Abstract
Background and Objectives
The proximal portion of the abdominal aorta (AA) is characterized by minimal arteriosclerosis compared with other aortic segments. To assess the clinical usefulness of this characteristic, the correlation between ultrasonographically measured proximal AA stiffness and brachial-ankle pulse wave velocity (baPWV) was examined.
Subjects and Methods
285 subjects were analyzed, half with hypertension and half with normal blood pressure. Proximal AA was examined using ultrasonography; strain, distensibility, elastic modulus, and the stiffness index were determined. After adjustment for age, gender, body mass index (BMI), systolic blood pressure (SBP), and heart rate, the relationships between baPWV and all these parameters were tested.
Results
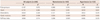
The mean age of the study subjects was 58.1±12.8 years and the mean BMI was 24.3±3.8 kg/cm2. 58.9% of the subjects were female. 42.8% were hypertensive subjects. Among the hypertensive subjects, 56.0% were taking antihypertensive medication. Adjusted partial correlation coefficients for the relationship between baPWV with strain, distensibility, elastic modulus, and the stiffness index of the proximal AA were -0.203 (p=0.01), -0.121 (p=0.129), 0.304 (p=0.0001), and 0.299 (p=0.0001), respectively, in normotensive subjects. In the multivariate analyses, such correlations were observed mainly in the normotensive group, whereas there was no association among hypertensive subjects regardless of antihypertensive medication status.
Aortic stiffness is known to be associated with cardiovascular outcomes. Pulse wave velocity (PWV) is one of the best ways to measure aortic stiffness. Aortic stiffness measured by PWV is regarded as one of the prognostic markers of cardiovascular diseases.1) In addition, aortic stiffness can also be assessed by analyzing strain in various parts of the aorta.2-5) This can be measured directly using ultrasound or magnetic resonance imaging,2) which are familiar tools in clinical practice. In general, the abdominal aorta (AA) is more susceptible to increased stiffness due to degenerative changes or aging than the more proximal or ascending parts, because the elastic fiber composition and the susceptibility to ischemic damage from atherosclerosis differ.6)7)
In a recent necropsy study of Korean subjects, the proximal portion of the AA was found to display minimal atherosclerosis compared to other segments such as the ascending or proximal parts or the distal part of the AA.8) This observation suggests that an examination of the proximal part of the AA may be more useful for the measurement of aortic stiffness, because any structural changes, such as severe atherosclerosis or aneurysmal changes, can make it difficult to measure the strain.
Carotid-femoral PWV (cfPWV) is the standard measure of aortic stiffness. However, from a practical point of view, cfPWV has some limitations, such as requiring a long time for measurement, examiner variability, and inconvenience of exposing the femoral site.9) Practically, brachial-ankle PWV (baPWV), on the other hand, does not require exposure of the femoral site and is a more feasible measure of aortic stiffness than cfPWV. baPWV is a measure of the pulse wave propagation velocity from the point of the aorta where the pulse wave arrives during the time period of the same pulse wave travel to the brachial artery to the ankle. Although baPWV is also affected by the characteristics of the peripheral arteries and the inferior measure of the aortic stiffness compared to cfPWV, baPWV has been validated mainly by comparison with cfPWV, with which it shows a moderate correlation.10) Hence, at least in part, baPWV can reflect the characteristics of the aorta. Moreover, the validity of baPWV as a marker for cardiovascular diseases has been reported in population studies.11) To investigate the usefulness of measurement of proximal AA distensibility, we examined the relationship between the stiffness parameters for the proximal AA and baPWV as the partial measure of aortic stiffness.
Data were prospectively collected from 290 consecutive patients (selected from an initial cohort of 396) who underwent echocardiography after fasting, in hypertension clinics at the Hanyang University Medical Center, Seoul, Korea from February 1st to May 31st, 2009. During the study period, 114 cases were referred from a health promotion center and local clinic for an evaluation of atypical chest symptoms, palpitation, electrocardiographic changes without symptoms, and abnormal blood pressure or laboratory findings.
Clinical exclusion criteria were the refusal to provide informed consent, incomplete clinical data, patients with exposure to nicotine smoking or drinking coffee one hour before the study, and patients with significant skin diseases, joint deformity, renal insufficiency (estimated glomerular filtration rate <60 mL/min), atrial fibrillation, valvular heart disease, and unstable coronary artery disease.
Echocardiographic exclusion criteria were moderate or severe valvular dysfunction, systolic dysfunction characterized by an ejection fraction below 55% as indicated by M-mode measurement, regional wall motion abnormality, moderate or large pericardial effusion, cardiomyopathy, aortic aneurysm, right side heart failure, or pulmonary hypertension. Patients with an ankle-brachial index less than 0.95 were also excluded from the study.
Clinical information was collected via interviews with the participants and from medical records. Body mass index (BMI) was calculated as weight in kg/(height in meters)2 and blood pressure was measured according to current guidelines. Blood chemistry data on fasting blood glucose, lipid profiles, creatinine, and hemoglobin were collected from patient medical records. Only current smokers were defined as smokers. Hypertensive patients were defined as those with systolic blood pressure (SBP) ≥140 mm Hg, diastolic blood pressure (DBP) ≥90 mm Hg, or those taking antihypertensive medications. Patients with diabetes mellitus were defined as those with fasting blood glucose >126 mg/dL, HbA1C >6.5%, or those taking antidiabetic medications or insulin.
Dyslipidemia was defined as total cholesterol ≥240 mg/dL, low density lipoprotein-cholesterol (LDL-C) ≥160 mg/dL, high density lipoprotein-cholesterol <40 mg/dL in males and <50 mg/dL in females, or triglyceride ≥150 mg/dL. A history of ischemic heart disease and/or cerebrovascular accident was determined through interviews.
The proximal AA was examined at the epigastrium for changes in diameter during the cardiac cycle using an echocardiography machine (iE33, Philips®). Unlike the ascending aorta, the posterolateral wall motion of the proximal AA is limited by the spine, so that most of the wall excursion during a cardiac cycle is observed in the anterior wall. By targeting the spine and the diaphragm and tilting the projection slightly to the right side, proximal AA wall excursions were recorded just below the diaphragm, in the suprarenal portion of the AA (Fig. 1).
All participants were examined by a single examiner, and aortic dimensions were measured by a single individual in an off-line procedure using Infinity® DICOM Software (Infinity Inc., Korea). The minimal diastolic proximal AA diameter (AAoD) was measured at the time of QRS onset, and the maximal systolic proximal AA diameter (AAoS) was measured at the time of peak T wave in the electrocardiography recording from the trailing edge of the anterior wall to the leading edge of the posterior wall, over three cycles. Intra-observer Pearson correlation coefficients for repeated measurements of aortic dimensions in 30 subjects were 0.89 and 0.87, respectively, for diastolic and systolic diameters.
A preliminary study to calculate the Pearson correlation coefficient between proximal AA strain and aortic strain measured on the ascending aorta at a level 3 cm distal to the aortic annulus revealed a coefficient of 0.322 (p=0.018, n=50).
The stiffness parameters for the proximal AA were calculated as follows:
Brachial-ankle pulse wave velocity was measured upon the completion of echocardiography after five minutes of rest in the supine position using a VP-2000™ (Colin Co. Ltd., Komaki, Japan), as described in a previous study.19) The mean values of the right and left baPWV were used for statistical analysis. All measurements were performed by a single examiner. For 17 subjects in the repeated measurement, Cronbach alpha was 0.978 and the repeatability coefficient was 186.4 cm/sec.
Heart-carotid PWV (hcPWV), heart-femoral PWV (hfPWV), and cfPWV were also measured to allow for an assessment of the correlation between baPWV and those particular parameters. Measurements were performed on the left side using an applanation tonometry probe.20)21) The Pearson correlation coefficients for the relationship of baPWV with hcPWV, hfPWV, and cfPWV were 0.580 (p<0.001), 0.423 (p<0.05), and 0.577 (p<0.001), respectively.
The study protocol was reviewed and approved by the Institutional Review Board of the Hanyang University Medical Center in Seoul, and each participant provided informed consent.
The sample size was calculated from the expected Pearson correlation coefficients for the relationship of age with proximal AA strain and baPWV of 0.5 and 0.3. A two-tailed difference between the two correlation coefficients was expected to be detected at the level of alpha=0.05, with a value for 1-beta of 0.9.22) The sample size was 279 when the correlation coefficient between proximal AA strain and baPWV was 0.3.
For the analysis of the correlation between baPWV and the stiffness parameters for the proximal AA partial correlation coefficients, adjusted for age, gender, and SBP, were calculated for all subjects, normotensive/hypertensive patients, and treated/untreated patients (with antihypertensive medication). Partial correlation coefficients according to gender were generated by adjusting for age and SBP.
Multiple regression analyses were performed to separately examine the factors influencing each proximal AA stiffness parameter. To test the main hypothesis, the parameters for the stiffness parameters for the proximal AA were set as the dependent variables in each multiple linear regression model. baPWV was set as an independent variable along with other independent variables, such as age, gender, BMI, SBP, heart rate, total cholesterol, and fasting blood glucose. baPWV values adjusted for age, gender, BMI, SBP, and heart rate were compared according to the quartiles of each proximal AA stiffness parameter using analysis of variance and general linear models. A p<0.05 was regarded as statistically significant.
All statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) software package 15th edition (SPSS Inc., Chicago, IL, USA), and data are expressed as mean±standard deviation.
The mean age of the study subjects was 58.1±12.8 years and the mean BMI was 24.3±3.8 kg/cm2. 58.9% of the subjects were female. Hypertension was noted in 122 subjects (42.8%). The proportion of current smokers was 13.6% (32 males and 7 females). Frequencies of essential hypertension, dyslipidemia, and diabetes were 49.5%, 58.9%, and 14.7%, respectively. Histories of coronary artery disease and stroke were observed in 10.5% and 2.4% of the subjects, respectively.
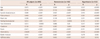
Table 1 shows the general characteristics of the subjects and compares these characteristics between males and females. As can be seen in the table, on average, females had higher pulse pressure, total cholesterol level, and LDL level than the male subjects.
Table 2 shows the comparison between hypertensive and normotensive subjects and between hypertensive subjects according to antihypertensive medication status. SBP in hypertensive subjects was the highest in untreated hypertensive at 137.7±18.8, whereas the control rate of hypertension was 61/132 (46.2%). Among the hypertensive patients, 56.0% (74/122) were taking antihypertensive medication. baPWV was also higher in hypertensive subjects. As shown in Table 2, the proportion of ischemic heart disease in treated hypertension subjects was higher than among normotensive or untreated subjects.
As shown in Table 1, the parameters related to pulse pressure, i.e. distensibility, elastic modulus, and stiffness index, were significantly more affected among females than among males, even though baPWV was not significantly different between genders. Parameters for proximal AA stiffness were different among the normotensive, untreated hypertensive, and treated hypertensive groups. They were worst among untreated hypertensive subjects (Table 2).
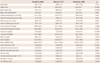
In a simple correlation analyses, the Pearson correlation coefficients for the relationship between baPWV and age, SBP, pulse pressure, heart rate, fasting blood glucose, total cholesterol, and creatinine were significantly positive (Table 3). The parameters of proximal AA stiffness were significantly correlated with baPWV in both normotensive and hypertensive subjects (Fig. 2).
In partial correlation analyses, after adjustments for age, gender, SBP, BMI, and heart rate, baPWV was consistently significantly correlated with strain, elastic modulus, and stiffness index in all subjects and in normotensive subjects (Table 4). When additionally adjusted for antihypertensive medication status, there was no significant correlation between baPWV and the stiffness parameters for the proximal AA.
In the multiple regression analyses, baPWV was independently associated with the strain of the proximal AA or strain only among normotensive subjects, as shown in Table 5. Not antihypertensive medication status itself, but the level of blood pressure and heart rate, was associated with baPWV in the multiple linear regression model, including abdominal aortic strain.
After adjustments for age, gender, BMI, SBP, and heart rate, baPWV was significantly higher among the lower quartiles of distensibility in the normotensive group (Q1, 1539±36 cm/sec; Q2, 1426±32 cm/sec; Q3, 1406±32 cm/sec; Q4, 1425±35 cm/sec, p for linear trend=0.0419). The baPWV among normotensive subjects was significantly higher with increasing quartiles of elastic modulus (Q1, 1428±35 cm/sec; Q2, 1404±31 cm/sec; Q3, 1426±32 cm/sec; Q4, 1539±36 cm/sec, p for linear trend=0.0489) (Fig. 3A). For the hypertensive group, with additional adjustments for antihypertensive medication status, baPWV was not significantly different among the quartile groups (Fig. 3B).
The main finding of this study is that baPWV has a moderate crude correlation with the stiffness parameters for proximal AA. However, when adjusted for age, sex, SBP, heart rate, and BMI, such correlations were observed only among normotensive subjects. The antihypertensive medication status does not appear to be associated with baPWV in the multiple linear regression model, including abdominal aortic strain. Such a finding suggests that, in hypertensive subjects, not antihypertensive medication itself, but other factors, (such as age, SBP, and heart rate), may be more involved in the relationship between baPWV and proximal AA strain than for normotensive subjects. The relationship between baPWV and proximal AA stiffness parameters seemed to be linear only in the normotensive group. The lack of any significant association between baPWV and proximal AA stiffness parameters in the hypertension group may be due to the effect of antihypertensive medication on blood pressure and heart rate. The role of the different classes of antihypertensive medication could not be demonstrated in the present study.
Similar results were observed in a previous study, which showed that baPWV might have some limitations in predicting arterial stiffness in hypertensive patients with a history of cardiovascular disease.23) However, some authors suggest that baPWV can predict early arteriosclerotic changes.24) In addition, compared to the augmentation index, baPWV is reported to be useful among elderly patients, and some studies have shown that baPWV can predict aortic calcification.4)25)
The non-significant correlations between baPWV and proximal AA stiffness in the hypertensive group, regardless of antihypertensive medication status, can be explained by findings from previous studies. The stiffness parameters of the proximal AA do not have a linear relationship with age; a plateau can be observed in old age.26)27) It was reported that aortic distensibility and elastic modulus are more useful indicators in normal young subjects than among hypertensive and elderly subjects.28) baPWV was reported to underestimate aortic stiffness in hypertensive patients with coronary artery disease or target organ damage, as these subjects have lower femoral-ankle PWV.23)
In this study, we unexpectedly found that the stiffness parameters of the proximal AA were more affected in female subjects (Table 1 and 5). The higher pulse pressure in females is likely to be the reason for those differences. It is known that pulse pressure tends to be higher in females than males after the age of 50.29) In addition, we found that diastolic aortic dimensions were significantly lower among female subjects, which is consistent with a previous study suggesting that aortic arch diameter in the diastole was lower in females than in males (2.56±0.31 mm vs. 2.88±0.35 mm).30) Although the smaller aortic size could not explain the pulse pressure difference completely, these differences between genders point to some gender-related differences in mechanical properties in response to aortic pressure changes, or a gender-related mismatch between ventricular function and aortic function.30) Furthermore, females had higher total cholesterol and LDL, consistent with a previous study performed in the general population and one of patients with familial hypercholesterolemia.16)31) Finally, there may be a difference in left ventricular function, which may affect proximal AA distensibility, as found in a previous study.32)
Ultrasonography is a readily accessible clinical tool for examining proximal AA when combined with an examination of the heart or intra-abdominal organs. The worst quartiles of proximal AA stiffness in normotensive subjects had greatly increased baPWV values. The application of a conventional ultrasound examination of the proximal AA may be helpful in identifying normotensive subjects with arterial stiffness, but its potential application for hypertensive subjects is not supported by the findings of the present study. However, the proportion of subjects with ischemic heart disease history was about a quarter in the treated hypertension group, because, in our study, the subjects were recruited from a hypertension clinic affiliated with a cardiology division. Consequently, any generalized application of the negative findings among hypertensive subjects may be limited.
There are some limitations of this study. Firstly, all subjects were examined after fasting. Thus, the usefulness of measuring proximal AA stiffness in fed subjects was not demonstrated. Additionally, cfPWV, which is more accurate than baPWV, was not used in this study because, during preliminary testing, baPWV was found to be superior in terms of both technical feasibility and general use in actual clinical practice. Using a VP-2000 device, hfPWV would be a far more accurate indicator of aortic stiffness than baPWV if a femoral artery probe can be applied. The correlation between PWV and abdominal aortic strain would have been improved had cfPWV been adopted. The result cannot be applied to cfPWV. The results of the study demonstrating the effects of antihypertensive medication on aortic strain in the multiple regression analysis should be interpreted with caution, because each of the classes of antihypertensive drugs were not considered. In the present study, the sample size was too small to examine the effects of antihypertensive drug classes in the treated subjects. Further studies are warranted in this area of investigation.
Figures and Tables
Fig. 1
Measurement of abdominal aortic strain. A sector probe was placed at the epigastrium targeting the spine, which typically shows a prominent anterior wall excursion and a relatively fixed posterior wall. *Abdominal aorta abutting spine posteriorly. AAoD: minimal diastolic abdominal aortic dimension at the onset of the QRS wave, AAoS: maximal systolic abdominal aortic dimension.

Fig. 2
Scatter plots for the correlation between proximal abdominal aortic strain and mean brachial-ankle pulse wave velocity according to hypertension status. The correlation was higher in normotensive subjects than in hypertensive subjects.

Fig. 3
baPWV according to the quartiles of the stiffness parameters of the proximal AA. A: least square means adjusted for age, gender, systolic blood pressure, heart rate, and body mass index according to the quartile groups of the stiffness parameters of the proximal AA in normotensive subjects. B: least square means additionally adjusted for antihypertensive medication status, according to the quartile groups of the stiffness parameters of the proximal AA in hypertensive subjects. There was no difference observed in baPWV between the quartiles of the stiffness parameters of the proximal AA in the hypertensive group. baPWV: brachial-ankle pulse wave velocity, AA: abdominal aorta.

Table 3
Pearson correlation coefficients for the relationships between mean baPWV and proximal AA stiffness parameter
References
1. Laurent S, Boutouyrie P, Asmar R, et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001; 37:1236–1241.
2. Kolipaka A, Woodrum D, Araoz PA, Ehman RL. MR elastography of the in vivo abdominal aorta: a feasibility study for comparing aortic stiffness between hypertensives and normotensives. J Magn Reson Imaging. 2012; 35:582–586.
3. Kim MJ, Lee SY, Kim YB, Kil HR. Click here to read click here to read clinical significance of the mechanical properties of the abdominal aorta in Kawasaki disease. Korean J Pediatr. 2008; 51:1012–1017.
4. Nakamura U, Iwase M, Nohara S, Kanai H, Ichikawa K, Iida M. Usefulness of brachial-ankle pulse wave velocity measurement: correlation with abdominal aortic calcification. Hypertens Res. 2003; 26:163–167.
5. Okubo M, Ino T, Takahashi K, Kishiro M, Akimoto K, Yamashiro Y. Age dependency of stiffness of the abdominal aorta and the mechanical properties of the aorta in Kawasaki disease in children. Pediatr Cardiol. 2001; 22:198–203.
6. Haskett D, Johnson G, Zhou A, Utzinger U, Vande Geest J. Microstructural and biomechanical alterations of the human aorta as a function of age and location. Biomech Model Mechanobiol. 2010; 9:725–736.
7. Ahlgren AR, Hansen F, Sonesson B, Länne T. Stiffness and diameter of the common carotid artery and abdominal aorta in women. Ultrasound Med Biol. 1997; 23:983–988.
8. Seo JS, Lee SY, Kim HD. Quantitative analysis of aortic atherosclerosis in Korean female: a necropsy study. J Korean Med Sci. 2007; 22:536–545.
9. Zakai NA, Katz R, Jenny NS, et al. Inflammation and hemostasis biomarkers and cardiovascular risk in the elderly: the Cardiovascular Health Study. J Thromb Haemost. 2007; 5:1128–1135.
10. Kaibe M, Ohishi M, Komai N, et al. Arterial stiffness index: a new evaluation for arterial stiffness in elderly patients with essential hypertension. Geriatr Gerontol Int. 2002; 2:199–205.
11. Giannattasio C, Capra A, Facchetti R, et al. Relationship between arterial distensibility and coronary atherosclerosis in angina patients. J Hypertens. 2007; 25:593–598.
12. Gur M, Yilmaz R, Demirbag R, et al. Relationship between myocardial performance index and aortic distensibility in patients with essential hypertension. Int J Clin Pract. 2008; 62:138–142.
13. Dernellis J, Panaretou M. Aortic stiffness is an independent predictor of progression to hypertension in nonhypertensive subjects. Hypertension. 2005; 45:426–431.
14. Gosling RG, Budge MM. Terminology for describing the elastic behavior of arteries. Hypertension. 2003; 41:1180–1182.
15. Kawasaki T, Sasayama S, Yagi S, Asakawa T, Hirai T. Non-invasive assessment of the age related changes in stiffness of major branches of the human arteries. Cardiovasc Res. 1987; 21:678–687.
16. Pitsavos C, Toutouzas K, Dernellis J, et al. Aortic stiffness in young patients with heterozygous familial hypercholesterolemia. Am Heart J. 1998; 135:604–608.
17. Stefanadis C, Stratos C, Boudoulas H, Kourouklis C, Toutouzas P. Distensibility of the ascending aorta: comparison of invasive and noninvasive techniques in healthy men and in men with coronary artery disease. Eur Heart J. 1990; 11:990–996.
18. Pannier BM, Avolio AP, Hoeks A, Mancia G, Takazawa K. Methods and devices for measuring arterial compliance in humans. Am J Hypertens. 2002; 15:743–753.
19. Shin J, Lee J, Lim HK, Lee BH, Kim MK, Choi BY. The relationship between the pulse wave velocity (PWV) and the left ventricular geometry: a Community-Based Cross-Sectional Study. Korean Circ J. 2005; 35:683–689.
20. Erdogan D, Gullu H, Caliskan M, et al. The influence of circadian blood pressure changes on aortic distensibility and left ventricular diastolic function in hypertensive individuals. Int J Cardiovasc Imaging. 2006; 22:157–165.
21. Lee YS, Kim KS, Hyun DW, et al. The change of arterial stiffness according to dialysis in patients with end-stage renal disease. Korean Circ J. 2004; 34:865–873.
22. Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009; 41:1149–1160.
23. Ito N, Ohishi M, Takagi T, et al. Clinical usefulness and limitations of brachial-ankle pulse wave velocity in the evaluation of cardiovascular complications in hypertensive patients. Hypertens Res. 2006; 29:989–995.
24. Hung CS, Lin JW, Hsu CN, et al. Using brachial-ankle pulse wave velocity to associate arterial stiffness with cardiovascular risks. Nutr Metab Cardiovasc Dis. 2009; 19:241–246.
25. Li B, Gao H, Li X, Liu Y, Wang M. Correlation between brachial-ankle pulse wave velocity and arterial compliance and cardiovascular risk factors in elderly patients with arteriosclerosis. Hypertens Res. 2006; 29:309–314.
26. Redheuil A, Yu WC, Wu CO, et al. Reduced ascending aortic strain and distensibility: earliest manifestations of vascular aging in humans. Hypertension. 2010; 55:319–326.
27. Tsamis A, Rachev A, Stergiopulos N. A constituent-based model of age-related changes in conduit arteries. Am J Physiol Heart Circ Physiol. 2011; 301:H1286–H1301.
28. Lehmann ED, Gosling RG, Parker JR, deSilva T, Taylor MG. A blood pressure independent index of aortic distensibility. Br J Radiol. 1993; 66:126–131.
29. Regnault V, Thomas F, Safar ME, et al. Sex difference in cardiovascular risk: role of pulse pressure amplification. J Am Coll Cardiol. 2012; 59:1771–1777.
30. Dart AM, Kingwell BA, Gatzka CD, et al. Smaller aortic dimensions do not fully account for the greater pulse pressure in elderly female hypertensives. Hypertension. 2008; 51:1129–1134.
31. Mokhtari A, Bellinetto-Ford L, Melander O, Nilsson PM. Determinants of increasing pulse pressure during 23 years' follow-up as a marker of arterial stiffness and vascular ageing. Blood Press. 2008; 17:291–297.
32. Giannattasio C, Achilli F, Failla M, et al. Radial, carotid and aortic distensibility in congestive heart failure: effects of high-dose angiotensin-converting enzyme inhibitor or low-dose association with angiotensin type 1 receptor blockade. J Am Coll Cardiol. 2002; 39:1275–1282.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download