Abstract
Aortic coarctation is a correctable hypertensive disease. For safety reasons and due to the invasiveness of surgical techniques, percutaneous interventions have become drastically more popular in recent times. In elderly patients with aortic coarctation who are at risk of an aortic wall aneurysm and rupture, covered stents are preferred but in younger patients, bare metal stenting may be sufficient for long-term safety. Herein we present a 47-year-old typical aortic coarctation patient who was successfully treated with a bare metal stent.
Aortic coarctation is a rare disease entity in adults and a reversible cause of hypertension.1) Because surgical management is relatively invasive and has the possibility of serious complications such as paraplegia, paroxysmal hypertension, re-coarctation and aneurysms, percutaneous stent implantation has become a popular alternative.2)3) Research into which type of stent should be standard for coarctation has been inconclusive but in limited patients with Turner's syndrome or hypoplastic aortic arch, and in those suspected to have fragile blood vessels, treatment with a covered stent is recommended.4)5) However, covered stenting leads to the potential risk of critical complications such as occlusion of left subclavian artery, which may lead to acute paraplegia.6) Moreover, there are currently no flexible covered stents available in Korea as imports. Instead, there are several bare metal stents (BMS) for aortic coarctation available, made out of shape memory nitinol. These have the advantage of flexibility and conformability, as well as being safe in terms of vessel wall damage as they have soft ends. Unless there is clear evidence of fragile vessels, implantation of BMS may be another cost-effective and safe treatment option. This is the first report describing a case successfully managed by transcatheter treatment of aortic coarctation in an adult patient using BMS who had finished one year clinical follow-up at the time of writing.
A 47-year-old man presented to our hospital due to sustained headache and uncontrolled hypertension. The patient had a history of hypertension diagnosed approximately 10 years previously. His hypertension was poorly controlled despite a combination of three different antihypertensive agents (candesartan 16 mg DP, amlodipine 5 mg DP and hydrochlorothiazide 12.5 mg DP).
Physical examination showed a blood pressure of 140/80 mm Hg in both arms, a heart rate of 69 beats/minute and no audible murmur. There was no significant pathologic finding in the chest radiography. His echocardiogram showed enlarged sinus portion of ascending aorta with moderate aortic regurgitation (grade 3), suspicious of aortic aneurysm, but left ventricular systolic function was well preserved. Due to the significantly enlarged sinus portion of ascending aorta, the patient underwent multislice spiral computed tomography (CT) angiography for evaluation of aorta anatomy. CT angiography showed focal significant stenosis of the descending aorta, just below the left main pulmonary artery level with vigorous collateral blood flow (Fig. 1A). Invasive aortography was then performed, which showed severe aortic coarctation distal to the origin of subclavian artery (Fig. 2A). According to the quantitative aortography measurements, the coarctation segment was a minimum of 8 mm in diameter and 40 mm in length. The diameters of the thoracic aorta above and below the coarctation segment were 19 and 22 mm, respectively. The patient was then planned for elective percutaneous balloon dilatation with subsequent stent implantation.
Under the local anesthesia, bilateral retrograde femoral artery approach was carried out. A 7 Fr arterial sheath was inserted into the right femoral artery and then in sequence a 5 Fr arterial sheath was also inserted into the left femoral artery. After this, a 5 Fr pigtail catheter was placed at the coarctation segment following successful wiring with a 0.035 inch Terumo guidewire (Terumo, Tokyo, Japan). After baseline angiography was done, a pigtail catheter was removed for predilatation. Afterwards, multiple predilatation with an 8×40 mm PowerFlex balloon (Johnson & Johnson, Miami, FL, USA) was applied to the coarctation segment. Additional predilatation with a 10×40 mm PowerFlex balloon was followed sequentially. An aortic stent was successfully deployed using a 22×50 mm self-expandable nitinol stent (Hercules Vascular stent, S&G, Seongnam, Korea) (Fig. 3). Further to this, post-dilatation with a 12×40 mm Ultrathin balloon (Boston Scientific, Natick, MA, USA) was carried out.
Immediate after the stenting, final aortography revealed adequate patency of the stent in the coarctation segment of the thoracic aorta and showed correct device position without any dissection or perforation, with the diameter of the isthmus increased from 8 to 16 mm (Fig. 2B).
The patient has been prescribed acetyl salicylic acid 100 mg per day, which was continued until the latest visit. Clinical follow-up was performed at 1, 3 and 6 months after the procedure then continued at 4-month intervals. The patient's hypertension was well controlled using fewer antihypertensive medications on follow-up and his subjective symptoms disappeared shortly after the procedure. To date, the patient has been followed for 12 months in good clinical condition.
Follow-up multislice spiral CT angiography was performed at six months after the procedure and showed no significant re-stenosis within the stent of coarctation segment. Further, occlusion of abdominal aorta branches, aneurysm formation, or other related complications were not observed. CT angiography also showed tremendously diminished collateral blood flow compared with pre-procedural images (Fig. 1B).
Aortic coarctation is a congenital vascular lesion that is diagnosed in childhood in most cases, and accounts for 5 to 10% of all congenital cardiovascular malformations.7) However, it may sometimes not be diagnosed easily until adulthood.8) The clinical manifestations are distinguished according to the age groups. The neonate may remain asymptomatic due to patent ductus arteriosus. Heart failure is not frequent beyond the neonatal period, thus most infants and children also remain asymptomatic, leading to delayed diagnosis. In adults, the initial presenting sign is typically uncontrolled hypertension. There could be significant variability in measuring blood pressure in the upper and lower extremities but regional blood flow is usually well retained by the autoregulatory system. Most adult patients are also asymptomatic till severe hypertension give rise to headache, epistaxis, heart failure, or aortic dissection. Additionally, claudication may occur due to reduced blood flow to the lower extremities.9-11)
In 2008, the American College of Cardiology and American Heart Association suggested guidelines for adults with coarctation. The recommended indications for intervention include a high peak to peak coarctation gradient, anatomic imaging evidence of coarctation and radiologic evidence of significant collateral blood flow. Yet even in these guidelines, the optimal treatment for coarctation of the aorta in adults is left open to debate.12)
The endovascular technique for adult aortic coarctation has obtained a widespread popularity since the mid-1990s. In 2006, Carr13) published a comparison between angioplasty (stent, balloon dilatation or a combination; n=633) and surgery (n=213) in adult aortic coarctation patients, based on papers published during 1995-2005. Stenting had the lower morbidity (mean 9%, range 0-20%), whereas morbidity was slightly higher in the surgical group (mean 11%, range 0-25%), mainly related to bleeding and recurrent laryngeal nerve injury. Restenosis was found in 11% (range 0-25%) in the stented group, but in only 2% (range 0-9%) in the surgical group. Stenting restored hypertension in 61% of patients, compared to 64% after surgery. However, it is difficult to make recommendations because stent technology has progressed over time, producing superior stent designs. It may be necessary to set up a multicentre prospective randomized clinical trial comparing surgical modality to stenting in order to ascertain what is the best management method for aortic coarctation in adults.14)
Safety is one of the major advantages of percutaneous intervention, compared to surgical treatment. However, intervention techniques do have some potentially serious complications. Deaths related to aortic rupture and dissection during procedure are very rare,13)15) but other complications also exist. In many cases, authors report device migration and vascular injuries at the site of arterial cannulation. Stent fractures and balloon rupture are also potential complications of percutaneous intervention.
Covered stents are preferentially used for patients at risk of complications due to complex anatomy or advanced age.14) However there are several disadvantages, such as relatively small sheath size and potentiality of supra-aortic branch occlusion.16)17) The wide cost gap between BMS and covered stents is also problematic. However, to our knowledge, there is no single randomized control trial comparing between BMS and covered stent in mid-aged otherwise healthy candidates. As found in our case report, BMS can be safely deployed in selected patients and, moreover it has obvious advantage in terms of cost.
Efficacy and safety comparisons between the two types of stents will be needed to confirm the optimal modality for the treatment of aortic coarctation in adults.
Figures and Tables
Fig. 1
Pre- and post-procedural CT angiographic findings. A: pre-procedural CT angiography showing severe coarctation of descending aorta just below the left main pulmonary artery level (transparent arrow). Note vigorous collateral blood flow of anterior and posterior trunk (white arrows). B: post-procedural CT angiography showed increased isthmus diameter from 8 to 16 mm (transparent arrow). Diminished collateral blood flow was also observed (white arrows).

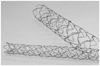
Fig. 2
Invasive angiographic images of pre- and post-stenting. A: thoracic aortography showed the coarctation segment of 8 mm in diameter and 40 mm in length (arrowheads). B: successful deployment of bare metal stent using a 22×50 mm self-expandable nitinol stent showing correct device position without any immediate dissection or perforation (arrowheads).

References
1. Keith DS, Markey B, Schiedler M. Successful long-term stenting of an atypical descending aortic coarctation. J Vasc Surg. 2002. 35:166–167.
2. Mullen MJ. Coarctation of the aorta in adults: do we need surgeons? Heart. 2003. 89:3–5.
3. Teixeira AM, Anjos R, Abecasis M, Cordeiro P, Ferreira R, Martins M. Stents for correction of aortic coarctation in adults. Rev Port Cardiol. 2005. 24:1559–1563.
4. Butera G, Piazza L, Chessa M, et al. Covered stents in patients with complex aortic coarctations. Am Heart J. 2007. 154:795–800.
5. Tzifa A, Ewert P, Brzezinska-Rajszys G, et al. Covered Cheatham-platinum stents for aortic coarctation: early and intermediate-term results. J Am Coll Cardiol. 2006. 47:1457–1463.
6. Orend KH, Zarbis N, Schelzig H, Halter G, Lang G, Sunder-Plassmann L. Endovascular treatment (EVT) of acute traumatic lesions of the descending thoracic aorta--7 years' experience. Eur J Vasc Endovasc Surg. 2007. 34:666–672.
7. Grech V. Diagnostic and surgical trends, and epidemiology of coarctation of the aorta in a population-based study. Int J Cardiol. 1999. 68:197–202.
8. Cevik S, Izgi C, Cevik C. Asymptomatic severe aortic coarctation in an 80-year-old man. Tex Heart Inst J. 2004. 31:429–431.
9. Brickner ME, Hillis LD, Lange RA. Congenital heart disease in adults. First of two parts. N Engl J Med. 2000. 342:256–263.
10. Kenny D, Hijazi ZM. Coarctation of the aorta: from fetal life to adulthood. Cardiol J. 2011. 18:487–495.
11. Tanous D, Benson LN, Horlick EM. Coarctation of the aorta: evaluation and management. Curr Opin Cardiol. 2009. 24:509–515.
12. Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines on the management of adults with congenital heart disease). Circulation. 2008. 118:e714–e833.
13. Carr JA. The results of catheter-based therapy compared with surgical repair of adult aortic coarctation. J Am Coll Cardiol. 2006. 47:1101–1107.
14. Godart F. Intravascular stenting for the treatment of coarctation of the aorta in adolescent and adult patients. Arch Cardiovasc Dis. 2011. 104:627–635.
15. Forbes TJ, Garekar S, Amin Z, et al. Procedural results and acute complications in stenting native and recurrent coarctation of the aorta in patients over 4 years of age: a multi-institutional study. Catheter Cardiovasc Interv. 2007. 70:276–285.
16. Rehders TC, Petzsch M, Ince H, et al. Intentional occlusion of the left subclavian artery during stent-graft implantation in the thoracic aorta: risk and relevance. J Endovasc Ther. 2004. 11:659–666.
17. Butera G, Manica JL, Chessa M, et al. Covered-stent implantation to treat aortic coarctation. Expert Rev Med Devices. 2012. 9:123–130.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download