Abstract
We describe a case of chronic total occlusion of the right coronary artery ostium 5 months after a repeated Bentall procedure in a patient with Behçet's disease. In this patient, an antegrade approach to delivering the guidewire during percutaneous coronary intervention was not successful. Coronary angiography revealed the existence of collateral blood supply from the left coronary artery. Using a retrograde approach, a guidewire was successfully advanced from the distal left circumflex artery through the collateral vessel and into the posterolateral branch of the right coronary artery. After the guidewire crossed over the occluded right coronary artery ostium and was snared into the ascending aorta, antegrade access for balloon and stent delivery succeeded.
In Behçet's disease, coronary ostial stenosis following a Bentall procedure is rarely reported but can be fatal.1) Among chronic total occlusion (CTO) lesions, the ostial location is especially difficult to treat with percutaneous coronary intervention (PCI) due to the inability to engage the guiding catheter into the coronary artery. However a retrograde approach, has been recently introduced, which may increase the rate of success of PCI.2) Here we report a case of retrograde recanalization of a chronically occluded right coronary artery (RCA) ostium after a repeated Bentall procedure in a patient with Behçet's disease.
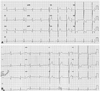
A 41-year-old man with Behçet's disease was referred to our outpatient clinic for treatment of CTO of the RCA ostium. He did not have any risk factors such as hypertension, diabetes, hyperlipidemia, and smoking. He had undergone a Bentall procedure for severe aortic regurgitation 10 years ago, and required reoperation on the aortic root replacement with Prima Plus 23 mm (Edwards Lifesciences, Irvine, CA, USA) and an ascending aortic graft insertion with Intergard 24 mm (Maquet, Wayne, NJ, USA) due to infective endocarditis 7 months prior. Two months earlier, he experienced rapidly worsening exertional angina and was evaluated at another hospital. Emergent coronary angiography showed a significant tubular lesion of the left main coronary artery (LMCA) ostium (Fig. 1A) and total occlusion of the RCA ostium (Fig. 1B). Stent implantation in the LMCA was successfully performed, but catheter engagement into the RCA failed due to CTO of the RCA ostium. On admission, electrocardiography revealed abnormal Q waves over the inferior leads (Fig. 2A), but cardiac magnetic resonance imaging showed no evidence of delayed enhancement. Echocardiography showed normal left ventricle systolic function and aortic valve function. Coronary angiography showed a patent LMCA stent and no disease in the left sided vasculature; however, the RCA ostium was totally occluded and collateral flow (grade 3) was supplied by the left coronary artery (Fig. 3A). We first attempted to use a 6 Fr JR 4 guiding catheter (Cordis, Miami, FL, USA) for an antegrade approach, but were unable to penetrate into the RCA ostium. Subsequently, a 5 Fr XB 3.5 guiding catheter (Cordis, Miami, FL, USA) was used in a retrograde approach via the right radial artery. We chose the left circumflex artery (LCX) for the retrograde approach. A superselective tip injection of contrast using a Finecross™ microcatheter (Terumo, Tokyo, Japan) was performed, and a channel from the LCX to the posterolateral branch of the RCA was confirmed. A Runthrough™ NS (Terumo, Tokyo, Japan) with a microcatheter was retrogradely advanced into the distal RCA, and further advanced into the distal end of the occlusion (Fig. 3B) before penetrating the CTO lesion (Fig. 3C). We then exchanged the Runthrough™ NS guidewire for a Fielder-FC™ 300 cm guidewire (Asahi Intecc, Aichi, Japan), which was subsequently snared into the ascending aorta (Fig. 3D) and pulled out of the sheath placed in the right femoral artery using a Multi-Snare® (PFM medical, CA, USA) (Fig. 3E). The lesion was pre-dilated using a 2.0×20 mm Lacrosse balloon (Goodman, Nagoya, Japan) at 18 atmospheres. A 3.0×28 mm Nobori® stent (Terumo, Tokyo, Japan) was then placed successfully in the CTO lesion at 16 atmospheres. Final angiographic findings showed no residual stenosis or complications (Fig. 3F). The medications of the previous hospital were maintained including colchicine 0.6 mg qd, azathioprine 50 mg qd, aspirin 100 mg qd, clopidogrel 75 mg qd, ramipril 5 mg qd, bisoprolol 5 mg qd, and atorvastatin 80 mg qd. He was referred back to the previous hospital.
Aneurysmal dilatations of the sinus of Valsalva and ascending aorta are more frequent in patients with Behçet's disease than in healthy subjects.3) The Bentall procedure for aortic root and valve replacement with coronary reimplantation is considered the gold standard for treatment of combined valve and ascending aortic pathology,4) with coronary ostial stenosis following this procedure occurring in less than 2% of patients.5) This complication may be related to an imperfect suture technique, or to the direct instrumentation of the coronary ostium itself. In these cases, signs of ischemia typically present early on during hospitalization.6) In recent reports, delayed ostial coronary stenosis occurring within months of the operation might be due to inflammatory and/or proliferative responses of the coronary wall to tissue adhesives used during the operation.7)8) Coronary artery stenosis in aortitis syndrome with the stenosis occurred two years after the operation has been reported.9) In our case, signs and symptoms of stenosis were observed 5 months after surgery. Thus, the time lapse between the procedure and the presentation of ostial occlusion implies a mechanism that is related to the tissue adhesion rather than the suture technique or Behçet's disease itself.
Our patient presented with acute myocardial infarction and underwent successful PCI of the LMCA ostium. It was not possible to perform this procedure using an antegrade approach to the CTO in the RCA ostium. It has been reported that successful revascularization of CTO leads to significantly reduced mortality rates and long term risk of adverse cardiac events.10)11) Retrograde CTO recanalization has recently become an essential alternative to the classical antegrade approach. When performed by an experienced clinician, the retrograde technique has a high success rate with a low complication profile, despite frequent utilization in the most anatomically and clinically complex patients.2) In retrograde CTO recanalization, analysis of all potential collateral channels is critical. The epicardial collaterals are preferred less than septal collaterals, because rupture could lead to tamponade and procedural ischemia or infarction may occur.2) However, we used the epicardial collateral because no septal collaterals are suitable. In addition, because the occlusion was located at the ostium of the coronary artery, there was no space to engage the antegrade guiding catheter. In such situation, a pure retrograde wire crossing is the only way to transverse the occlusion. The retrograde wire was able to advance to the false lumen and advancing more caused the dissection. If available for antegrade approach, the use of intravascular ultrasound through the antegrade system may prevent the engagement to the false lumen.12) However, if not available for antegrade wiring, we have no choice but to advance the retrograde wire carefully by an experienced operator. After crossing CTO lesion, either pushing the retrograde guidewire into the guiding catheter or trapping it at the contralateral sheet may be used for wire externalization.13) Through this retrograde approach, we were able to snare the 300 cm guidewire into the ascending aorta, and then ultimately pull it out of the proximal end of the femoral sheath.
In summary, we propose that a retrograde approach for PCI can be useful in the treatment of CTO of the coronary ostium as a consequence of the Bentall procedure in patients with Behçet's disease.
Figures and Tables
Fig. 1
Initial coronary angiography from the previous hospital. A: significant tubular stenosis at the left main coronary artery (white arrow). B: ostial occlusion with thrombolysis in myocardial infarction 1 flow at the right coronary artery (white arrow). C: final angiography after stent implantation of left main coronary artery at the previous hospital. Collateral flow supplied to proximal right coronary artery.

Fig. 3
Revascularization for chronic total occlusion (CTO) in right coronary artery. A: patent stent at the left main coronary artery. Collateral flow supplied from the left coronary artery to the right coronary artery (white arrows). B: a Finecross™ microcatheter (Terumo, Tokyo, Japan) was further advanced into the CTO lesion (white arrow). C: a Runthrough™ NS (Terumo, Tokyo, Japan) was crossed over the CTO lesion. D: snaring of the retrograde guidewire into the ascending aorta (white arrow). E: a retrograde guidewire was pulled out of the sheath placed in the right femoral artery (white arrow). F: final angiogram with no residual stenosis.

References
1. Nonoyama M, Tsuchida K. [A case report of sudden death after Bentall's operation (Piehler's modification) due to left coronary occlusion]. Kyobu Geka. 1997. 50:569–572.
2. Joyal D, Thompson CA, Grantham JA, Buller CE, Rinfret S. The retrograde technique for recanalization of chronic total occlusions: a step-by-step approach. JACC Cardiovasc Interv. 2012. 5:1–11.
3. Gürgün C, Ercan E, Ceyhan C, et al. Cardiovascular involvement in Behçet's disease. Jpn Heart J. 2002. 43:389–398.
4. Huang XM, Huang CJ, Sha Y, Wang Q, Zeng XJ. [Cardiac valve involvement in Behcet's disease: a clinical study of 10 patients]. Zhonghua Yi Xue Za Zhi. 2010. 90:2357–2359.
5. Worthley MI, Burgess J, Traboulsi M. Bilateral coronary ostial stenoses post-Bentall procedure: management options in the DES era. J Invasive Cardiol. 2005. 17:680–682.
6. Balbi M, Olivotti L, Scarano F, et al. Percutaneous treatment of left main coronary stenosis as a late complication of bentall operation for acute aortic dissection. Catheter Cardiovasc Interv. 2004. 62:343–345.
7. Marino M, Cellini C, Tsiopoulos V, et al. A case of myocardial infarction effectively treated by emergency coronary stenting soon after a Bentall-De Bono aortic surgery. Cardiovasc Revasc Med. 2010. 11:263.
8. Tsukui H, Aomi S, Nishida H, Endo M, Koyanagi H. Ostial stenosis of coronary arteries after complete replacement of aortic root using gelatin-resorcinol-formaldehyde glue. Ann Thorac Surg. 2001. 72:1733–1735.
9. Terasawa A, Kondo K, Ishikawa S, Morimoto R, Tajika T, Hayashi Y. Sirolimus-eluting stent implantation for ostial stenosis of left main coronary artery after Bentall operation in aortitis syndrome. J Cardiol. 2010. 55:147–150.
10. Joyal D, Afilalo J, Rinfret S. Effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis. Am Heart J. 2010. 160:179–187.
11. Rathore S, Katoh O, Matsuo H, et al. Retrograde percutaneous recanalization of chronic total occlusion of the coronary arteries: procedural outcomes and predictors of success in contemporary practice. Circ Cardiovasc Interv. 2009. 2:124–132.
12. Rathore S, Katoh O, Tuschikane E, Oida A, Suzuki T, Takase S. A novel modification of the retrograde approach for the recanalization of chronic total occlusion of the coronary arteries intravascular ultrasound-guided reverse controlled antegrade and retrograde tracking. JACC Cardiovasc Interv. 2010. 3:155–164.
13. Galassi AR, Tomasello SD, Costanzo L, Tamburino C. Retrograde recanalization of an in-stent ostial chronically occluded right coronary artery. Int J Cardiol. 2010. 142:304–306.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download