Abstract
Background and Objectives
We investigated the predictors of the recovery of depressed left ventricular ejection fraction (LVEF) in patients with moderate or severe left ventricular (LV) systolic dysfunction after acute myocardial infarction (MI).
Subjects and Methods
We analyzed 1307 patients, who had moderately or severely depressed LVEF (<45%) on echocardiography soon after acute MI and who underwent a follow-up echocardiography, among 27369 patients from the Korea Working Group on the Myocardial Infarction Registry. Patients were categorized into two groups according to recovery of LVEF: group I with consistently depressed LVEF (<45%) at the follow-up echocardiography and group II with a recovery of LVEF (≥45%).
Results
Recovery of LV systolic dysfunction was observed in 51% of the subjects (group II, n=663; ΔLVEF, 16.2±9.3%), whereas there was no recovery in the remaining subjects (group I, n=644; ΔLVEF, 0.6±7.1%). In the multivariate analysis, independent predictors of recovery of depressed LVEF were as follows {odds ratio (OR) [95% confidence interval (CI)]}: moderate systolic dysfunction {LVEF ≥30% and <45%; 1.73 (1.12-2.67)}, Killip class I-II {1.52 (1.06-2.18)}, no need for diuretics {1.59 (1.19-2.12)}, non-ST-segment elevation MI {1.55 (1.12-2.16)}, lower peak troponin I level {<24 ng/mL, median value; 1.55 (1.16-2.07)}, single-vessel disease {1.53 (1.13-2.06)}, and non-left anterior descending (LAD) culprit lesion {1.50 (1.09-2.06)}. In addition, the use of statin was independently associated with a recovery of LV systolic dysfunction {OR (95% CI), 1.46 (1.07-2.00)}.
The left ventricular ejection fraction (LVEF) is the most important predictor of morbidity and mortality after acute myocardial infarction (MI).1-3) The left ventricular systolic dysfunction during the early phase of acute MI may be sustained or progressively aggravated by the process of ventricular remodeling, which is related to the risk of congestive heart failure and death.4)5) However, improvements in left ventricular function can be apparent after acute MI, through mechanisms such as the gradual recovery of myocardial stunning or hibernation, and may have a beneficial effect on patient survival.6)7)
Thus, it is important to determine which patient may have a sustained left ventricular dysfunction or which variables can predict a change in the LVEF. Predictors of a change in the LVEF may have prognostic significance and important implications for the therapeutic approach to use. The aim of this study is, therefore, to determine the clinical, therapeutic, and angiographic predictors of recovery of depressed LVEF in patients with moderate or severe left ventricular systolic dysfunction following acute MI.
From November 2005 to March 2012, a total of 1307 patients with moderate or severe left ventricular systolic dysfunction after the first acute MI from the Korean Acute Myocardial Infarction Registry (KAMIR) and Korean Myocardial Infarction (KorMI) registry were enrolled. The KAMIR and KorMI registry is a prospective, observational, multi-center registry reflecting current practices of management, risk factors, and clinical outcomes in Korean patients with acute MI. The registry was supported by the Korean Working Group of Acute Myocardial Infarction. Participating centers included 53 community and teaching hospitals with facilities for primary percutaneous coronary intervention and on-site cardiac surgery. A well-trained study coordinator collected the data based on standard protocol. Each ethics committee of the participating hospitals approved the study protocol. Fig. 1 shows the flow chart of this study. Moderate or severe systolic dysfunction was defined as the LVEF <45% or <30%, respectively, based on the current guidelines of the American Society of Echocardiography and European Society of Echocardiography.8) Patients with a history of ischemic heart disease or heart failure were excluded. Patients with the first acute MI, who had moderately or severely depressed LVEF less than 45% on echocardiography at the hospital-stay and who underwent serial echocardiography after discharge, were selected and constituted the eligible 1307 patients of the 27369 total registered patients. Patients were categorized into two groups according to the recovery of LVEF: group I (n=644, 49.3%) with consistently depressed LVEF less than 45% at the follow-up echocardiography, and group II (n=663, 50.7%) with a recovery of LVEF more than or equal to 45%. Demographic data, laboratory values including cardiac enzymes, therapeutic data, angiographic and procedural details were available. Two-dimensional echocardiography was performed at the hospital-stay and follow-up period. Baseline echocardiography was performed at 1.2±1.3 days (median, 1.0 days; interquartile range, 0.0-2.0 days) from admission. Mean interval between serial echocardiography was 221.9±148.7 days (median, 208.0 days; interquartile range, 114.0-297.0 days).
All continuous variables were presented as mean±standard deviation for the normally distributed data or median (interquartile range) for the skewed data. Categorical variables were described with absolute and relative (percentage) frequencies. The two groups were compared with respect to the patients' clinical characteristics, and baseline echocardiographic and angiographic data using the unpaired t-test for continuous and Pearson's χ2 test for categorical variables were employed. Multivariate logistic regression analysis was used to examine the predictors of recovery of depressed LVEF. A p less than 0.05 was considered statistically significant. Analyses were performed with the Statistical Package for the Social Sciences (SPSS) version 18.0 statistical package (SPSS Inc., Chicago, IL, USA).
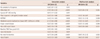
Table 1 shows the clinical characteristics of patients between both groups. There were no significant differences in age, gender, and body mass index between the two groups. Other cardiovascular risk factors, including smoking, diabetes mellitus, hypertension, and dyslipidemia, were not significantly different in both groups. Complaints of dyspnea or frank pulmonary edema and cardiogenic shock (Killip class III-IV) during acute MI was significantly more prevalent among group I patients, compared with those in group II. Systolic blood pressure (BP) and diastolic BP were not significantly different between both groups, although systolic BP tended to be lower in group I than in group II. However, there were more patients with systolic BP less than 90 mm Hg in group I than in group II (6.6% vs. 3.5%, p=0.009). Heart rate was significantly faster in group I than in group II (87.0±21.1 vs. 82.4±19.1, p<0.001). In addition, there were significantly more patients with ST-segment elevation MI (73.8% vs. 66.1%, p=0.001) in group I, compared with that of group II. Regarding discharge medications, loop diuretics were more frequently prescribed in group I (47.5% vs. 35.1%, p<0.001) and β-blocker or statin was more frequently prescribed in group II (71.8% vs. 78.3%, 69.3% vs. 76.3%, respectively, p<0.01 for both). There was no significant difference in the frequency of prescription of angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers in both groups.
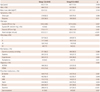
Table 2 illustrates the laboratory data, including myonecrosis biomarkers or metabolic parameters. The peak level of creatine kinase-myocardial band and troponin I were significantly higher in group I than in group II {102.4 ng/mL (20.0-292.0) vs. 61.0 ng/mL (11.6-179.0), 31.0 ng/mL (4.8-86.3) vs. 16.5 ng/mL (3.9-50.0), respectively, p<0.001 for both}. Group I had significantly higher levels of N-terminal pro-B-type natriuretic peptide, compared with that of group II {1729.0 pg/mL (276.0-5304.0) vs. 1399.0 pg/mL (227.5-3655.3), p=0.031}. In addition, group I had significantly higher levels of glucose on admission (189.7±82.5 mg/dL vs. 178.1±80.2 md/dL, p=0.011) and had a tendency of higher levels of high-sensitivity C-reactive protein {1.80 mg/dL (0.32-8.00), 1.07 mg/dL (0.30-6.61), p=0.075}, compared with those of group II.
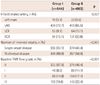
Group I had more left anterior descending (LAD) culprit lesions than group II (72.7% vs. 65.5%, p=0.037). Multivessel disease or baseline Thrombolysis in Myocardial Infarction flow grade 0 of infarct-related artery was more prevalent in group I than in group II (66.9% vs. 56.6%, 57.5% vs. 45.4%, respectively; p<0.001 for both) (Table 3). The LVEF at the baseline echocardiography was significantly lower in group I, compared with that in group II (35.3±6.7% vs. 38.0±5.8%, p<0.001) (Table 4). In addition, group I had a more dilated left ventricle than group II at the baseline. The change of LVEF was 0.6±7.1% and 16.2±9.3% in group I and group II, respectively (p<0.001). At the follow-up echocardiography, the left ventricular end-diastolic and end-systolic volumes were significantly increased from the baseline by 11.7±38.8 mL and 7.1±29.5 mL in group I, and were significantly reduced from the baseline by 3.7±31.8 mL and 15.4±24.9 mL in group II, respectively (p<0.01 for both).
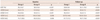
The predictors of recovery of depressed LVEF were as listed in Table 5. By multivariate logistic regression analysis, moderate systolic dysfunction (LVEF ≥30% and <45%) was the independent predictor for the recovery of depressed LVEF with an odds ratio (OR) of 1.73 {95% confidence interval (CI), 1.12-2.67, p=0.013}. Non-ST-segment elevation MI, peak troponin I level less than 24 ng/mL (median value), and Killip class I-II were also independently associated with the recovery of systolic dysfunction {OR (95% CI), 1.55 (1.12-2.16), 1.55 (1.16-2.07), 1.52 (1.06-2.18), respectively; p<0.05 for all}. Single-vessel disease and non-LAD culprit lesions were independent predictors for contractile recovery {OR (95% CI), 1.53 (1.13-2.06), 1.50 (1.09-2.06), respectively; p<0.05 for both}. In addition, the lack of need for diuretics at discharge and the use of statin were significantly related with the recovery of depressed LVEF {OR (95% CI), 1.59 (1.19-2.12), 1.46 (1.07-2.00), respectively; p<0.05 for both}.
The independent predictors of improvement of LVEF more than or equal to 10% in terms of absolute value were as shown in Table 6. As the results of multivariate analysis for recovery of depressed LVEF, peak level of troponin I less than 24 ng/mL, use of statin, and non-ST-segment elevation MI were also independent predictors of improvement of LVEF more than or equal to 10%. However, contrary to the independent predictors of recovery of depressed LVEF, severe systolic dysfunction (LVEF <30%) was the independent predictor of improvement of LVEF more than or equal to 10% with an OR of 2.41 (95% CI, 1.58-3.67, p<0.001). In Pearson's correlation analysis, the change of LVEF (follow-up LVEF-baseline LVEF) was negatively correlated with the baseline LVEF (r=-0.236, p<0.001).
Among the study subjects who had a baseline LVEF of less than 45% soon after acute MI, left ventricular systolic dysfunction was recovered (follow-up LVEF ≥45%) in almost 50% (group II) after a median follow-up of 222 days, which was comparable to a previous study.9) By multivariate analysis, several variables, as follows, were identified as independent predictors of contractile recovery, which were closely related with less severe heart failure or a small extent of myonecrosis: moderate systolic dysfunction, Killip class I-II, no need for diuretics, lower peak level of troponin I, non-ST-segment elevation MI, single-vessel disease, and non-LAD culprit lesions. In addition, the use of statin was independently associated with the contractile recovery of the left ventricle.
The specific predictors of potential contractile recovery have prognostic significance and important implications for the therapeutic approach used. However, previous studies in literature have not suggested consistent predictors sufficient to forecast contractile recovery. Ongoing with our results, two studies demonstrated an association between contractile recovery and a higher baseline left ventricular systolic function.10)11) Leclercq et al.10) revealed that contractile recovery was independently associated with higher LVEF, the presence of collateral blood flow, and dobutamine responsiveness at the dobutamine echocardiography. Furthermore, Abdel-Salam and Nammas11) observed that higher LVEF and a lower wall motion score index at the baseline echocardiography were significantly related to myocardial contractile recovery after percutaneous coronary intervention. More severe left ventricular systolic dysfunction most likely implicates larger infarct size and wider expansion of the infarcted zone. The larger infarct size is significantly correlated with a higher peak level of myonecrosis biomarkers.12) The peak creatine kinase level was the independent predictor of the functional recovery of the left ventricle, probably indicating viable myocardium.13)14) Absolute infarct size measured by gadolinium contrast-enhanced magnetic resonance imaging was larger in the ST-segment elevation MI than in the non-ST-segment elevation MI.15) In addition, patients with more severe left ventricular systolic dysfunction may present more symptoms or signs of heart failure, including pulmonary congestion (Killip class III) or cardiogenic shock (Killip class IV), and may be prescribed less frequently with β-blockers or more diuretics. In our study, several independent predictors of the recovery of systolic dysfunction were closely related to less severe heart failure at the time of presentation and a smaller extent of myonecrosis, including non-ST-segment elevation MI, lower Killip class (I-II), lower peak troponin I level, or the frequency of prescribed medications such as the lower need for diuretics.
Nonetheless, other studies were unable to demonstrate a relationship between contractile recovery and baseline LVEF.9)16)17) Auerbach et al.17) found no relation between contractile recovery and the basal LVEF, but demonstrated that myocardial viability detected by positron emission tomography could predict the improvement of left ventricular function in patients with ischemic cardiomyopathy. Ottervanger et al.9) assessed clinical variables associated with the recovery of left ventricular function measured by radionuclide ventriculography at day 4 and after 6 months in 600 patients with acute MI, all treated by primary percutaneous coronary intervention. They demonstrated that anterior MI, single-vessel disease, and initially depressed LVEF less than or equal to 40% were independently associated with the recovery of left ventricular function, suggesting stunning might be prolonged in larger infarcts. However, these results may be applied to patients with ST-segment elevation MI who achieved early and complete patency of infarct-related artery and may be affected by the time at which baseline LVEF was measured. In the multivariate analysis and correlation analysis, initially depressed LVEF less than 30% was independently related with an improvement of LVEF more than or equal to 10% (absolute value) and there was a negative correlation between the change of LVEF and the baseline LVEF. Therefore, the baseline LVEF as a predictor of an improvement or recovery of LVEF may be dependent on the index of contractile recovery.
In this study, the prescription of statin was also an independent predictor of the recovery of systolic dysfunction after acute MI. Statin treatment improved survival in patients with not only acute MI but also ischemic and non-ischemic heart failure.18)19) In addition, the risk of developing ischemic heart failure was reduced in patients with coronary artery disease by statin treatment.20)21) Sola et al.22) demonstrated that atorvastatin improved LVEF and attenuated adverse left ventricular remodeling in patients with non-ischemic heart failure, decreasing the level of pro-inflammatory markers. Many pleiotropic effects of statin, such as improving endothelial function and providing plaque stabilization and anti-inflammatory effects, might be effective in improving myocardial function, and also in retarding the progression of heart failure. However, a large randomized prospective study is required to determine the role of statin in the recovery of left ventricular systolic dysfunction following acute MI.
This study has several limitations. First, the follow-up echocardiography was performed only among one quarter of the patients with depressed LVEF, giving rise to a selection bias. Second, the baseline and follow-up echocardiography were performed at a variety of time intervals after index MI, which might have underestimated the recovery of LVEF or might not have reflected the true recovery of each subject during the follow-up period. Third, in our study, adverse events, such as re-infarction or revascularization during the follow-up period, were not considered, which may affect the change of left ventricular systolic function. Fourth, we had no data on left ventricular diastolic function or regional wall motion abnormalities. Moreover, we had no data on the extent of functionally viable myocardium, such as stunned or hibernating myocardium.
In conclusion, future contractile recovery of LV systolic dysfunction following acute MI was significantly predicted by less severe heart failure at the time of presentation, the smaller extent of myonecrosis, or non-LAD culprit lesions rather than LAD lesions.
Figures and Tables
 | Fig. 1The flow chart of the study. KAMIR: Korean Acute Myocardial Infarction Registry, KorMI: Korean Myocardial Infarction, LVEF: left ventricular ejection fraction. |
Table 5
Predictors of recovery (follow-up LVEF ≥45%) of depressed LVEF in patients with moderate or severe systolic dysfunction (baseline LVEF <45%) by univariate and multivariate logistic regression analysis
References
1. Risk stratification and survival after myocardial infarction. N Engl J Med. 1983; 309:331–336.
2. White HD, Norris RM, Brown MA, Brandt PW, Whitlock RM, Wild CJ. Left ventricular end-systolic volume as the major determinant of survival after recovery from myocardial infarction. Circulation. 1987; 76:44–51.
3. St John Sutton M, Pfeffer MA, Plappert T, et al. Quantitative two-dimensional echocardiographic measurements are major predictors of adverse cardiovascular events after acute myocardial infarction. The protective effects of captopril. Circulation. 1994; 89:68–75.
4. Gaudron P, Eilles C, Kugler I, Ertl G. Progressive left ventricular dysfunction and remodeling after myocardial infarction. Potential mechanisms and early predictors. Circulation. 1993; 87:755–763.
5. Bolognese L, Cerisano G, Buonamici P, et al. Influence of infarct-zone viability on left ventricular remodeling after acute myocardial infarction. Circulation. 1997; 96:3353–3359.
6. Christian TF, Behrenbeck T, Pellikka PA, Huber KC, Chesebro JH, Gibbons RJ. Mismatch of left ventricular function and infarct size demonstrated by technetium-99m isonitrile imaging after reperfusion therapy for acute myocardial infarction: identification of myocardial stunning and hyperkinesia. J Am Coll Cardiol. 1990; 16:1632–1638.
7. Wijns W, Vatner SF, Camici PG. Hibernating myocardium. N Engl J Med. 1998; 339:173–181.
8. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005; 18:1440–1463.
9. Ottervanger JP, van't Hof AW, Reiffers S, et al. Long-term recovery of left ventricular function after primary angioplasty for acute myocardial infarction. Eur Heart J. 2001; 22:785–790.
10. Leclercq F, Messner-Pellenc P, Moragues C, et al. Myocardial viability assessed by dobutamine echocardiography in acute myocardial infarction after successful primary coronary angioplasty. Am J Cardiol. 1997; 80:6–10.
11. Abdel-Salam Z, Nammas W. Predictors of myocardial contractile recovery after coronary revascularization in patients with prior myocardial infarction. Cardiovasc Revasc Med. 2010; 11:2–7.
12. Gibbons RJ, Valeti US, Araoz PA, Jaffe AS. The quantification of infarct size. J Am Coll Cardiol. 2004; 44:1533–1542.
13. Solomon SD, Glynn RJ, Greaves S, et al. Recovery of ventricular function after myocardial infarction in the reperfusion era: the healing and early afterload reducing therapy study. Ann Intern Med. 2001; 134:451–458.
14. Bauters C, Fertin M, Delhaye C, et al. Late recovery in left ventricular systolic function after discharge of patients with a first anterior myocardial infarction. Arch Cardiovasc Dis. 2010; 103:538–545.
15. Steen H, Futterer S, Merten C, Jünger C, Katus HA, Giannitsis E. Relative role of NT-pro BNP and cardiac troponin T at 96 hours for estimation of infarct size and left ventricular function after acute myocardial infarction. J Cardiovasc Magn Reson. 2007; 9:749–758.
16. Eitzman D, al-Aouar Z, Kanter HL, et al. Clinical outcome of patients with advanced coronary artery disease after viability studies with positron emission tomography. J Am Coll Cardiol. 1992; 20:559–565.
17. Auerbach MA, Schöder H, Hoh C, et al. Prevalence of myocardial viability as detected by positron emission tomography in patients with ischemic cardiomyopathy. Circulation. 1999; 99:2921–2926.
18. Stenestrand U, Wallentin L. Swedish Register of Cardiac Intensive Care (RIKS-HIA). Early statin treatment following acute myocardial infarction and 1-year survival. JAMA. 2001; 285:430–436.
19. Horwich TB, MacLellan WR, Fonarow GC. Statin therapy is associated with improved survival in ischemic and non-ischemic heart failure. J Am Coll Cardiol. 2004; 43:642–648.
20. Kjekshus J, Pedersen TR, Olsson AG, Faergeman O, Pyörälä K. The effects of simvastatin on the incidence of heart failure in patients with coronary heart disease. J Card Fail. 1997; 3:249–254.
21. Aronow WS, Ahn C. Frequency of congestive heart failure in older persons with prior myocardial infarction and serum low-density lipoprotein cholesterol > or = 125 mg/dl treated with statins versus no lipid-lowering drug. Am J Cardiol. 2002; 90:147–149.
22. Sola S, Mir MQ, Lerakis S, Tandon N, Khan BV. Atorvastatin improves left ventricular systolic function and serum markers of inflammation in nonischemic heart failure. J Am Coll Cardiol. 2006; 47:332–337.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download