This article has been corrected. See "Erratum: Etiologies and Predictors of False-Positive Diagnosis of ST-Segment Elevation Myocardial Infarction" in Volume 43 on page 580.
Abstract
Background and Objectives
Rapid diagnosis of ST-segment elevation myocardial infarction (STEMI) is essential for the appropriate management of patients. We investigated the prevalence, etiologies and predictors of false-positive diagnosis of STEMI and subsequent inappropriate catheterization laboratory activation in patients with presumptive diagnosis of STEMI.
Subjects and Methods
Four hundred fifty-five consecutive patients (62±13 years, 345 males) with presumptive diagnosis of STEMI between August 2008 and November 2010 were included.
Results
A false-positive diagnosis of STEMI was made in 34 patients (7.5%) with no indication of coronary artery lesion. Common causes for the false-positive diagnosis were coronary spasm in 10 patients, left ventricular hypertrophy in 5 patients, myocarditis in 4 patients, early repolarization in 3 patients, and previous myocardial infarction and stress-induced cardiomyopathy in 2 patients each. In multivariate logistic regression analysis, symptom-to-door time >12 hours {odds ratio (OR) 4.995, 95% confidence interval (CI) 1.384-18.030, p=0.014}, presenting symptom other than chest pain (OR 7.709, 95% CI 1.255-39.922, p=0.027), absence of Q wave (OR 9.082, CI 2.631-31.351, p<0.001) and absence of reciprocal changes on electrocardiography (ECG) (OR 17.987, CI 5.295-61.106, p<0.001) were independent predictors of false-positive diagnosis of STEMI.
Conclusion
In patients whom STEMI was planned for primary coronary intervention, the false-positive diagnosis of STEMI was not rare. Correct interpretation of ECGs and consideration of ST-segment elevation in conditions other than STEMI may reduce inappropriate catheterization laboratory activation.
The time-to-reperfusion in the setting of ST-segment elevation myocardial infarction (STEMI) is an important predictor of clinical events and outcomes.1)2) Therefore, rapid diagnosis of STEMI is essential for an appropriate management of patients.3)4) However, the decision to provide immediate reperfusion therapy to patients presenting with chest pain and ST-segment elevation may not be simple since STEMI is not the only cause of ST-segment elevation on electrocardiography (ECG).5-16) False-positive catheterization laboratory activation is a significant concern because of procedural risks to the patient and burdens on financial resources.17) Although limited data is available on the prevalence of false-positive catheterization laboratory activation in patients undergoing percutaneous coronary intervention (PCI) for suspected STEMI,17)18) we predicted that the causes of false-positive catheterization activation may differ in Korea compared with the reports from Western countries.17)18) The objective of the present was to determine the prevalence, etiologies and predictors of false-positive diagnosis of STEMI and subsequent inappropriate catheterization laboratory activation in patients with presumptive diagnosis of STEMI.
Four hundred fifty-five consecutive patients with presumptive diagnosis of STEMI who underwent emergency coronary angiography for primary PCI at Kyungpook National University Hospital, Daegu, Korea between August 2008 and November 2010 were included. All patients except one (n=454, 99.8%) were ethnic Korean and presented within the first 12 hours after symptom onset with ST-segment elevation or new left bundle branch block (LBBB) on ECG were considered eligible for primary PCI. Patients with symptom onset >12 hours were also included if they were symptomatic on arrival. The decision to activate the catheterization laboratory for primary PCI was made by the physician in the Department of Internal Medicine and communicated by face-to-face notification during on-duty hours and by the emergency physician via a phone call to the on-call interventional cardiologist during off-duty hours, who would in turn activate the entire staff involved in primary PCI.
ST-segment elevation was defined as J-point elevations in ≥2 leads, with a cutoff of ≥0.2 mV in leads V 1, V 2, or V 3 and ≥0.1 mV in other leads. In patients with LBBB, ST-segment elevation was defined as ST-segment elevation ≥0.5 mV and discordant with QRS complex.19) ST-segment elevation was assessed relative to the RR segment. ST-segment depression in the following leads was identified as reciprocal ST-segment change: leads I, aVL in inferior STEMI, leads II, III, aVF in anterior STEMI and III, aVF in lateral STEMI.20) All ECGs were reviewed by Y Cho and MH Bae at our hospital. Each 12-lead ECG was separately reviewed for the presence or absence of ST-segment elevation, Q wave, reciprocal changes, left ventricular hypertrophy (LVH), LBBB and right bundle branch block (RBBB). The height of maximal ST-segment elevation and the number of leads with ST-segment elevation were also recorded. The cardiac troponin I (cTnI) levels were measured on admission and every 6 hours after to detect the presence of myocardial injury using an enzyme immunoassay based on the sandwich principle kit (Dimension; Dade Behring, USA); the lower detection limit of this assay was 0.04 ng/mL. Elevated cardiac biomarker levels were defined as maximal values of cTnI that exceeded the decision limit (99th percentile of the values for a reference control group) on at least one occasion. A culprit coronary lesion was identified if a coronary lesion corresponding to the electrocardiographic changes was found. False-positive catheterization laboratory activation for STEMI was defined as the absence of a culprit coronary artery in patients who underwent emergency coronary angiography for planned primary PCI. Myocarditis was defined by flu-like signs and symptoms, typical ECG findings of pericarditis, elevations of cTnI levels and normal coronary artery by angiography.21) A final diagnosis of stress-induced cardiomyopathy was based on characteristic 2-dimensional (D) echocardiographic wall motion abnormalities in the mid and distal left ventricle and associated psychological stress preceding the cardiac event.22) Coronary spasm was defined if culprit spastic vessel was relieved by intracoronary nitroglycerin injection or if the result of a ergonovine test was positive; total or near total occlusion of culprit vessel with concurrent chest pain and/or ST-segment elevation.23) LVH was based on the definitions of Sokolow and Lyon.24) Previous myocardial infarction (MI) with persistent ST-segment elevation was defined by history of a Q-wave MI with ST-segment elevation that was either demonstrated on a previous ECG or did not demonstrate ST-segment evolutionary changes.17) Early repolarization was identified in patients with negative cTnI results and the following ECG findings: elevated concave ST-segment, located commonly in the precordial leads (most conspicuous in leads V 1-3), tall peaked T waves, a slur on the R wave.5)6) Clinical, laboratory, 2-D echocardiographic, angiographic, and outcome data for all patients who had the diagnosis of presumptive STEMI were collected. Two-D echocardiography was performed within 24 hours after arrival in most cases.
Data are presented as mean±standard deviation for continuous variables and percentages for categorical variables. Patients were categorized into a STEMI group and a false-positive STEMI group. Comparisons were made using the Student's t-test for continuous variables and the chi-square test for categorical variables. The p were 2-sided, and p<0.05 was considered significant. Multiple logistic regression analysis was used to determine independent predictors of false-positive catheterization laboratory activation for STEMI, and adjusted for baseline confounding characteristics with p<0.05 in univariate analysis. Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS)® version 15.0 for Windows® (SPSS Inc., Chicago, IL, USA).
Four hundred fifty-five consecutive patients who underwent emergency coronary angiography for primary PCI with presumptive diagnosis of STEMI were enrolled in this study. Four hundred twenty-one patients (92.5%) had identifiable culprit lesion(s) in coronary arteries responsible for the presumptive diagnosis of STEMI, and classified as true-positive for catheterization laboratory activation in those patients. The frequencies of anterior and inferior STEMI were 45.3% and 40.8%, respectively. Thirty-four patients (7.5%) had either normal coronary arteries or significant coronary lesions which were not responsible for the suspected STEMI leading to the classification of false-positive for catheterization laboratory activation and cardiac biomarker results were negative in 18 patients.
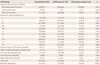
The baseline patient characteristics are shown in Table 1. The mean age was 62±13 years and 345 patients (75.8%) were men. There was a higher proportion of dyslipidemia (p=0.006) in the STEMI group. The false-positive group had a significantly longer symptomto-door time (p=0.048) and significantly higher proportion of symptom-to-door time >12 hours (p=0.015) compared with the STEMI group. Two hundred eighty-three patients (62.2%) were referred from regional medical centers with no primary PCI capability, and presentation to a district hospital without primary PCI capability was not associated with false-positive catheterization laboratory activation (p=0.123). Among the 264 patients referred with their official transfer note, 36 patients (13.6%) had been diagnoses with conditions other than STEMI, which were not associated with false-positive catheterization laboratory activation (p=0.465). The presenting symptoms in patients with the presumptive diagnosis of STEMI included chest pain in most patients (n=427; 93.8%), epigastric pain (n=7), dyspnea (n=5), mental status change (n=5), and syncope (n=3). Presenting symptoms other than chest pain were associated with false-positive catheterization laboratory activation (p=0.048). The in-hospital mortality was not different between the STEMI group and the false-positive STEMI group (p=1.000). During the 6-month follow-up period after the index admission, there were four all cause deaths (3 cardiac and 1 non-cardiac death) in the STEMI group. However, there was no all cause deaths in the false-positive STEMI group during 6-month follow-up period.
Comparisons of ECG parameters are listed in Table 2. Compared to the STEMI group, the false-positive group had a significantly higher proportion of left anterior descending artery (LAD, p=0.034), and a lower proportion of right coronary artery (p=0.018) as suspected ECG territory for STEMI. Proportions of ST-segment elevation in leads III (p=0.003) or aVF (p=0.003) were significantly higher in the STEMI group and the proportion of ST-segment elevation in lead V 3 (p=0.006) was significantly higher in the false-positive STEMI group. The number of leads with ST-segment elevation (p=0.389) and the height of maximal ST-segment elevation (p=0.534) were not different between the two groups. LVH (27.3% vs. 14.0%, p=0.041) and LBBB (5.9% vs. 0.5%, p=0.030) were significantly more prevalent in the false-positive STEMI group than in the STEMI group. However, Q waves (21.2% vs. 50.5%, p=0.005) and reciprocal changes (24.2% vs. 74.7%, p<0.001) were significantly less common in the false-positive STEMI group than in the STEMI group. Among the STEMI group, reciprocal changes were significantly more common in patients with inferior STEMI than in patients with anterior STEMI (95.3% vs. 53.2%, p<0.001).
The causes of false-positive catheterization laboratory activation among the 34 patients are listed in Table 3. Among these patients, 16 (3.5%) had positive and 18 (4.0%) had negative cTnI results. Common causes of false-positive diagnosis were coronary spasm in 10, LVH in 5, myocarditis in 4, early repolarization in 3, and previous MI and stress-induced cardiomyopathy in 2 each. Aortic dissection, unstable angina, pericarditis, mediastinitis, pericardial fat necrosis, cholecystitis, LBBB and RBBB on ECG were found to be uncommon causes of false-positive catheterization laboratory activation.
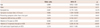
Multivariate logistic regression analysis as described in Table 4 indicated that symptom-to-door time >12 hours {odds ratio (OR) 4.995, 95% confidence interval (CI) 1.384-18.030, p=0.014}, presenting symptom other than chest pain (OR 7.709, 95% CI 1.255-39.922, p=0.027), absence of Q wave (OR 9.082, 95% CI 2.631-31.351, p<0.001) and absence of reciprocal changes on ECG (OR 17.987, 95% CI 5.295-61.106, p<0.001) were independent predictors of false-positive catheterization laboratory activation after adjusting for age, gender, dyslipidemia, suspicious LAD territory and LVH on ECG.
The primary finding of the present study was the 7.5% prevalence of false-positive diagnosis of STEMI and subsequent inappropriate catheterization laboratory activation with predominant causes of coronary spasm, LVH, and myocarditis. Among ECG parameters, the absence of Q wave and reciprocal changes were important independent predictors of false-positive catheterization laboratory activation.
Door-to-balloon time in the setting of STEMI is an important predictor of clinical events and outcomes.1)2) Rapid interpretation of ST-segment elevation on ECG is essential for decreasing door-to-balloon time in patients with suspected STEMI.3)4) However, the decision to provide immediate reperfusion therapy to patients presenting with chest pain and ST-segment elevation is not always easy to make because ST-segment elevation in conditions other than STEMI is not rare.5-16) The common causes of ST-segment elevation include early repolarization pattern, normal male-pattern ST-changes, LVH, LBBB, pericarditis and ventricular aneurysm.5-9) Acute myocarditis, Brugada syndrome, stress-induced cardiomyopathy, aortic dissection, myocardial bridge and coronary spasm are also known rare causes of ST-segment elevation that are not rarely mistaken for MI.10-16) In this study, the etiologies of false-positive catheterization laboratory activation were different from those documented in several studies from Western countries.14)17)18) The proportion of coronary spasm (29.4% vs. 1-7%) was significantly higher and the proportion of pericarditis (2.9% vs. 11-83%) was lower in this study. The proportions of LVH, early repolarization, stress-induced cardiomyopathy and myocarditis were not different.14)17)18) It is well known that the prevalence of coronary spasm appears to be higher in the far East than in the West,15) and this racial difference is most likely one explanation of the higher proportion of coronary spasm in this study. Brugada syndrome, which is known to be more common in Asians than in Caucasians,11) and myocardial bridge was not a cause of falsepositive STEMI diagnosis in the present study.
In Korea, the government urges every hospital performing primary PCI to reduce the door-to-balloon time in cases of STEMI treated with primary PCI to less than 90 minutes, ideally less than 60 minutes, and achievement of shorter mean door-to-balloon time became one of the most important factors in grading hospitals and reimbursement in the management of patients with STEMI. However, as the interhospital transport system for STEMI patients has not been firmly established in most parts of Korea, patient data such as ECG are usually not available until the arrival of the patient. Relatively higher proportion of coronary spasm among cases of falsepositive STEMI in this study might be associated with no proper interhospital referral system in place.
In the present study, symptom-to-door time >12 hours was an independent predictor of false-positive catheterization laboratory activation. Also pathologic Q wave, associated with time delay and infarct size in the course of acute MI,25) had significance. A previous study9) reported that half the cases of false-positive diagnosis of STEMI were in patients with previous MI and in these patients, the distinction between ST-segment changes due to old and new MI were very difficult. However, in the present study, Q waves were more prevalent in the STEMI group than in the false-positive group, implying their clinical significance in the diagnosis of STEMI. Our study showed that the absence of reciprocal changes was the most important independent predictor of false-positive diagnosis of STEMI. Reciprocal changes were reported to be as more frequent in patients with inferior STEMI compared with anterior STEMI26)27) as observed in this study (95.3% vs. 53.2%, p<0.001). Among the patients with anterior STEMI, patients with a LAD artery lesion proximal to the first diagonal branch and a wrapped LAD artery, or with a LAD artery lesion distal to the diagonal branch and a nonwrapped LAD artery do not have a reciprocal change.20) Despite the limitations in anterior STEMI, the presence of reciprocal changes on ECG is very useful for the rapid and correct diagnosis of STEMI in patients with a suspected inferior STEMI, although it lacks specificity.
There are several limitations in this study. First, this was a single-center observational study with a relatively small sample size. Second, an overemphasis on false-positive STEMI may induce under diagnosis of true STEMI potentially leading to fatal prognosis of patients. However, the rate of false-negative diagnosis of STEMI was not evaluated since this study focused on false-positive diagnosis of STEMI.
In conclusion, false-positive diagnosis of STEMI and subsequent inappropriate catheterization laboratory activation were not rare. Prudent ECG interpretation and consideration of ST-segment elevation on ECG in conditions other than STEMI may reduce inappropriate catheterization laboratory activation.
Figures and Tables
Table 1
Comparison of demographic and clinical characteristics between the STEMI group and the false-positive group

Acknowledgments
We thank Dr. SungHee Kim for her assistance with the preparation of this manuscript.
References
1. Watanabe K, Nagao K, Watanabe I, Kanmatsuse K. Relationship between the door-to-TIMI-3 flow time and the infarct size in patients suffering from acute myocardial infarction: analysis based on the fibrinolysis and subsequent transluminal (FAST-3) trial. Circ J. 2004; 68:280–285.
2. Brodie BR, Hansen C, Stuckey TD, et al. Door-to-balloon time with primary percutaneous coronary intervention for acute myocardial infarction impacts late cardiac mortality in high-risk patients and patients presenting early after the onset of symptoms. J Am Coll Cardiol. 2006; 47:289–295.
3. Nakayama N, Kimura K, Endo T, et al. Current status of emergency care for ST-elevation myocardial infarction in an urban setting in Japan. Circ J. 2009; 73:484–489.
4. Yan RT, Yan AT, Allegrone J, et al. Differences between local hospital and core laboratory interpretation of the admission electrocardiogram in patients with acute coronary syndromes and their relation to outcome. Am J Cardiol. 2007; 100:169–174.
5. Turnipseed SD, Bair AE, Kirk JD, Diercks DB, Tabar P, Amsterdam EA. Electrocardiogram differentiation of benign early repolarization versus acute myocardial infarction by emergency physicians and cardiologists. Acad Emerg Med. 2006; 13:961–966.
6. Surawicz B, Parikh SR. Prevalence of male and female patterns of early ventricular repolarization in the normal ECG of males and females from childhood to old age. J Am Coll Cardiol. 2002; 40:1870–1876.
7. Sgarbossa EB, Pinski SL, Barbagelata A, et al. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. GUSTO-1 (Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries) Investigators. N Engl J Med. 1996; 334:481–487.
8. Lange RA, Hillis LD. Clinical practice. Acute pericarditis. N Engl J Med. 2004; 351:2195–2202.
9. Miller DH, Kligfield P, Schreiber TL, Borer JS. Relationship of prior myocardial infarction to false-positive electrocardiographic diagnosis of acute injury in patients with chest pain. Arch Intern Med. 1987; 147:257–261.
10. Ahmar W, Lefkovits J. Acute ST elevation myocardial infarction with angiographically normal coronary arteries: causes and outcomes. Int J Cardiol. 2008; 128:131–133.
11. Takagi M, Yokoyama Y, Aonuma K, Aihara N, Hiraoka M. Japan Idiopathic Ventricular Fibrillation Study (J-IVFS) Investigators. Clinical characteristics and risk stratification in symptomatic and asymptomatic patients with brugada syndrome: multicenter study in Japan. J Cardiovasc Electrophysiol. 2007; 18:1244–1251.
12. Prasad A. Apical ballooning syndrome: an important differential diagnosis of acute myocardial infarction. Circulation. 2007; 115:e56–e59.
13. Klinceva M, Widimský P, Pesl L, et al. Prevalence of stress-induced myocardial stunning (Tako-Tsubo cardiomyopathy) among patients undergoing emergency coronary angiography for suspected acute myocardial infarction. Int J Cardiol. 2007; 120:411–413.
14. Gu YL, Svilaas T, van der, Zijlstra F. Conditions mimicking acute ST-segment elevation myocardial infarction in patients referred for primary percutaneous coronary intervention. Neth Heart J. 2008; 16:325–331.
15. Kim PJ, Seung KB, Kim DB, et al. Clinical and angiographic characteristics of acute myocardial infarction caused by vasospastic angina without organic coronary heart disease. Circ J. 2007; 71:1383–1386.
16. Kang WY, Jeong MH, Ahn YK, et al. Are patients with angiographically near-normal coronary arteries who present as acute myocardial infarction actually safe? Int J Cardiol. 2011; 146:207–212.
17. Larson DM, Menssen KM, Sharkey SW, et al. "False-positive" cardiac catheterization laboratory activation among patients with suspected ST-segment elevation myocardial infarction. JAMA. 2007; 298:2754–2760.
18. Prasad SB, Richards DA, Sadick N, Ong AT, Kovoor P. Clinical and electrocardiographic correlates of normal coronary angiography in patients referred for primary percutaneous coronary intervention. Am J Cardiol. 2008; 102:155–159.
19. Al-Faleh H, Fu Y, Wagner G, et al. Unraveling the spectrum of left bundle branch block in acute myocardial infarction: insights from the Assessment of the Safety and Efficacy of a New Thrombolytic (ASSENT 2 and 3) trials. Am Heart J. 2006; 151:10–15.
20. Sasaki K, Yotsukura M, Sakata K, Yoshino H, Ishikawa K. Relation of ST-segment changes in inferior leads during anterior wall acute myocardial infarction to length and occlusion site of the left anterior descending coronary artery. Am J Cardiol. 2001; 87:1340–1345.
21. Feldman AM, McNamara D. Myocarditis. N Engl J Med. 2000; 343:1388–1398.
22. Lee JW, Kim JY, Youn YJ, et al. Clinical characteristics and prognostic factors of stress-induced cardiomyopathy. Korean Circ J. 2010; 40:277–282.
23. Hung MJ, Cheng CW, Yang NI, Hung MY, Cherng WJ. Coronary vasospasm-induced acute coronary syndrome complicated by life-threatening cardiac arrhythmias in patients without hemodynamically significant coronary artery disease. Int J Cardiol. 2007; 117:37–44.
24. Antikainen RL, Grodzicki T, Palmer AJ, et al. Left ventricular hypertrophy determined by Sokolow-Lyon criteria: a different predictor in women than in men? J Hum Hypertens. 2006; 20:451–459.
25. Das MK, Khan B, Jacob S, Kumar A, Mahenthiran J. Significance of a fragmented QRS complex versus a Q wave in patients with coronary artery disease. Circulation. 2006; 113:2495–2501.
26. Peterson ED, Hathaway WR, Zabel KM, et al. Prognostic significance of precordial ST segment depression during inferior myocardial infarction in the thrombolytic era: results in 16,521 patients. J Am Coll Cardiol. 1996; 28:305–312.
27. Tsuka Y, Sugiura T, Hatada K, Abe Y, Takahashi N, Iwasaka T. Clinical characteristics of ST-segment elevation in lead V6 in patients with Q-wave acute inferior wall myocardial infarction. Coron Artery Dis. 1999; 10:465–469.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download