Abstract
A 67-year-old male patient was admitted with an abrupt sudden cardiac death. He represented with an extreme electrical storm of 30 times of ventricular fibrillation (VF) episodes on one day. External shocks were performed to terminate VF. Transient J-wave in the inferior-lateral leads and Brugada electrocardiography pattern on the right precordial leads appeared during the electrical storm. And J-wave disappeared after the termination of electrical storm. We report a case of the appearance of J-wave during electrical storm in a patient with Brugada syndrome.
Brugada syndrome is a hereditary arrhythmogenic disease characterized by ST elevation in the right precordial lead of standard electrocardiography (ECG), and is known to increase the risk of sudden cardiac death.1) Recent studies have confirmed a clear association of early repolarization (ER) with sudden cardiac death in patients with idiopathic ventricular fibrillation (VF).2) Brugada syndrome and ER abnormality seem to share a common mechanism that results in ECG changes, caused by the loss of the transient outward potassium current (Ito)-mediated action potential dome in the epicardium.3) It has been demonstrated that ER abnormality in the inferior-lateral leads can also be observed in the Brugada syndrome.4) The role of ER abnormality in the inferior-lateral leads is far from being clarified in the Brugada syndrome. We report a case on the appearance of transient J-wave in the inferior-lateral leads during electrical storm in a patient with Brugada syndrome.
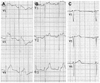
A 67-year-old man presented to the emergency room of our hospital at midnight after resuscitated cardiac arrest which was witnessed. He had no relevant past medical history except for gastroesophageal reflux disease. He had fallen asleep at approximately 11:30 p.m., but at 11:39 p.m. his wife noticed that he had fallen into sudden apnea and stiffness. His son called 119 (emergency medical service) and performed cardiopulmonary resuscitation for 3 minutes before the emergency teams arrived. On arrival at our emergency room he appeared to be acutely ill-looking, and his mental state was alert. His vital signs were as follows: blood pressure 93/70 mm Hg, pulse rate of 112 bpm, body temperature 36.0℃. Laboratory results including complete blood count, biochemistry profile, electrolyte panels, cardiac enzymes ware within normal limits. The chest radiograph was also normal. While the patient was rushed to our hospital by ambulance, VF occurred 3 times. He was defibrillated with Automated External Defibrillator but VF occurred repeatedly. As he continued to develop VF, he was defibrillated 30 times until 9 a.m. (Fig. 1). The 12-lead ECG, initially recorded in the emergency room, revealed normal sinus rhythm with a heart rate of 93 bpm. There was coved type-ST elevation in V 1-2 and J-wave in II, III, aVF, V 5-6 leads (Fig. 2B). Based on his family history, we found that his elder brother died in his sleep, when he was in his thirties. Furthermore, considering spontaneous presence of Brugada ECG patterns in the right precordial leads during the electrical stimulation (Fig. 3), we diagnosed him to have Brugada syndrome. Myocardial infarction was ruled out by coronary angiography with negative results of ergonovine test. We have no results of IC challenge test because we had no drug (e.g., flecainide) for the test, and we concluded that IC challenge test was not necessary because the patient had a typical pattern of Brugada syndrome on ECG. The Implantable Cardioverter Defibrillator was implanted for secondary prevention. Interestingly, abnormal low-amplitude terminal QRS deflection (J-wave), which was present in the inferior-lateral leads during VF storm (Fig. 2B) disappeared when his status became stable, without any VF recurrence (Fig. 2A). An ECG taken five years ago showed normal sinus rhythm and no J-wave on the inferior-lateral leads and no Brugada pattern ECG on the right precordial leads (Fig. 2A).
This report shows the transient presence of J-wave in the inferior-lateral leads during electrical stimulation in a patient with Brugada syndrome. There was no J-wave in the ECG that was checked 5 years ago. The J-wave disappeared after the patient's rhythm became stabilized. We are not certain if the appearance of J-wave is associated with electrical stimulation or with a secondary effect of direct current (DC) shock.
Recently, ER abnormalities, such as J-wave presence, have been associated with idiopathic VF, and in certain cases the increase in the J point and ST elevation has preceded spontaneous episodes of VF. It has been demonstrated that 11% of patients with Brugada syndrome have ER abnormalities, such as presence of J-wave in the inferior-lateral leads.4) Until now the meaning of ER abnormality in Brugada syndrome was not known. Letsas et al.5) reported that the ER sign is not a poor prognosis for Brugada syndrome. However, Kamakura et al.6) has shown that ER means an indicator of poor prognosis in patients with Brugada syndrome.
Sorgente et al.7) showed that the patient recovered from VF essentially has J-wave on the inferior-lateral leads, and after DC cardioversion, J-wave transiently disappeared and then Type I Brugada ECG pattern in the right precordial leads was documented by ajmaline test. This report informed us that exclusion of diagnosis of Brugada syndrome is important before we consider VF survivors to be suffering from J-wave syndrome.
The present case showed the transient appearance of J-wave on the inferior-lateral leads and several Brugada ECG patterns in the right precordial leads during electrical stimulation. However, after electrical stimulation was terminated and sinus rhythm was stabilized, Brugada ECG pattern in the right precordial leads and J-wave in the inferior-lateral leads disappeared. The history of syncope or sudden cardiac death, spontaneous ECG type of Brugada syndrome, symptoms or positive genetic test for SCN5NA mutations have already been proven to be related with risk factors for Brugada syndrome.5) Considering the present case, a transient appearance of J-wave can be associated with spontaneous episodes of VF in some cases of Brugada syndrome. Nevertheless, we need further studies with a larger population and discussions on the exact mechanism of appearance of J-wave.
Figures and Tables
 | Fig. 2A: electrocardiography (ECG) showed normal QRS complex (no J wave and no Brugada ECG pattern) after termination of electrical storm, which had the same pattern to one taken 5 years previously. B: ECG showed J wave in II, III, aVF, V 5-6 lead, and coved type Brugada pattern in V 1-2 leads during electrical storm. |
References
1. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992. 20:1391–1396.
2. Haïssaguerre M, Derval N, Sacher F, et al. Sudden cardiac arrest associated with early repolarization. N Engl J Med. 2008. 358:2016–2023.
3. Yan GX, Antzelevitch C. Cellular basis for the electrocardiographic J wave. Circulation. 1996. 93:372–379.
4. Sarkozy A, Chierchia GB, Paparella G, et al. Inferior and lateral electrocardiographic repolarization abnormalities in Brugada syndrome. Circ Arrhythm Electrophysiol. 2009. 2:154–161.
5. Letsas KP, Sacher F, Probst V, et al. Prevalence of early repolarization pattern in inferolateral leads in patients with Brugada syndrome. Heart Rhythm. 2008. 5:1685–1689.
6. Kamakura S, Ohe T, Nakazawa K, et al. Long-term prognosis of probands with Brugada-pattern ST-elevation in leads V1-V3. Circ Arrhythm Electrophysiol. 2009. 2:495–503.
7. Sorgente A, Sarkozy A, Brugada P. J-wave disappearance immediately after an episode of ventricular fibrillation in a patient with resuscitated sudden cardiac death and Brugada syndrome. J Cardiovasc Electrophysiol. 2010. 21:1413–1415.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download