Abstract
Brugada syndrome is a life threatening disease that is usually overlooked during emergency service admissions. It is characterized by typical electrocardiography resembling right bundle branch block, static or dynamic ST-segment elevation in leads V 1-3. There is familial tendency in some cases. A majority of patients have a structurally normal heart and are likely to remain asymptomatic, however they may present to emergency departments with syncope and various serious arrhythmias. Therefore it is crucially important for emergency medicine physicians not to omit this potential diagnosis. Herein we report a case with Brugada syndrome which was iatrogenically unmasked after propafenone administration for atrial fibrillation.
Brugada syndrome, first described in 1992, is a life threatening disease and is usually overlooked during emergency service admissions.1) It is characterized by typical electrocardiography (ECG) resembling right bundle branch block (RBBB), static or dynamic ST-segment elevation in leads V 1-3. There is familial tendency in some cases.2) A majority of patients have a structurally normal heart and are likely to remain asymptomatic, however they may present to emergency departments with syncope and various arrhythmias (atrial fibrillation, ventricular tachycardia, ventricular fibrillation-cardiac arrest and etc.).1)2) Therefore it is crucially important for emergency medicine physicians not to omit this potential diagnosis. Herein we report a case with Brugada syndrome which was iatrogenically unmasked after propafenone administration for atrial fibrillation.
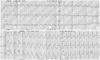
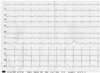
A 62-year-old male presented to the emergency department of a local hospital complaining of palpitation. Because emergency department physicians interpreted the ECG as indicating atrial fibrillation, they administered intravenous propafenone (Fig. 1). After this, the patient experienced dizziness and became hypotensive (blood pressure: 80/50 mm Hg). ECG after propafenone infusion showed an RBBB pattern, ST-segment elevation in leads V 1-3 and ST-segment depression in leads DII, DIII and aVF (Fig. 2). He was thus immediately transferred to our center with the diagnosis of acute myocardial infarction. On admission to our center he had palpitation and mild chest pain. Other than the above mentioned characteristics, ECG revealed atrial fibrillation with a ventricular rate of 155/min. The remainder of the physical examination results were within normal limits. We performed coronary angiography, which was normal. Given that he was symptomatic and hypotensive, direct current cardioversion was performed (100 joules). After shock, the ECG was in sinus rhythm and compatible with Brugada syndrome (Fig. 3). After cardioversion, his symptoms subsided and blood pressure returned to within the normal range. His transthoracic echocardiography, electrolytes and cardiac enzymes were all normal. ECG changes were in accordance with iatrogenic unmasking of concealed type Brugada syndrome. Due to ethical reasons we did not give additional propafenone for challenge. From acquiring detailed history, we learnt that one of his sisters had the diagnosis of Brugada syndrome (Fig. 4). During family screening, we found that his daughter also had the asymptomatic type 2 ECG pattern of Brugada. We recommended him for further electrophysiologic evaluation for possible ventricular arrhythmia detection and risk stratification.
In the present paper, we report a case with Brugada syndrome which was iatrogenically unmasked after propafenone administration for atrial fibrillation. As described in the introduction, the syndrome is commonly overlooked at admission but has several important diagnostic features. It is more common in males and Asian populations.1)2)
In Brugada syndrome there are three typical types of repolarization presentation, based on the appearance of the ST-segments in leads V 1-3. Type 1 has ST-segment elevation, ending with a negative T wave, forming a "coved" appearance. Type 2 has a downsloping ST-segment elevation above baseline forming a "saddle back" ST appearance. Type 3 has the same saddleback appearance as Type 2, but with less ST-segment elevation. Type 1 ECG is more diagnostic for Brugada syndrome. ECG readings are dynamic and may transform from one type to another or may even completely normalize. Increased vagal activity, fever, tricyclic antidepressant agents, or class I A, IC and III antiarrhythmic agents may unmask the ECG similarly to that which occurred in our case.3)4)
In conclusion, in case of admission with atrial fibrillation to emergency department, a commence of class IC antiarrhythmic agent in order to return to normal sinus rhythm may unmask concealed Brugada syndrome. The appearance of post treatment ST-segments elevation in leads V 1-3 with RBBB patterns should alert emergency physicians so that they do not omit this life threatening disease.
Figures and Tables
References
1. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992; 20:1391–1396.
2. Brugada J, Brugada R, Brugada P. Right bundle-branch block and ST-segment elevation in leads V1 through V3: a marker for sudden death in patients without demonstrable structural heart disease. Circulation. 1998; 97:457–460.
3. Antzelevitch C. The Brugada syndrome. J Cardiovasc Electrophysiol. 1998; 9:513–516.
4. Chutani S, Imran N, Grubb B, Kanjwal Y. Propafenone-induced Brugada-like ECG changes mistaken as acute myocardial infarction. Emerg Med J. 2008; 25:117–118.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download