Abstract
Background and Objectives
Dobutamine stress echocardiography (DSE) is an important non-invasive imaging method for evaluating ischemia. However, wall motion interpretation can be impaired by the experience level of the interpreter and the subjectivity of the visual assessment. In our study we aimed to combine DSE and tissue syncronisation imaging to increase sensitivity for detecting ischemia.
Subjects and Methods
50 patients with indications for DSE were included in the study. In 25 patients we found DSE positive for ischemia and in the other 25 patients we found it to be negative. The negative group was accepted as the control group. There was no significant difference in terms of risk factors and echocardiographic parameters between the two groups, except for wall motion scores. In both groups, left ventricular dyssychrony was accepted as the difference between time to peak systolic velocity (Ts) in the reciprocal four couple of non-apical segments at rest and during peak stress. Timings were corrected for heart rate. We compared the differences of the dyssynchronisation value at rest and during peak stress to determine the distinctions within the groups and between the groups of DSE positive and negative patients.
Results
We found that stress and ischemia did not create any significant difference over the left intraventricular dyssynchrony with DSE, although at the segmenter level it prolonged the time to peak systolic velocity (p<0.05). These alterations did not show any significant difference between positive and negative DSE groups.
Ischemic heart diseases are among the more prominent cause of death in the community. In these diseases, early diagnosis protects the patient from death and permanent disability. Dobutamine stress echocardiography (DSE) is one of the most reliable techniques for detecting ischemic heart diseases.1) Cardiac stress echocardiography does not provide knowledge about how much obstruction is present in the coronary vessels at the anatomic level. However, it provides knowledge about the physiological importance of the obstruction in the coronary lumen. This technique, in particular, can be used for patients who cannot tolerate an exercise test, while at the same time it is important for evaluating myocardial viability, hibernation, valvular heart diseases, and, in selected patients, can be utilized prior to non-cardiac surgery.2) When used for detecting ischemia, the most important limitation of this technique's effectiveness depends on the physician and image quality of the patient.1) Wide studies reported that the technique has an accuracy of 80-85% compared with other techniques. False negative results may be connected with inadequate stress and heart rates. False positive results can arise from true ischemia without angiographycally significant lesions, variations of normal wall movements, and regional changes of endocardial thickening.3) In the presence of coronary arterial occlusion, dobutamine increases myocardial volume oxygen consumption. This condition causes myocardial ischemia with a mismatch of presentation consumption.4) Numerous studies have revealed the relationship between myocardial synchrony and the clinical symptoms of heart failure.5) Asynchronous motion can be clearly traceable in coronary arterial disease between left ventricular (LV) segments. Previous studies stated that TSI could be used in ischemic and infarcted coronary arterial disease for determining regional myocardial disease.5)6) Tissue Synchronisation Imaging is dependent on tissue Doppler imaging, which can automatically measure time to peak velocity (Ts) and peak velocity (Vp); encoded myocard with different colours, and placed tissue synchronisation images on the tissue images. In the early phase of the contraction of normal myocardium, which can manage the peak velocity encoded with green colour, there was no delay in movement (Ts 20-150 msec). Delayed contracted myocardium is encoded with yellow or red colour, according to the degree of the delay, to maintain peak velocity. A moderate delay can be seen as yellow (Ts 150-300 msec); a severe delay can be seen as red (Ts 300-500 msec).5) In this study, we investigated the extent and importance of LV dyssynchrony when the ventricle was exposed to dobutamine stress. We also aimed to increase the clinical utility of DSE by evaluating normal and abnormal synchronisation with Tissue Synchronisation Imaging and determining if there is any change in the synchronization of myocardial segments with ischemia.
This study was undertaken at the Atatürk University Faculty of Medicine, Department of Cardiology. Inclusion criteria were admitting to our policlinic with chest pain and those not suitable for exercise testing because of orthopaedic problems, arthritis, peripheral arterial disease with claudication, or prior stroke and obstructive pulmonary disease. Exclusion criteria were acute coronary syndromes, decompensated heart failure, uncontrolled ventricular or supraventricular tachyarrhythmias, uncontrolled hypertension, hypertrophic obstructive cardiomyopathy, severe aortic stenosis, and QRS duration more than 120 ms. The study population consisted of 50 patients (26 men, 24 women). The control group consisted of these 50 patients, 25 of whose DSE results were negative. Written informed consent was obtained from all participants before DSE was performed. The study conformed to the principles of the Declaration of Helsinki and was approved by the Atatürk University Faculty of Medicine Ethics Committee. All patients were monitored for two hours in the coronary intensive care unit after the test was concluded.
Transthoracic echocardiographic examination including DSE (Figs.1 and 2) was performed with a commercially available ultrasound system (Vivid 7, GE Healthcare) equipped with a 2.5-MHz transducer. All data was stored at three cardiac cycles at rest and at peak stress digitally, and analysed off-line by two cardiologists. β blocker drugs were ceased 48 hours prior to testing. Dobutamine was given intravenously at three-minute periods with increased doses at 5, 10, 20, 30, 40 mcgr/kg/minute. Among our patients, we achieved a target heart rate and positive DSE criteria without atropine. Electro-cardiography and blood pressure were monitored using non-invasive methods. The test terminated when the target heart rate was reached, in the event of new or worsened wall motion abnormality, new continuously arrhythmia, increases and persistence of systolic blood pressure over 200 mm Hg, seeing ST-segment depression or elevation, or in the event of chest pain or dyspnea. New or worsened wall motion abnormality in at least two segments was accepted as positive criteria for DSE.3) Scoring wall motion abnormalities was performed in accordance with the American Society of Echocardiography Committee recommendations: 1) normal; 2) hypokinesia; 3) akinesia; 4) dyskinesia.7) In tissue Doppler imaging mode a cursor was placed to the lateral, septal, anterior and inferior walls' basal and mid points at apical four chamber and apical two chamber images for obtaining myocardial velocity graphics. Apical segments of the heart were not encoded with colour using the TSI method, so we did not analyse these segments. Systol was accepted as 200 ms after the start of QRS complex. The time from the beginning of QRS complex to peak systolic velocity was measured from 8 segments at rest and at peak stress. Measurements were corrected for heart rate using the Bazett Formula (Tscor=Ts/√R-R).2) The absolute value of the difference between opposite segments' Tscor values (inferior and anterior, lateral and septal) was accepted as intraventricular dyssynchrony.8) Intraventricular dyssynchrony was measured separately at rest and peak stress. We made intragroup and intergroup comparisons with differences of dyssynchrony values at rest and peak stress.
Data was entered and analysed using the Statistical Package for the Social Sciences (SPSS) statistical software version 10.0 (SPSS Inc., Chicago, IL, USA). The Wilcoxon signed rank test was used to determine the intragroup differences and the Mann-Whitney U test was used to determine the intergroup differences for continuous variables. The Pearson chi-square test was used to determine the difference between discontinuous variables. p<0.05 was accepted as significant.
Fifty potentially suitable patients were included for study. A total of 25 patients' DSE tests were determined as positive. The other 25 patients' tests were negative and those patients were specified as the control group. All patients were in sinus rhythm and had no segmental wall motion abnormality. DSE positive patients under-went coronary angiography, and we founded left anterior descending lesions in 4 (16%) patients, circumflex lesions in 11 (44%) patients and right coronary artery lesions in 8 (32%) patients. Lesions were considered to have a diameter stenosis of ≥50%. In two (8%) patients, coronary angiography readings were normal. The distribution of age, sex, height, weight, LV systolic and diastolic diameters, left atrium diameter, ejection fraction (using the Modified Simpson method), diabetes mellitus, hypertension, smoking rates, coronary arterial disease and family history is shown in Table 1 and 2. The distribution of these characteristics was similar across groups. As expected, heart rate was higher in the control group than in the DSE positive group because of positivity being detected at a lower heart rate. Again, as expected, the peak stress wall motion score was found to be significantly higher in the DSE positive group than in the control group. Ts was measured in 120/120 segments at rest and peak stress in the two groups. Corrections were made using the Bazett formula. In Table 3, the mean values of measured segments Ts values and standard deviations are shown. In the control group, we could not find any significant difference in Tscor values between segments at rest and peak stress. Conversely, there was a significant difference in the DSE positive patient group in the Tscor values of all segments at rest and peak stress (Table 4). There was no significant difference in the terms of intraventricular dyssynchrony between mutual segments of the DSE positive and negative groups at rest and peak stress. However, in the DSE positive group, we found a difference quite close to the significance level at the mid-inferior segment (ischemia detected more often than the other segments) and mid-anterior segment (compared segment of the mid-inferior segment) (Table 5). When we compared the two groups' dyssynchrony values at rest and peak stress, we did not find any significant difference (Table 6).
Delayed contraction of myocardium, decreased contraction power, and dyssynchronous motion is characterised by reduced systolic function. Myocardial contraction depends on energy. In myocardial ischemia, energy supply decreases and systolic dysfunction occurs. Analysing local myocardial contraction characteristics, illuminating systolic vitodynamics and the physiological mechanisms of myocardium play important roles in the diagnosis of ischemia and infarct. Tissue Doppler imaging, strain rate imaging, and tissue synchronisation imaging can be used for determining local myocardial conduction and systolic function.5)9) Gorcsan et al.10) first used TSI for determining myocardial dyssynchrony before and after cardiac pacemaker implantation. They found a sensitivity of 87% and specificity of 100% for determining myocardial dyssynchrony, reporting that TSI is a simple and usable method for the quantitative determination of regional myocardial dyssynchrony. However, with the exception of a few studies, TSI was not used for detecting ischemia and determining regional motion abnormality through the result of hypoxia. In our study, we aimed to develope the usage of this technique in clinical life.
Dobutamine stress echocardiography allows for the detection of ischemia by a non-invasive method in patients who are older, whose exercise capacity has decreased and for whom participating in an exercise test is difficult or impossible. Exercise allows patients to reach higher heart rates but decreases the heart rate much faster. Imaging problems result at a higher rate than for DSE.11) We used DSE with the intention of obtaining much better exposure of ischemia dyssynchrony.
We found that the stress induced by DSE did not make a significant difference in intraventricular dyssynchrony, but prolonged the elapsed time to reach peak systolic velocity at the segmental level. There was no significant difference due to these changes in the DSE positive and negative groups. Therefore, no new value was caused by DSE for detecting inducible ischemia when segmental dyssynchrony and time to peak systole were corrected for heart rate. There are conflicting results relating to the effects of stress at dyssynchrony in the studies performed by stimulated tachycardia. Lafitte et al.12) reported in patients with normal LV function that exercise did not modify the extent of LV asynchrony. In contrast, in heart failure patients, LV dyssynchrony increased by at least 20% in 34% of them, remained stable in 37%, and decreased by at least 20% in 29%. Furthermore, 26% of heart failure patients had either exercise induction or normalisation of ventricular dyssynchrony. Valzania et al.13) studied CRT implanted patients whose QRS duration was over 130 ms. At rest, CRT withdrawal was associated with an increased interventricular mechanical delay and impaired intraventricular synchrony. They reported that dobutamine infusion had no impact on interand intraventricular synchrony. During stress, there was an improvement in LV performance both at the "on" and "off" positions. However, LV dp/dt, aortic VTI, cardiac output, mean systolic peak velocities, and LV filling time during dobutamine stress were significantly greater with CRT "on". Although they analysed peak systolic velocity times without correcting for heart rate, Kang et al.14) investigated the impact of exercise induced changes in intraventricular dyssynchrony in patients with nonischemic cardiomyopathy. They found no significant difference in intraventricular dyssynchrony with exercise, but indicated that dyssynchrony value could change with exercise. These studies support our findings. We found that there was no significant difference in intraventricular dyssynchrony in DSE positive and negative groups, although in the two groups intraventricular dyssynchrony increased at two segments and did not change in two segments with stress. Again in our study we showed that dyssynchrony was dynamic in the majority of patients and that it can be changed by DSE. These dynamic changes significantly increase the time to peak systolic velocity with heart rate. These conditions show that intrasegmental dyssynchrony can be induced by DSE in patients who have no dyssynchrony at rest. De Sutter et al.15) reported from the Belgian Multicentre Registry on dyssynchrony that the prevalence of inter- and intraventricular dyssynchrony was low (17% and 18%, respectively) in patients with heart failure and preserved left ventricular ejection fraction (LVEF). However, in the presence of a QRS width of ≥120 ms, this prevalence increased to almost 50%, comparable to that for patients with heart failure and reduced LVEF and a QRS width of ≥120 ms. Hummel et al.16) revealed that stress effects occur especially among patients with heart failure and whose QRS width was over 120 ms. Da Costa et al.17) asserted that the effect of stress on dyssynchrony depends on whether QRS width is over or under 120 ms., heart rate, the agent of the stress, and the variety of dyssynchrony definition. They presumed that this was the reason for the variable results from different studies. In our study, we selected patients with a QRS width under 120 ms. Again, in our study, we payed additional attention to the general characteristics of patients with no difference between the two groups.
We aimed to combine the TSI method, which uses wall motions' quantitatively time parameters for detecting myocardial conduction and contraction functions, and DSE in probable coronary heart disease patients. However, as we mentioned earlier, the tissue synchronysation imaging technique, when combined with DSE, does not provide any quantitative benefit for detecting ischemia. There is a pressing need for further studies in combining TSI and DSE.
Although the study sample was small, it was formed for the homogeneous patient population, and, because of ethical reasons, we did not correct negative DSE with angiographic methods. The TSI method does not detect apical segments of the heart, so we did not study patients with apical wall motion abnormalities. The other limitations of this study were the image quality changes from patient to patient. Peak systolic velocity time is impacted by the Doppler angle, so we used a Doppler angle under 15 degrees, decreasing the angle effect on the results.
Figures and Tables
 | Fig. 1Tissue synchronisation imaging and measurements of intraventricular dyssynchrony at 2 chamber and 4 chamber images. |
Table 1
General characteristics of dobutamine stress echocardiography positive and negative patients

LVDD: left ventricular diastolic diameter, LVSD: left ventricular systolic diameter, IVS: interventricular septum thickness, PW: posterior wall thikness, LVEF: left ventricular ejection fraction (Modified Simpson method), LA: left atrium diameter, NS: not significant, DSE: dobutamine stress echocardiography, LAD: left anterior descending, LCx: left circumflex, RCA: right coronary artery
Table 2
General characteristics of dobutamine stress echocardiography positive and negative patients
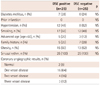
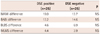
Table 4
Corrected time to peak velocity (ms) values at dobutamine stress echocardiography positive group

References
1. Marwick TH. Stress echocardiography. Heart. 2003; 89:113–118.
2. Gottdiener JS. Overview of stress echocardiography: uses, advantages, and limitations. Curr Probl Cardiol. 2003; 28:485–516.
3. Picano E. Stress Echocardiography. 4th ed. Heidelberg, Germany: Springer-Verlag;2003.
4. Corday E, Hajduczki I, O'Byrne GT, Kar S, Areeda J, Corday SR. Echocardiographic criteria to distinguish reversible from irreversible myocardial ischaemia. Eur Heart J. 1988; 9:Suppl F. 29–43.
5. Tian JW, Du GQ, Ren M, Sun LT, Leng XP, Su YX. Tissue synchronization imaging of myocardial dyssynchronicity of the left ventricle in patients with coronary artery disease. J Ultrasound Med. 2007; 26:893–897.
6. Kyriakides ZS, Manolis AG, Kolettis TM. The effects of ventricular asynchrony on myocardial perfusion. Int J Cardiol. 2007; 119:3–9.
7. Schiller NB, Shah PM, Crawford M, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr. 1989; 2:358–367.
8. Dohi K, Pinsky MR, Suffoletto MS, Severyn DA, Gorcsan J III. A new rapid and simple index of mechanical dyssynchrony by colour-coded strain dyssynchrony imaging. J Am Coll Cardiol. 2005; 45:A289.
9. Sade LE, Gorcsan J 3rd, Severyn DA, Edelman K, Katz WE. Usefulness of angle corrected tissue Doppler to assess segmental left ventricular function during dobutamine stress echocardiography in patients with and without coronary artery disease. Am J Cardiol. 2005; 96:141–147.
10. Gorcsan J 3rd, Kanzaki H, Bazaz R, Dohi K, Schwartzman D. Usefulness of echocardiographic tissue synchronization imaging to predict acute response to cardiac resynchronization therapy. Am J Cardiol. 2004; 93:1178–1181.
11. Leier CV, Unverferth DV. Drugs five years later. Dobutamine. Ann Intern Med. 1983; 99:490–496.
12. Lafitte S, Bordachar P, Lafitte M, et al. Dynamic ventricular dyssynchrony: an exercise-echocardiography study. J Am Coll Cardiol. 2006; 47:2253–2259.
13. Valzania C, Gadler F, Eriksson MJ, Olsson A, Boriani G, Braunschweig F. Electromechanical effects of cardiac resynchronization therapy during rest and stress in patients with heart failure. Eur J Heart Fail. 2007; 9:644–650.
14. Kang SJ, Lim HS, Choi BJ, et al. The impact of exercise-induced changes in intraventricular dyssynchrony on functional improvement in patients with nonischemic cardiomyopathy. J Am Soc Echocardiogr. 2008; 21:948–953.
15. De Sutter J, Van de Veire NR, Muyldermans L, et al. Prevalence of mechanical dyssynchrony in patients with heart failure and preserved left ventricular function (a report from the Belgian Multicenter Registry on dyssynchrony). Am J Cardiol. 2005; 96:1543–1548.
16. Hummel JP, Lindner JR, Belcik JT, et al. Extent of myocardial viability predicts response to biventricular pacing in ischemic cardiomyopathy. Heart Rhythm. 2005; 2:1211–1217.
17. Da Costa A, Thévenin J, Roche F, et al. Prospective validation of stress echocardiography as an identifier of cardiac resynchronization therapy responders. Heart Rhythm. 2006; 3:406–413.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download