Abstract
Background and Objectives
The purposes of this study are 1) to investigate the relationship between resting baseline Pd/Pa, determined by the ratio of the pressures proximal (Pa) and distal (Pd) to the target lesion before, inducing hyperemia and fractional flow reserve (FFR) and 2) to identify a resting baseline Pd/Pa range that might reliably preclude the need for hyperemic induction.
Subjects and Methods
A total of 622 pressure wire data sets obtained from intermediate stenotic lesions were analyzed.
Results
There was a good linear relationship between resting baseline Pd/Pa and FFR (r=0.746, p<0.001). Receiver-operating characteristic curves of the resting baseline Pd/Pa with FFR ≤0.80 as the reference variable showed an area under the curve of 0.89 (95% confidence intervals 0.863-0.914, p<0.001) with a diagnostic accuracy of 82.3% when the resting baseline Pd/Pa was ≤0.92. These results showed that certain cutoff values can reliably predict FFR, whether positive or negative. The resting baseline Pd/Pa >0.95 (n=257, 41.3%) had a negative predictive value (NPV) of 98.1% and a sensitivity of 97.3%. the resting baseline Pd/Pa ≤0.88 (n=65, 10.5%) had a positive predictive value (PPV) of 96.2% and a specificity of 99.8%. These were consistent regardless of coronary vessel, lesion location, lesion length, or degree of stenosis.
For decades, functional assessment of coronary artery stenosis in the catheterization laboratory has been performed by measuring the coronary flow reserve and/or fractional flow reserve (FFR).1) In contemporary guidelines, FFR is the most widely used index as a surrogate test for the detection of myocardial ischemia.2) However, the utility of the pressure wire remains low due to several limitations in measuring FFR, most notably the high cost, laboriousness of this manual procedure, and possible adverse systemic effects of adenosine administration, such as bradyarrhythmia, chest pain, or bronchospasm.3) FFR is determined by the ratio of the pressures proximal (Pa) and distal (Pd) to the target lesion under maximal hyperemia.4) The pressure gradient across the stenotic lesion becomes greater as blood flow across the lesion increases during induction of hyperemia (flow augmentation). We have studied this pressure change across the stenotic lesion in response to flow augmentation, while investigating the relationship between the resting baseline Pd/Pa and FFR.5) Based on this relationship, we also determined the resting baseline Pd/Pa range that might reliably preclude the necessity for induction of hyperemia to determine the functional significance of the lesion.
We retrospectively investigated a total of 622 pressure wire data sets from 452 patients obtained during routine clinical practice at the Cardiovascular Center at Pusan National University Yangsan Hospital (Yangsan, Korea), from December 2008 through November 2011. We excluded pressure wire data for infarction-affected arteries or for the resting baseline Pd/Pa ≤0.80, and cases of minimal diameter stenosis assessed by subsequent quantitative coronary angiography (QCA) analysis. This study was approved by the Institutional Review Board of Pusan National University Yangsan Hospital.
Invasive conventional coronary angiography was performed by standard techniques using either a transradial or transfemoral approach. At least four views of the left and two views of the right coronary arteries were obtained. Intermediate coronary artery stenosis was defined as a diameter stenosis of 40-70% by visual estimation by two expert interventional cardiologists. A physiological study was also performed to assess the intermediate stenotic lesions, using a pressure wire (Radi Medical Systems, St. Jude Medical, Inc., USA). Hemodynamic measurements, including heart rate and aortic blood pressure, and the ratio of differential pressure at the aorta and distal to the stenosis were recorded continuously and stored throughout all phases of the study. Maximal hyperemia was induced by continuous intravenous infusion (140 µg/kg/min) of adenosine through the large forearm (antecubital) vein, following a standard protocol. We did not get the pullback data for the resting baseline Pd/Pa. Lesions with FFR ≤0.8 were considered functionally significant. Coronary angiograms were analyzed using QCA software (QantCor, QCA, Pie Medical Imaging, Maastricht, the Netherlands) by cardiologists who were blinded to the data of pressure wire study.
All statistical analyses were performed using Statistical Package for the Social Sciences software version 15.0 for Windows (IBM Corp. Armonk, NY, USA), and MedCalc software version 11.4 (MedCalc®, Mariakerke, Belgium). Continuous variables are expressed as the mean±standard deviation and categorical variables as frequencies (N) and percentages (%). Pearson's correlation coefficient (r) was used to assess the relationship between the resting baseline Pd/Pa and FFR. Receiver-operating characteristic (ROC) area under the curve (AUC) analysis was used to estimate the diagnostic performance of resting baseline Pd/Pa and to identify the appropriate cutoff value compared with the FFR threshold of 0.8. Sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV) with corresponding 95% confidence intervals (CI) were calculated. Subgroup analyses were also performed according to the diseased vessel {left anterior descending artery (LAD), left circumflex artery (LCx), or right coronary artery (RCA)}, lesion location (proximal or mid-to-distal), lesion length (<20 mm or ≥20 mm) and diameter stenosis by QCA (<50% or ≥50%).
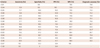
A total of 622 pressure wire data sets from 452 patients were analyzed retrospectively. The resting baseline characteristics of patients are presented in Table 1. The mean age was 63.0±9.9 years, and 323 patients (71.5%) were men. One hundred twenty-two patients (27.0%) had diabetes mellitus, 207 patients (45.8%) had hypertension, 102 patients (22.6%) had dyslipidemia, and 134 patients (29.6%) were current or former smokers. Patients had been referred for coronary angiography for stable angina (49.3%), unstable angina (27.0%), myocardial infarction (14.2%), or other reasons (9.5%), including atypical chest pain, silent ischemia, syncope, or structural heart disease. The target vessels were the left main coronary artery in 13 (2.5%) cases, LAD in 332 (53.4%) cases, LCx in 127 (20.4%) cases, and RCA in 150 (24.1%) cases. QCA results are also presented in Table 1. The mean diameter stenosis was 54.0±8.0% and the mean lesion length was 26.0±12.8 mm.
The range of resting baseline Pd/Pa values was 0.81 to 1.0, and the range of FFR values was 0.47 to 1.0. Based on the established FFR cutoff threshold of 0.8 to define a positive result, 183 of 622 (29.4%) lesions were considered functionally significant (positive) and 439 of 622 (70.6%) lesions were considered functionally non-significant (negative). Pearson's correlation analysis between the resting baseline Pd/Pa and diameter stenosis, as well as between FFR and diameter stenosis showed poor linear relationships in terms of its strength: r=-0.285 between the resting baseline Pd/Pa and diameter stenosis (p<0.001) (Fig. 1A), and r=-0.373 between FFR and diameter stenosis (p<0.001) (Fig. 1B). By contrast, there was a good linear relationship between the resting baseline Pd/Pa and FFR (r=0.746, p<0.001) (Fig. 1C).
The ROC curve for the resting baseline Pd/Pa, using an FFR ≤0.80 as the reference standard variable showed an AUC of 0.89 (95% CI=0.863-0.914, p<0.001). The resting baseline Pd/Pa ≤0.92 was associated with the greatest diagnostic accuracy (82.3%) for the prediction of FFR, whether positive or negative (Fig. 2, Table 2). Examining the diagnostic test performances according to the value for the resting baseline Pd/Pa more closely, we found two arbitrary points for the resting baseline Pd/Pa. At one point, the sensitivity and NPV began to decrease simultaneously and at the other point, the specificity and PPV began to descend simultaneously (Fig. 3). These patterns indicated that the resting baseline Pd/Pa >0.95 had >97% sensitivity and >98% NPV, and that the resting baseline Pd/Pa ≤0.88 had >98% specificity and >90% PPV.
When the resting baseline Pd/Pa was >0.95, as was the case in 257 of 622 (41.3%) data sets, sensitivity was 97.3% (95% CI=93.7-99.1%), NPV was 98.1% (95% CI=95.5-99.4%), specificity was 57.4% (95% CI=52.6-62.1%), and PPV was 48.8% (95% CI=43.5-54.0%). In the subgroup analysis, the sensitivity and NPV were consistently high, regardless of the diseased vessel (LAD or LCx/RCA), lesion location (proximal or mid-to-distal), lesion length (≤20 mm or >20 mm), or diameter stenosis (<50% or ≥50%) (Table 3-1).
When the resting baseline Pd/Pa was ≤0.88, which was the case in 65 of 622 (10.5%) data sets, specificity was 98.6% (95% CI=97.0-99.5%), PPV was 90.8% (95% CI=81.0-96.5%), sensitivity was 32.2% (95% CI=25.5-39.5%), and NPV was 77.7% (95% CI=74.1-81.1%). In the subgroup analysis, the specificity and PPV were consistently high, regardless of the diseased vessel (LAD or LCx/RCA), lesion location (proximal or mid-to-distal), lesion length (≤20 mm or >20 mm), or diameter stenosis (<50% or ≥50%) (Table 3-2).
Our study demonstrated that there is a range of the resting baseline Pd/Pa values that may reliably predict FFR guided lesion significance before the induction of hyperemia in company with a good correlation between the resting baseline Pd/Pa and FFR (r=0.746, p<0.001) (Fig. 1C).
The concept of an instantaneous wave-free ratio (iFR) introduced recently by the authors of the ADVISE study has attracted interest.6) However, this drug-free index of stenosis severity correlates weakly with FFR and seems not to be independent of hyperemia. In the VERIFY study by Berry et al.7) the diagnostic accuracy of an iFR value ≤0.80 was only 60% for all vessels, compared with the FFR cutoff value of ≤0.80. The resting baseline Pd/Pa has similar limitations to iFR. The resting baseline Pd/Pa can change under various situations. Different degrees of stenosis with identical resting baseline Pd/Pa can generate completely different FFR values. In our study, the diagnostic accuracy of the resting baseline Pd/Pa was 82.3% at best when used with the FFR cutoff value of ≤0.80. This suggests that the diagnostic accuracy is not high enough to justify skipping hyperemic induction for FFR measurement (Fig. 2). In particular, the diagnostic accuracy of the resting baseline Pd/Pa of 0.89-0.95 was very poor, and this range might have limited clinical usefulness. By contrast, when we examined more closely of the NPV and PPV of the resting baseline Pd/Pa together with their corresponding sensitivity or specificity simultaneously, the resting baseline Pd/Pa >0.95 or ≤0.88 appeared to be reliable points that predicted negative or positive FFR without losing its accurate diagnostic performances (Fig. 3).
We noted that about half of the cases of angiographically intermediate lesions had resting baseline Pd/Pa >0.95 (n=257, 41.3%) or ≤0.88 (n=65, 10.5%). These two cutoff values were not dependent on the vessel territory (LAD vs. non-LAD), lesion location (proximal vs. mid-to-distal), lesion length (short vs. long), or diameter stenosis (<50% vs. ≥50%). Our study result is similar to that of Mamas et al.8) who found a strong correlation between the resting Pd/Pa and FFR and a similar cutoff value for the resting baseline Pd/Pa (resting Pd/Pa ≥0.96 or ≤0.87). However, their study contained all of the consecutive pressure wire data, including tight or minimal stenotic lesions, which comprised about one-third of all cases, and did not demonstrate sensitivity, specificity, and predictive values for every decimal point of the resting baseline Pd/Pa measured simultaneously.
During FFR studies, pharmacologic vasodilation is essential for assessing the severity of stenosis, and adenosine is the most commonly used agent for inducing hyperemia. Although most patients feel chest discomfort or breathlessness during adenosine infusion, these side effects are short lived and well tolerated. Quite harmful or life-threatening systemic adverse reactions happen very rarely, and the only absolute contraindication for adenosine is severe bronchial asthma. As in previous studies,9)10) we failed to induce hyperemia using adenosine in a small number of patients (less than 1% of our accumulated data over the past 5 years) because of the unexpected bronchospasm, profound chest pain and atrioventricular conduction block. In such patients, other vasodilators, such as nicorandil, can be used safely and efficiently as the hyperemic agent for FFR measurements.12) However, some interventional cardiologists may still feel some pressure for using adenosine for the FFR study.
Our study has several limitations. First, our data were obtained from a single hospital center. However, we analyzed 622 pressure wire data sets from 452 patients and ensured that the volume of our data was quantitatively sufficient to get good quality results. Second, we routinely induced hyperemia using adenosine through the forearm (antecubital) vein, and not through the central (femoral) vein. In the study by Lindstaedt et al.,13) this method was slightly less effective than that of femoral vein infusion. However, recent studies by De Bruyne et al.14) and Seo et al.15) have shown that hyperemic efficacy of adenosine does not differ between infusion into the central vein and peripheral vein. Third, this study was performed in Korean patients with relatively low body mass index, and these results might not be directly applicable to patients with a large body mass index in Western populations.
In conclusion, the resting baseline Pd/Pa had good linear relationship with FFR in the intermediate lesions. A certain range of the resting baseline Pd/Pa values had an excellent NPV and sensitivity (resting baseline Pd/Pa >0.95) or PPV and specificity (resting baseline Pd/Pa ≤0.88) for determining lesion significance. These results might help the clinician predict the significance of the lesion without the need for inducing hyperemia to examine angiographically intermediate stenotic lesions. We hope that, by overcoming the perceived difficulties of assessing FFR, our study will facilitate wider use of the pressure wire for the purpose of increasing physiology-guided revascularization and consequent reduction of unnecessary percutaneous coronary intervention.
Figures and Tables
 | Fig. 1Scatter plots. A: scatter plots of diameter stenosis versus the resting baseline Pd/Pa (n=622, r=-0.285, p<0.001). B: scatter plots of diameter stenosis vs. FFR (n=622, r=-0.373, p<0.001). C: scatter plots of the resting baseline Pd/Pa vs. FFR (n=622, r=0.746, p<0.001). A single dot may represent many identical pressure wire data points. FFR: fractional flow reserve, r: Pearson's correlation coefficient. |
 | Fig. 2Receiver operating characteristic area under the curve (AUC) of the resting baseline Pd/Pa values, using FFR ≤0.80 as the reference standard variable. A: all vessels (AUC 0.89, n=662). B: left anterior descending artery (LAD; AUC 0.85, n=332). C: right coronary artery (RCA; AUC 0.93, n=150). D: left circumflex artery (LCx; AUC 0.84, n=127). FFR: fractional flow reserve. |
 | Fig. 3Diagnostic test performances according to the resting baseline Pd/Pa. When the resting baseline Pd/Pa was >0.95, sensitivity was 97.3% (95% CI=93.7-99.1%) and negative predictive value was 98.1% (95% CI=95.5-99.4%). When the resting baseline Pd/Pa was ≤0.88, specificity was 98.6% (95% CI=97.0-99.5%) and positive predictive value was 90.8% (95% CI=81.0-96.5%). CI: confidence intervals. |
Acknowledgments
This study was supported by a Medical Research Institute Grant (2012), Pusan National University Yangsan Hospital.
References
1. Tobis J, Azarbal B, Slavin L. Assessment of intermediate severity coronary lesions in the catheterization laboratory. J Am Coll Cardiol. 2007; 49:839–848.
2. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011; 124:e574–e651.
3. Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). European Association for Percutaneous Cardiovascular Interventions (EAPCI). Wijns W, et al. Guidelines on myocardial revascularization. Eur Heart J. 2010; 31:2501–2555.
4. Pijls NH, van Son JA, Kirkeeide RL, De Bruyne B, Gould KL. Experimental basis of determining maximum coronary, myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after percutaneous transluminal coronary angioplasty. Circulation. 1993; 87:1354–1367.
5. Kim JH, Park JH, Choo K, et al. Pressure-wire based assessment of microvascular resistance using calibrated upstream balloon obstruction: a predictor of myocardial viability. Catheter Cardiovasc Interv. 2012; 80:581–589.
6. Sen S, Escaned J, Malik IS, et al. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis: results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) study. J Am Coll Cardiol. 2012; 59:1392–1402.
7. Berry C, van't Veer M, Witt N, et al. VERIFY (VERification of Instantaneous Wave-Free Ratio and Fractional Flow Reserve for the Assessment of Coronary Artery Stenosis Severity in EverydaY Practice): A Multicenter Study in Consecutive Patients. J Am Coll Cardiol. 2013; 61:1421–1427.
8. Mamas MA, Horner S, Welch E, et al. Resting Pd/Pa measured with intracoronary pressure wire strongly predicts fractional flow reserve. J Invasive Cardiol. 2010; 22:260–265.
9. Tonino PA, DeBruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009; 360:213–224.
10. De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012; 367:991–1001.
11. Jung HO, Seung KB, Kim PJ, et al. Comparison between nicorandil and adenosine in the measurement of coronary flow reserve using a Doppler guide wire. Korean Circ J. 2002; 32:391–397.
12. Jang HJ, Koo BK, Lee HS, et al. Safety and efficacy of a novel hyperaemic agent, intracoronary nicorandil, for invasive physiological assessments in the cardiac catheterization laboratory. Eur Heart J. 2013; [Epub ahead of print].
13. Lindstaedt M, Bojara W, Holland-Letz T, et al. Adenosine-induced maximal coronary hyperemia for myocardial fractional flow reserve measurements: comparison of administration by femoral venous versus antecubital venous access. Clin Res Cardiol. 2009; 98:717–723.
14. De Bruyne B, Pijls NH, Barbato E, et al. Intracoronary and intravenous adenosine 5'-triphosphate, adenosine, papaverine, and contrast medium to assess fractional flow reserve in humans. Circulation. 2003; 107:1877–1883.
15. Seo MK, Koo BK, Kim JH, et al. Comparison of hyperemic efficacy between central and peripheral venous adenosine infusion for fractional flow reserve measurement. Circ Cardiovasc Interv. 2012; 5:401–405.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download