sciences, Inc., Chicago, IL, USA)
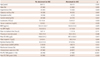
A total of 86 patients (72 men, 58±13 years of age) were enrolled in this study. In 30 of the 86 patients (35%), the GP IIb/IIIa inhibitor was used as an initial bolus of abciximab 0.25 mg/kg, followed by a 12-hour infusion of 0.125 µg/kg/min during the PCI procedure. When patients were divided into 2 groups based on the use of abciximab during PCI, baseline clinical characteristics were not different between the 2 groups except for dyslipidemia. Baseline characteristics are listed in Table 1. Leukocytes count, peak CK-MB, and peak troponin T were higher in patients treated with abciximab. In the abciximab group, more patients showed the initial Thrombolysis in Myocardial Infarction (TIMI) flow 0 or 1 grade than in patients who did not receive abciximab (90% vs. 46%, p<0.001). However, optimal PCI results (TIMI flow 3 grade) were achieved in most patients of both groups (90% vs. 96%, p=0.300).
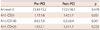
In all STEMI patients, levels of overall circulating MPs captured onto annexin V were not changed significantly after PCI (13.4±13.2 nM vs. 13.2±16.1 nM PS eq, p=0.479) (Table 2). However, circulating MPs captured with anti-CD31 or anti-CD146 were significantly reduced after primary PCI, whereas those captured with anti-CD42b were not (Table 2).
When patients were divided into 2 groups according to the use of abciximab during PCI, no significant change in the level of overall MPs was observed after PCI in patients who had undergone PCI without abciximab (14.1±14.5 nM vs. 16.0±17.4 nM PS eq, p=0.336) (Fig. 1). In the abciximab group, however, the level of circulating MPs was significantly decreased after PCI (12.0±10.7 nM vs. 7.8± 11.7 nM PS eq, p=0.018).
When the levels of MPs captured with different monoclonal antibodies were analyzed, only the level of CD146+ MPs was found to have decreased after PCI in patients who did not receive abciximab (0.5±0.9 nM vs. 0.4±0.5 nM PS eq, p=0.025) (Fig. 2). However, in the abciximab group, the levels of MPs showed a significant reduction after PCI, regardless of their cellular origins.
When levels of MPs captured on annexin V and different monoclonal antibodies were compared according to the use of abciximab, pre-PCI levels of MPs were comparable between the two groups. However, post-PCI levels of total MPs, CD31+MPs, and CD42b+MPs were significantly lower in the abciximab group (Table 3).
Of the 86 patients enrolled, intracoronary aspiration was performed in 73 patients (85%). Therefore, the effect of intracoronary aspiration on the change of MPs was also analyzed. However, there was no significant change observed in the level of circulating MPs before and after PCI in both groups (Fig. 3). When patients were divided into 4 groups according to the use of intracoronary aspiration or abciximab during PCI, the significant reduction of MPs was observed only in patients who had undergone both intracoronary aspiration and abciximab infusion (n=26; 12.7±11.1 nM vs. 8.4±12.4 nM PS eq, p=0.049) (Fig. 4). An insignificant trend of reduction was also observed in patients who received abciximab without intracoronary aspiration (n=4; 7.4±6.3 nM vs. 3.7±4.3 nM PS eq, p=0.068). However, that same trend was not observed in other groups.
The principal finding of this study is that the additional use of abciximab during primary PCI significantly reduced the level of circulating MPs in patients with STEMI, regardless of their cellular origins. In patients who had undergone PCI without abciximab, only the level of MPs captured on anti-CD146 showed a significant reduction after PCI.
In a previous in vitro study, abciximab has been shown to inhibit platelet MPs formation and P-selectin expression in heparin and heparin-induced thrombocytopenia positive serum-induced platelet activation.11) In patients with STEMI treated with primary PCI, it has been reported that the post-PCI level of procoagulant MPs is significantly lowered in the abciximab group compared with the eptifibatide subset or control group.8) However, no data are available comparing MPs levels before and after PCI with additional abciximab treatment.
Recently, our group demonstrated that the level of circulating MPs significantly decreased after PCI in the subgroup that received additional intravenous abciximab treatment during primary PCI, although the level of MPs in coronary arteries showed no significant change due to the use of additional abciximab.7) In the present study, we confirmed these findings in more patients. In addition, we demonstrated that, in the abciximab group, the levels of endothelial-derived MPs were also decreased after PCI, as well as platelet-derived MPs.
It has been shown that abciximab blocks not only the GP IIb/IIIa receptor, but also the expression of Mac-1 and the αvβ3 vitronectin receptor.12)13) Abciximab can reduce endothelial cell activation and membrane shedding14) and attenuate endothelial dysfunction after coronary stenting.15) Therefore, these favorable effects of abciximab may be partially responsible for the reduction of endothelial-derived MPs after PCI.
In this study, abciximab was used at the discretion of the operator and intracoronary aspiration was also performed for most of the patients (26/30; 87%). Therefore, the effect of intracoronary aspiration on the reduction of circulating MPs was also analyzed. However, no significant reduction of the level of MPs was observed in both groups. This result is consistent with our previous report that showed no significant change in the level of MPs in peripheral blood after primary PCI with intracoronary aspiration.7) In addition, the trend of the reduction in the level of MPs was observed in patients who received abciximab without intracoronary aspiration, although the difference was not statistically significant because of the small number of patients in the group.
It has been noted that the level of MPs is elevated in patients with ACS, especially in patients with acute myocardial infarction.5) Moreover, high endothelial-derived MPs levels are associated with highrisk angiographic lesions in ACS,16) or disease severity in acute stroke. 17) Endothelial-derived MPs are also known to be a risk factor for coronary artery disease in patients with diabetes.18) In addition, it has been shown that elevated levels of endothelial-derived MPs can independently predict future cardiovascular events in patients with heart failure19) or pulmonary hypertension.20) However, there are currently no data available to assess the clinical impact or prognostic value of the reduction of circulating MPs by therapeutic agents or procedures. Likewise, the clinical implications and prognostic significance of the early reduction in the level of MPs was not able to be determined in this study.
There are some limitations in this study. Firstly, abciximab was used at the discretion of the operator during the procedure, without randomization. However, the 2 groups, according to the use of abciximab, were comparable in clinical characteristics and baseline levels of circulating procoagulant MPs, regardless of their cellular origins. Secondly, post-PCI samples were obtained immediately after PCI, although intravenous abciximab was used for 24 hours. Therefore, the full effect of abciximab use on the change of the level of MPs over time could not be analyzed. However, the early decrease in the level of MPs during PCI was observed in this study. Lastly, the effects of other medications including antiplatelet and anticoagulant agents on the level of MPs could not be ruled out in this study. However, the same loading dosages of aspirin, clopidogrel, and intravenous heparin were used immediately prior to the 1st sampling.
In conclusion, primary PCI with additional abciximab significantly reduced the level of procoagulant MPs regardless of their cellular origins in patients with STEMI. Further observations in larger studies will be required to elucidate the clinical implications and prognostic significance of the early reduction of the level of MPs by additional GP IIb/IIIa antagonists in patients with STEMI.
Figures and Tables
Fig. 1
Comparison of levels of microparticles captured on immobilized annexin V before and after coronary intervention in patients with ST-segment elevation myocardial infarction who had undergone coronary intervention without abciximab (n=56) or with abciximab (n=30). The line within the box denotes the median. The box spans the Interquartile Range (IQR). The whiskers extend to the minimum or maximum values within 1.5 IQR. PS: phosphatidylserine, PCI: percutaneous coronary intervention.

Fig. 2
Levels of microparticles captured with insolubilized monoclonal anti-CD31 (A), anti-CD146 (B), and anti-CD42b (C) antibodies before and after a coronary intervention in patients with ST-segment elevation myocardial infarction who had undergone coronary intervention without abciximab (n=56) or with abciximab (n=30). The line within the box denotes the median. The box spans the Interquartile Range (IQR). The whiskers extend to the minimum or maximum values within 1.5 IQR. PS: phosphatidylserine, PCI: percutaneous coronary intervention.

Fig. 3
Comparison of levels of microparticles captured on immobilized annexin V before and after coronary intervention in patients with ST-segment elevation myocardial infarction who had undergone coronary intervention without intracoronary aspiration (n=13) or with intracoronary aspiration (n=73). The line within the box denotes the median. The box spans the Interquartile Range (IQR). The whiskers extend to the minimum or maximum values within 1.5 IQR. PS: phosphatidylserine, PCI: percutaneous coronary intervention.

Fig. 4
Comparison of levels of microparticles captured on immobilized annexin V before and after coronary intervention in patients divided into 4 groups according to the use of intracoronary aspiration or abciximab during intervention. The line within the box denotes the median. The box spans the Interquartile Range (IQR). The whiskers extend to the minimum or maximum values within 1.5 IQR. PS: phosphatidylserine, PCI: percutaneous coronary intervention.

Acknowledgments
This study was supported by grants from the Korean Society of Cardiology (Industrial-Educational Cooperation, 2010).
References
1. VanWijk MJ, VanBavel E, Sturk A, Nieuwland R. Microparticles in cardiovascular diseases. Cardiovasc Res. 2003; 59:277–287.
2. Puddu P, Puddu GM, Cravero E, Muscari S, Muscari A. The involvement of circulating microparticles in inflammation, coagulation and cardiovascular diseases. Can J Cardiol. 2010; 26:140–145.
3. Leroyer AS, Isobe H, Lesèche G, et al. Cellular origins and thrombogenic activity of microparticles isolated from human atherosclerotic plaques. J Am Coll Cardiol. 2007; 49:772–777.
4. Mallat Z, Benamer H, Hugel B, et al. Elevated levels of shed membrane microparticles with procoagulant potential in the peripheral circulating blood of patients with acute coronary syndromes. Circulation. 2000; 101:841–843.
5. Bernal-Mizrachi L, Jy W, Jimenez JJ, et al. High levels of circulating endothelial microparticles in patients with acute coronary syndromes. Am Heart J. 2003; 145:962–970.
6. Morel O, Pereira B, Averous G, et al. Increased levels of procoagulant tissue factor-bearing microparticles within the occluded coronary artery of patients with ST-segment elevation myocardial infarction: role of endothelial damage and leukocyte activation. Atherosclerosis. 2009; 204:636–641.
7. Min PK, Kim JY, Chung KH, et al. Local increase in microparticles from the aspirate of culprit coronary arteries in patients with ST-segment elevation myocardial infarction. Atherosclerosis. 2013; 227:323–328.
8. Morel O, Hugel B, Jesel L, et al. Circulating procoagulant microparticles and soluble GPV in myocardial infarction treated by primary percutaneous transluminal coronary angioplasty. A possible role for GPIIb-IIIa antagonists. J Thromb Haemost. 2004; 2:1118–1126.
9. Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined--a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000; 36:959–969.
10. Jy W, Horstman LL, Jimenez JJ, et al. Measuring circulating cell-derived microparticles. J Thromb Haemost. 2004; 2:1842–1851.
11. Jeske WP, Walenga JM, Szatkowski E, et al. Effect of glycoprotein IIb/IIIa antagonists on the HIT serum induced activation of platelets. Thromb Res. 1997; 88:271–281.
12. Simon DI, Xu H, Ortlepp S, Rogers C, Rao NK. 7E3 monoclonal antibody directed against the platelet glycoprotein IIb/IIIa cross-reacts with the leukocyte integrin Mac-1 and blocks adhesion to fibrinogen and ICAM-1. Arterioscler Thromb Vasc Biol. 1997; 17:528–535.
13. Gawaz M, Neumann FJ, Dickfeld T, et al. Vitronectin receptor (alpha(v) beta3) mediates platelet adhesion to the luminal aspect of endothelial cells: implications for reperfusion in acute myocardial infarction. Circulation. 1997; 96:1809–1818.
14. Yeh CH, Peng HC, Huang TF. Accutin, a new disintegrin, inhibits angiogenesis in vitro and in vivo by acting as integrin alphavbeta3 antagonist and inducing apoptosis. Blood. 1998; 92:3268–3276.
15. Aymong ED, Curtis MJ, Youssef M, et al. Abciximab attenuates coronary microvascular endothelial dysfunction after coronary stenting. Circulation. 2002; 105:2981–2985.
16. Bernal-Mizrachi L, Jy W, Fierro C, et al. Endothelial microparticles correlate with high-risk angiographic lesions in acute coronary syndromes. Int J Cardiol. 2004; 97:439–446.
17. Simak J, Gelderman MP, Yu H, Wright V, Baird AE. Circulating endothelial microparticles in acute ischemic stroke: a link to severity, lesion volume and outcome. J Thromb Haemost. 2006; 4:1296–1302.
18. Koga H, Sugiyama S, Kugiyama K, et al. Elevated levels of VE-cadherinpositive endothelial microparticles in patients with type 2 diabetes mellitus and coronary artery disease. J Am Coll Cardiol. 2005; 45:1622–1630.
19. Nozaki T, Sugiyama S, Sugamura K, et al. Prognostic value of endothelial microparticles in patients with heart failure. Eur J Heart Fail. 2010; 12:1223–1228.
20. Amabile N, Heiss C, Chang V, et al. Increased CD62e(+) endothelial microparticle levels predict poor outcome in pulmonary hypertension patients. J Heart Lung Transplant. 2009; 28:1081–1086.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download