Abstract
Background and Objectives
We evaluated the long-term outcomes and predictors of clinical events after off-label use of drug-eluting stents (DES) beyond 1 year after procedure.
Subjects and Methods
A total of 518 patients who underwent DES implantation for off-label indications and did not have any major adverse cardiac events (MACE) during the first year were analyzed. The occurrence of MACE, including cardiac death, myocardial infarction (MI), stent thrombosis and target vessel revascularization, were evaluated for a median 1179 days (interquartile range 769-1541) after the first year.
Results
Major adverse cardiac events occurred in 43 patients (8.3%) including 8 cases (1.5%) of cardiac death, 9 cases (1.7%) of MI, 24 cases (4.6%) of target vessel revascularization, and 11 cases (2.1%) of stent thrombosis. Patients with MACE had a higher serum creatinine level, higher incidence of in-stent restenosis lesion, more overlapping stents, a greater number of stents, and longer stents than did patients without MACE. Multivariate analysis revealed that serum creatinine level >1.5 mg/dL {hazard ratio (HR) 2.3, p=0.019}, stent length >33 mm (HR 2.4, p=0.035), and in-stent restenosis lesions (HR 2.4, p=0.040) were independent risk factors for MACE. Patients with DES length >33 mm had a higher incidence of MACE than those with DES length ≤33 mm (HR 2.7, log rank p=0.002).
Drug-eluting stents (DES) have been reported to reduce angiographic restenosis and the need for repeat revascularization.1-4) However, systematic reviews and long-scale registries have observed a similar rate of death and myocardial infarction (MI) in patients treated with either DES or bare-metal stents (BMS) during long-term 5-year follow-up.5-7) In recent times, DES have been widely used in routine clinical practice, including for more complex patients and lesion characteristics, and full lesion coverage has been achieved by using longer stents. However, data regarding the safety and efficacy of such "off-label" use remains limited. Furthermore, there is growing concern regarding the potential risks of late stent thrombosis, especially with off-label use.8)9)
Several clinical, anatomical, and procedural factors have been suggested to be important risk factors for the development of clinical events after DES implantation.6)7)9-11) Clinical events most commonly occur from six to nine months after DES implantation, probably because neointimal growth mainly occurs during the first several months after DES implantation.12) Moreover, recent reports suggest that there may be a "catch-up" phenomenon associated with more progressive delayed late loss in patients with DES implantation.12-14)
Based on these findings, we evaluated the long-term outcomes and predictors of clinical events after off-label use of DES after 1-year follow-up had elapsed.
The studied patients were participants of a prospectively enrolled, single-center, percutaneous coronary intervention (PCI) with a DES cohort. We retrospectively analyzed 1057 consecutive patients who underwent DES implantation between January 2004 and January 2007. Off-label use was defined as DES use in lesion or patient subsets that have not been extensively studied in randomized trials and for which DES does not have Food and Drug Administration approval. This group included patients with ST-segment elevation MI, chronic total occlusions, saphenous vein graft lesions, bifurcation lesions, ostial lesions, left main lesions, in-stent restenotic lesions, small vessels (<2.5 mm), long lesions (>28 mm), and multilesion or multivessel PCI.4)15) On-label use included all other patients.
After 1-year follow-up, we excluded 74 patients who developed major adverse cardiac events (MACE) including all-cause death, non-fatal MI, repeated revascularization at any lesion, 364 patients who underwent on-label use of DES, and 101 patients who had been lost to follow-up within 1 year. Thus, a total of 518 patients were included in this analysis. All patients provided informed consent for their anonymous data to be processed, and the study was approved by the Institutional Review Boards of the hospital.
Stenting was performed according to current clinical practice at the physician's discretion. For all patients, aspirin (300 mg) and clopidogrel (300 mg or 600 mg) were loaded before the procedure. An intra-venous bolus of 5000 U of unfractionated heparin was given, after which additional heparin boluses were administered to maintain an activated clotting time >300 s during the procedure. Platelet glycoprotein IIb/IIIa inhibitors were administered according to operator preference. The occurrence of angiographic complications during PCI was recorded. These included side branch occlusion, slow or no reflow, major dissection, and distal embolization. After the procedure, the patients received 75 mg of clopidogrel for at least six months and aspirin indefinitely. The duration of extended clopidogrel use was determined at the physician's discretion.
Clinical observation was conducted for a median 1179 days (interquartile range 769-1541) after an event-free period of one year had elapsed. At one year after DES implantation, information regarding baseline clinical characteristics and laboratory findings including serum lipid profile, high sensitivity C-reactive protein, and renal function was collected. Clinical data during follow-up period were obtained via regular outpatient visits with intervals of three or six months or by telephone interview.
The endpoint was defined as the occurrence of MACE, including cardiac death, MI, stent thrombosis, and target vessel revascularization. Additionally, individual events including all-cause death, target lesion revascularization, and other non-target vessel revascularization were also recorded. Stent thrombosis was defined using a modified Academic Research Consortium definition of definite or probable stent thrombosis: angiographically documented stent thrombosis, a MI in the distribution of the target vessel, or sudden cardiac death. Death was defined as all-cause mortality during the follow-up period. All deaths were considered cardiac unless an unequivocal noncardiac cause could be established. MI was defined as the presence of at least two of the following: ischemic symptoms, a new elevation of the myocardial band fraction of creatine kinase >3 times the upper limit of normal, and new electrocardiographic changes compatible with MI. Target lesion revascularization was defined as target lesion reintervention inside the implanted stent or within 5 mm proximally or distally by either PCI or bypass surgery. Only the first event was counted as the end point.
Continuous variables are presented as means±standard deviation and were compared with independent t-test. Categorical variables are presented as frequencies or percentages and were compared with chi-square or Fisher's exact test, as appropriate. All analyses were performed using Statistical Package for the Social Sciences (SPSS) 18.0 for Windows (SPSS Inc., Chicago, IL, USA). Variables with a p<0.1 at univariate analysis were entered in a multivariate Cox regression model with a stepping algorithm to identify the independent predictors of MACE. Medication variables were not included, because information regarding medical history during the entire follow-up period was not clear. Cumulative event curves were generated using the Kaplan-Meier method and compared with the log-rank test of significance. All statistical tests were 2-sided, and differences were considered statistically significant at p<0.05.
The study population consisted of 518 patients who underwent DES implantation for off-label indications and did not have MACE during the first year after procedure. The median follow-up duration was 1179 days (interquartile range 769-1541) after a one year event-free period. During the follow-up period, MACE occurred in 43 patients (8.3%) including 8 cases (1.5%) of cardiac death, 9 cases (1.7%) of MI, 24 cases (4.6%) of target vessel revascularization, and 11 cases (2.1%) of stent thrombosis.
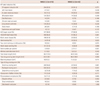
Baseline clinical characteristics at 1 year according to the occurrence of MACE are shown in Table 1. The patients with MACE and without MACE were similar in age, gender, coronary risk factors, and administration of dual antiplatelet therapy. However, patients with MACE had higher serum creatinine levels and a lower incidence of statin medication than did the patients without MACE. The patients with MACE were also more likely to have had a history of MI and previous PCI before the index PCI, compared to those without MACE.
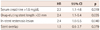
Off-label indications of DES use are shown in Table 2. The incidence of in-stent restenosis lesions was higher in patients with MACE than in the patients without MACE. The patients with MACE underwent more overlapping stenting and had both more stents and longer stents. There was no significant difference between the groups in the type of DES, use of glycoprotein IIb/IIIa inhibitor, and periprocedural complications at the index PCI.
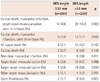
For stepwise multivariate Cox regression analysis, we used a median value for continuous variables. Multivariate analysis showed that serum creatinine >1.5 mg/dL, stent length >33 mm, and in-stent restenosis lesions were independent risk factors for MACE (Table 3). Stent number and lesion length were eliminated by stepwise regression. Therefore, among the procedural variables, total DES length was the only predictor of MACE {hazard ratio (HR) 2.4, 95% confidential interval 1.1-5.4, p=0.035}.
The incidence of MACE according to DES length is shown in Table 4. An increased likelihood of stent thrombosis was observed in patients implanted with >33 mm stent compared to those with shorter DES length (3.4% vs. 1.1%, p=0.073). The incidence of MACE, composite of cardiac death, MI, target vessel revascularization, and stent thrombosis, was higher in patients with longer DES length (12.4% vs. 4.9%, p=0.002).
The cumulative MACE during the follow-up period are presented in Fig. 1. Cardiac death, MI, and the incidence of stent thrombosis were higher in patients with DES length >33 mm compared with those with a DES length ≤33 mm (HR 3.2, log rank p=0.023). Those patients with DES length >33 mm had a higher incidence rate for the overall rate of cardiac death, MI, target vessel revascularization, and stent thrombosis compared with those with DES length ≤33 mm (HR 2.7, log rank p=0.002).
The main findings of our analysis are as follows: 1) after >3 years follow-up, the incidence of MACE remained considerable in a cohort of high-risk patients who underwent DES implantation for off-label indications, with an 8.3% cumulative incidence beyond the 1-year event-free period; 2) although cardiac death, MI, and stent thrombosis were relatively rare events, the incidence of these hard events remained constant throughout the follow-up period; 3) longer stent lengths were significantly associated with a higher risk of MACE (cardiac death, MI, stent thrombosis, and target vessel revascularization) in patients who underwent DES implantation.
Recently, long-term follow-up studies of up to five years after DES implantation have been conducted. A Korean Multicenter Network analysis reported that the proportion of MACE in the first year, as compared to that after 1 year was 45.1% in a sirolimus-eluting stent group and 52.5% in a paclitaxel-eluting stent group.12) The five-year result of the Treatment of De Novo Coronary Disease Using a Single Paclitaxel-Eluting Stent trial showed a target vessel revascularization rate of 16.9% at nine-month and a target vessel revascularization rate of 3.3%/year between 1 and 5 years.6) The long-term results of the Sirolimus-Eluting Stent in Coronary Lesions trial demonstrated that half of target lesion revascularization occurred within the first year during five-year follow-up.16) Furthermore, a five-year follow-up in the A Randomized Controlled Trial of the Medtronic Endeavor Drug (ABT-578) Eluting Coronary Stent System Versus the Cypher Sirolimus-Eluting Coronary Stent System in De Novo Native Coronary Artery Lesions showed that more than 80% of total target lesion revascularization was observed within one year of index revascularization.17) Most clinical events occurred within the first year after DES implantation, because routine angiographic follow-up would increase the rate of revascularization compared with clinically driven follow-up and vascular healing and neointimal growth were delayed after DES implantation compared with BMS implantation, wherein neointimal growth occurred at approximately six months.18) We observed the study population from one year after DES implantation to exclude the influence of routine angiographic follow-up and initial instability of patients' condition. We observed that the risk of both stent thrombosis and target vessel revascularization persisted in patients following the off-label use of DES, even if these adverse events did not develop within the first year.
In contrast to populations enrolled in randomized controlled trials, a large proportion of patients in daily clinical practice receive DES for off-label indications. The off-label use of DES is an independent predictor of stent thrombosis and MACE. The Evaluation of Drug-Eluting Stents and Ischemic Events registry compared outcomes with off-label versus on-label DES use and found a higher rate of target lesion revascularization (6.3% vs. 2.4%), MACE (17.5% vs. 8.9%), and stent thrombosis (1.6% vs. 0.9%) at one year with off-label use.8) The Strategic Transcatheter Evaluation of New Therapies registry also revealed a higher incidence of target vessel revascularization (11.8% vs. 6.5%), death/MI (10.9% vs. 7.9%), and stent thrombosis (1.6% vs. 0.9%) in off-label use of DES than with on-label use at two year follow-up.15) Planer et al.9) reported that 63% of patients underwent sirolimus-eluting stent implantation for off-label indications; such off-label use of DES increased the risk of stent thrombosis by 5.3 times as compared to on-label use of DES at 3.4 years. Most of these studies were limited to short-term follow-up periods, and a large proportion of events occurred within one year, similar to randomized trials involving the on-label use of DES. The added risks for adverse events associated with off-label indications remains unclear. Our results indicate that off-label use was associated with 4.6% of target vessel revascularization, 3.3% of death/MI, and 2.1% of stent thrombosis at more than 3.2 years (median) follow-up, despite 86% of patients continuing to receive dual antiplatelet therapy; moreover, the increased risk attributed to off-label use continues over time in the follow-up period. The most important risk factor for MACE in patients undergoing off-label DES implantation, among clinical variables was serum creatinine level and among procedural variables was the total DES length.
Stent length was found to be a significant predictor of MACE in this study. The Arterial Revascularization Therapy Study Part II analysis showed that total stent length was an independent predictor of stent thrombosis at three years (HR 1.14, p=0.0037).19) Suh et al.20) reported that the total stent length was a strong predictor of stent thrombosis and suggested a stent length ≥31.5 mm as a threshold for stent thrombosis, with a sensitivity of 88.4% and a specificity of 52.1%. Our study also demonstrated that DES length >33 mm was a significant predictor of MACE as well as death/MI/stent thrombosis. Although longer DES appear to be safer and more effective than BMS, data regarding DES length and adverse events are limited. Some studies have reported that long DES reduced the rate of target lesion revascularization compared with BMS, but these data were limited to only a one-year follow-up period.21)22) The present findings reveal an association between stent length and coronary events after DES implantation and should be considered when assessing long-term safety related to DES use.
Spot stenting, i.e., selective stenting of only the most severe stenotic parts of long diffuse lesions has been introduced as an alternative therapy for long lesions in the BMS era.23) Katritsis et al.24) reported that long-term MACE after spot DES stenting was comparable to full coverage of lesion using DES.25) Therefore, intravascular ultrasound or fractional flow reserve-guided stenting would be needed to reduce unnecessarily long DES implantation.
Our study had several limitations. This was not a randomized study. Similar to other observational studies, this study was subject to confounders and biases. The patient group was small, and the event rate was low. Only 43 patients developed MACE; therefore the multivariate analysis was limited. The association between MACE risk and stent length according to the DES type was not evaluated. Furthermore, the lack of intravascular ultrasound data diminished the power of the study to demonstrate the effectiveness of DES procedures.
In conclusion, the risk of both stent thrombosis and target vessel revascularization persisted in patients undergoing DES implantation for off-label indications beyond the first year. Clinical variables, such as the serum creatinine levels, and procedural variables, such as the stent length, along with in-stent restenosis lesions were independent predictors of MACE. A total DES length >33 mm was significantly associated with an increased incidence of death, MI, stent thrombosis, and target vessel revascularization following off-label use of DES.
Figures and Tables
Fig. 1
Event-free survival curves in patients more than 12 months after drug-eluting stent (DES) implantation for off-label indications. HR: hazard ratio, CI: confidence interval.

Table 1
Clinical and laboratory characteristics at 1-year follow-up, according to major adverse cardiac events

MACE: major adverse cardiac events including cardiac death, myocardial infarction (MI), stent thrombosis and target vessel revascularization, PCI: percutaneous coronary intervention, CABG: coronary artery bypass graft surgery, hs-CRP: high sensitivity C-reactive protein, HDL-C: high density lipoprotein-cholesterol, LDL-C: low density lipoprotein-cholesterol, ACE: angiotensin converting enzyme
Table 2
Baseline angiographic and procedural characteristics at index drug-eluting stent implantation
References
1. Babapulle MN, Joseph L, Bélisle P, Brophy JM, Eisenberg MJ. A hierarchical Bayesian meta-analysis of randomised clinical trials of drug-eluting stents. Lancet. 2004. 364:583–591.
2. Moses JW, Leon MB, Popma JJ, et al. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med. 2003. 349:1315–1323.
3. Stone GW, Ellis SG, Cox DA, et al. A polymer-based, paclitaxel-eluting stent in patients with coronary artery disease. N Engl J Med. 2004. 350:221–231.
4. Beohar N, Meyers SN, Erdogan A, et al. Off-label use of drug-eluting versus bare metal stents: a lesion-specific systematic review of long-term outcomes. J Interv Cardiol. 2010. 23:528–545.
5. Serruys PW, Onuma Y, Garg S, et al. 5-year clinical outcomes of the ARTS II (Arterial Revascularization Therapies Study II) of the sirolimus-eluting stent in the treatment of patients with multivessel de novo coronary artery lesions. J Am Coll Cardiol. 2010. 55:1093–1101.
6. Ellis SG, Stone GW, Cox DA, et al. Long-term safety and efficacy with paclitaxel-eluting stents: 5-year final results of the TAXUS IV clinical trial (TAXUS IV-SR: Treatment of De Novo Coronary Disease Using a Single Paclitaxel-Eluting Stent). JACC Cardiovasc Interv. 2009. 2:1248–1259.
7. Caixeta A, Leon MB, Lansky AJ, et al. 5-year clinical outcomes after sirolimus-eluting stent implantation insights from a patient-level pooled analysis of 4 randomized trials comparing sirolimus-eluting stents with bare-metal stents. J Am Coll Cardiol. 2009. 54:894–902.
8. Win HK, Caldera AE, Maresh K, et al. Clinical outcomes and stent thrombosis following off-label use of drug-eluting stents. JAMA. 2007. 297:2001–2009.
9. Planer D, Beyar R, Almagor Y, et al. Long-term (>3 Years) outcome and predictors of clinical events after insertion of sirolimus-eluting stent in one or more native coronary arteries (from the Israeli arm of the e-Cypher registry). Am J Cardiol. 2008. 101:953–959.
10. Dangas GD, Claessen BE, Caixeta A, Sanidas EA, Mintz GS, Mehran R. In-stent restenosis in the drug-eluting stent era. J Am Coll Cardiol. 2010. 56:1897–1907.
11. Lee CW, Park SJ. Predictive factors for restenosis after drug-eluting stent implantation. Korean Circ J. 2007. 37:97–102.
12. Park K, Park KW, Rha SW, et al. Comparison of 5-year clinical outcomes between sirolimus-versus paclitaxel-eluting stent: Korean multicenter network analysis of 9000-patient cohort. Circ Cardiovasc Interv. 2012. 5:174–184.
13. Park KW, Kim CH, Lee HY, et al. Does "late catch-up" exist in drug-eluting stents: insights from a serial quantitative coronary angiography analysis of sirolimus versus paclitaxel-eluting stents. Am Heart J. 2010. 159:446–453.
14. Ko YG, Kim JS, Choi D, et al. Five-year outcomes of sirolimus-eluting versus paclitaxel-eluting stents: a propensity matched study: clinical evidence of late catch-up? Int J Cardiol. 2011. 152:302–306.
15. Brodie BR, Stuckey T, Downey W, et al. Outcomes and complications with off-label use of drug-eluting stents: results from the STENT (Strategic Transcatheter Evaluation of New Therapies) group. JACC Cardiovasc Interv. 2008. 1:405–414.
16. Weisz G, Leon MB, Holmes DR Jr, et al. Five-year follow-up after sirolimus-eluting stent implantation results of the SIRIUS (Sirolimus-Eluting Stent in De-Novo Native Coronary Lesions) Trial. J Am Coll Cardiol. 2009. 53:1488–1497.
17. Kandzari DE, Mauri L, Popma JJ, et al. Late-term clinical outcomes with zotarolimus- and sirolimus-eluting stents. 5-year follow-up of the ENDEAVOR III (A Randomized Controlled Trial of the Medtronic Endeavor Drug [ABT-578] Eluting Coronary Stent System Versus the Cypher Sirolimus-Eluting Coronary Stent System in De Novo Native Coronary Artery Lesions). JACC Cardiovasc Interv. 2011. 4:543–550.
18. Nikol S, Huehns TY, Höfling B. Molecular biology and post-angioplasty restenosis. Atherosclerosis. 1996. 123:17–31.
19. Serruys PW, Daemen J, Morice MC, et al. Three-year follow-up of the ARTS-II# - sirolimus-eluting stents for the treatment of patients with multivessel coronary artery disease. EuroIntervention. 2008. 3:450–459.
20. Suh J, Park DW, Lee JY, et al. The relationship and threshold of stent length with regard to risk of stent thrombosis after drug-eluting stent implantation. JACC Cardiovasc Interv. 2010. 3:383–389.
21. Kim YH, Park SW, Lee SW, et al. Sirolimus-eluting stent versus paclitaxel-eluting stent for patients with long coronary artery disease. Circulation. 2006. 114:2148–2153.
22. Dawkins KD, Grube E, Guagliumi G, et al. Clinical efficacy of polymer-based paclitaxel-eluting stents in the treatment of complex, long coronary artery lesions from a multicenter, randomized trial: support for the use of drug-eluting stents in contemporary clinical practice. Circulation. 2005. 112:3306–3313.
23. Colombo A, De Gregorio J, Moussa I, et al. Intravascular ultrasound-guided percutaneous transluminal coronary angioplasty with provisional spot stenting for treatment of long coronary lesions. J Am Coll Cardiol. 2001. 38:1427–1433.
24. Katritsis DG, Korovesis S, Tzanalaridou E, Giazitzoglou E, Voridis E, Meier B. Comparison of long versus short ("spot") drug-eluting stenting for long coronary stenoses. Am J Cardiol. 2009. 104:786–790.
25. Katritsis DG, Korovesis S, Tzanalaridou E, Giazitzoglou E, Zografos T, Meier B. Spot drug-eluting stenting for long coronary stenoses: long-term results of a randomized clinical study. J Interv Cardiol. 2011. 24:437–441.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download