Abstract
Background and Objectives
The impact of multivessel coronary disease (MVD) with chronic total occlusion (CTO) on one-year mortality in patients with acute myocardial infarction (AMI) is not clearly known. We investigated the impact of MVD with concurrent CTO lesion on one-year mortality in patients with AMI.
Subjects and Methods
We studied 1008 consecutive patients who underwent coronary angiography between November 2005 and December 2008 with a diagnosis of AMI.
Results
Among 1008 patients, 432 patients (43%) had MVD, and 88 patients (8.7%) had CTO lesion. The one-year overall mortality was higher in patients with MVD than in patients with single vessel disease (SVD) (10.2% vs. 5.9%, p=0.012). However, the one-year overall mortality was not significantly higher in patients with CTO lesion than in patients without that lesion (12.5% vs. 7.3%, p=0.080). In multivariate analysis, independent predictors of one-year overall mortality were age older than 65 years {hazard ratio (HR) 2.41, 95% confidence interval (CI): 1.43 to 4.08}, Killip class ≥III (HR 3.59, 95% CI: 2.24 to 5.77), ST-elevation myocardial infarction (HR 2.45, 95% CI: 1.49 to 4.05) and MVD (HR 1.76, 95% CI: 1.07 to 2.89).
The incidence of multivessel disease (MVD) in patients with acute myocardial infarction (AMI) is reported to be 40-50%. The morbidity and mortality are higher in patients with MVD versus single vessel disease (SVD).1-6) Chronic total occlusion (CTO) is commonly found on diagnostic angiography in patients with coronary artery disease.7)8) Recent studies have shown that the effects of MVD on long term mortality are due to the presence of CTO in a noninfarct-related artery.9)10) These findings suggest that CTO lesion in a non-infarct related artery was a modifiable risk factor for mortality after AMI. However, successfully opened CTO lesions were not included in these studies. Therefore, we investigated the impact of MVD with CTO lesion on 12-month mortality in patients with AMI, including successfully opened lesions.
Between November 2005 and December 2008, 1094 patients with a diagnosis of AMI underwent coronary angiogram at Kyungpook National University Hospital in Daegu, Korea. Of these patients, 21 patients who had undergone coronary bypass surgery within 30 days after index hospitalization were excluded from the study. Also excluded were 65 patients who did not provide 12-month clinical follow-up data. Therefore, data on 1008 patients were retrospectively analyzed in this study.
Acute myocardial infarction was defined by the World Health Organization criteria incorporating clincial features, elevated biochemistry markers and electrocardiographic findings.11) ST-segment elevation myocardial infarction (STEMI) was defined as a new ST elevation in ≥2 contiguous leads, measuring >0.2 mV in leads V1 to V3, or 0.1 mV in all other leads. Killip class was defined at admission. Left ventricular ejection fraction (LVEF) was measured by 2-dimensional echocardiogram. MVD was defined as visually assessed ≥70% diameter stenosis of at least one of the non-infarct-related arteries. CTO was defined as total occlusion of an estimated duration of >3 months. Identical angiographic criteria with regard to vessel size (≥2.5 mm) and coronary artery lesion were used to qualify for the presence of MVD and/or a CTO. The duration of the occlusion was estimated from clinical events such as myocardial infarction and sudden onset or worsening of the symptoms or was proven by previous angiography. In patients without a history of angina and with a definite identification of the culprit vessel, associated total occlusion of a non-culprit vessel was considered a chronic occlusion if there was angiographic evidence of filling of the vessel through collaterals. If the duration of the occlusion was uncertain and the investigators had no clear reason to estimate the CTO <3 months, the patient was included.
Primary percutaneous coronary intervention (PCI), thrombolysis, or conservative treatment was used as the initial treatment strategy for patients with STEMI at the discretion of the attending doctor. For patients with non-STEMI (NSTEMI), the initial treatment strategy was early invasive PCI or conservative treatment according to the American College of Cardiology and the American Heart Association guidelines for the management of patients with acute coronary syndrome. Prescription of evidence-based medications was encouraged whenever clinically indicated.
The primary outcome for the present analysis was all-cause 12-month mortality. During the follow-up period, follow-up data were obtained by reviewing medical records and by telephone interview with patients.
Data are expressed as mean±SD for continuous variables and percentages for categorical variables. All comparisons between baseline variables were assessed with the Student's t-test for continuous variables and the Pearson's Chi-square test for categorical variables. Cumulative survival curves were constructed according to the Kaplan-Meier method, and significance of differences between the curves were calculated by log-rank test. Cox proportional- hazards model was used to determine independent predictors of all-cause death. Univariate predictors of 12-month mortality were included in the multivariate cox proportional analysis. Age (≥65 years) was dichotomised for the multivariate analysis. For all analyses, a two-sided p<0.05 was considered statistically significant. Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) version 12.0 (SPSS Inc., Chicago, IL, USA).
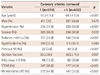
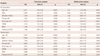
The mean age was 63±11 years, and 698 patients (69%) were men. Among all patients, 432 patients (43%) had MVD. The baseline characteristics of the patients are listed in Table 1. Patients with MVD were older than patients with SVD (64.7±10.6 years vs. 61.5±11.8 years, p<0.001). A history of hypertension or diabetes was more common in patients with MVD than in those with SVD (54.0% vs. 37.5%, p<0.001; 36.4% vs. 22.9%, p<0.001). Previous myocardial infarction (MI) was also more frequent in patients with MVD (9.3% vs. 3.8%, p<0.001). However, the prevalence of smoking was lower in patients with MVD than in those with SVD (60.9% vs. 68.0%, p=0.022). STEMI was more prevalent in patients with SVD (60.5% vs. 41.0%, p<0.001). The LVEF was lower (50.8±11.0% vs. 53.2±9.8%, p=0.001) and Killip class III or IV was more common in patients with MVD than in those with SVD (20.6% vs.12.2%, p=0.001). The left anterior descending artery was the most frequent infarct-related lesion in SVD (47.8%), compared to the right coronary artery in MVD (35.6%). There was no significant difference in gender or the prevalence of hyperlipidemia between the two groups. Twelve-month clinical follow-up outcomes are listed in Table 2. During the 12-month follow-up, 78 patients died (7.7%). The overall mortality in patients with MVD was higher than that in patients with SVD (10.2% vs. 5.9%, p=0.012). The cardiac mortality was also higher in patients with MVD (9.5% vs. 4.7%, p=0.003). Kaplan-Meier survival estimates for 12-month mortality in patients with MVD and SVD are shown in Fig. 1.
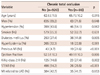
Among the 1008 patients, 88 (8.7%) patients had CTO lesion. CTO PCI was attempted in 60 (68%) patients. Successful opening was obtained in 66% of the attempted cases. Clinical characteristics are presented in Table 3. Patients with CTO lesion were older than patients without CTO lesion (65.7±10.2 years vs. 62.6±11.5 years, p=0.015). A history of diabetes (41.9% vs. 27.4%, p=0.005) or previous MI (21.6% vs. 4.7%, p<0.001) was more common in patients with CTO lesion than in those without that lesion. The frequency of STEMI was lower in patients with CTO lesion (29.5% vs. 54.2%, p<0.001). The LVEF was also lower in patients with CTO lesion (49.1±10.3% vs. 52.5±10.3%, p=0.006). Killip class III or IV was also more common in patients with CTO lesion (27.4% vs. 14.6%, p=0.002). There was no significant difference in gender or the prevalence of hypertension, smoking and hyperlipidemia between the two groups. The frequency of left anterior descending artery as the infarct-related artery was also similar between the two groups.
Twelve-month overall mortality was not significantly higher in patients with CTO lesion than in patients without that lesion (12.5% vs. 7.3%, p=0.080). However, cardiac mortality was higher in patients with CTO lesion (12.5% vs. 6.2%, p=0.024). Kaplan-Meier survival estimates for 12- month mortality in patients with or without CTO are shown in Fig. 2.
To examine the independent prognostic value of CTO, multivariate analysis was performed (Table 4). Independent predictors of one-year overall mortality were: age older than 65 years {hazard ratio (HR) 2.41, 95% confidence interval (CI): 1.43 to 4.08}, Killip class ≥III (HR 3.59, 95% CI: 2.24 to 5.77), STEMI (HR 2.45, 95% CI: 1.49 to 4.05) and MVD (HR 1.76, 95% CI: 1.07 to 2.89). Independent predictors of one-year cardiac death were age older than 65 years (HR 2.50, 95% CI: 1.42 to 4.39), Killip class ≥III (HR 3.55, 95% CI: 2.14 to 5.90), STEMI (HR 3.16, 95% CI: 1.81 to 5.53) and MVD (HR 2.11, 95% CI: 1.23 to 3.61) (Table 4). The presence of CTO was not a significant predictor of one-year mortality or cardiac death.
The purpose of this study was to determine the impact of MVD with CTO on one-year mortality in patients with AMI. Results of the present study are in line with those of a previous study demonstrating that patients with MVD had a higher one-year mortality than SVD patients. There were several differences in the baseline characteristics between patients with and without MVD. Patients with MVD were older and had a more frequent history of diabetes, hypertension or previous MI, and a lower LVEF than SVD patients. Therefore, the mortality difference could be explained by a higher prevalence of associated risk factors in patients with MVD.
In this study, CTO lesion was present in 8% of all study patients and in 20% of patients with MVD. CTO PCI was attempted in 60 (68%) patients. Successful opening was obtained in 66% of the attempted cases. Patients with CTO lesion were older, more often diabetic, and had more unfavorable Killip class compared with patients without that lesion. Of note, STEMI was more frequent in patients without CTO lesion. Among the 88 patients with CTO lesion, there were 11 deaths, all of which were of cardiac origin. We found that the presence of CTO was not a significant predictor of one-year overall mortality and cardiac mortality of AMI patients. These findings are in contrast to the results of van der Schaaf et al.9) They insisted that the presence of a CTO, but not the mere presence of MVD, was an independent predictor of one-year mortality. Moreover, they also evaluated the effects of a concurrent CTO on long-term mortality and left ventricular function.12) They found that the presence of CTO lesion, but not MVD alone, was associated with long-term mortality even when early deaths were excluded from the analysis, and the presence of CTO lesion was associated with reduced LVEF and further deterioration of LVEF. Although the reason for these differences is not clear, the impact of successful revascularization of CTO might have affected the results. In our study, although the number of CTO was small, successful revascularization of CTO was obtained in more than 40% of patients with CTO lesion. It is also known that delayed opening of CTO has beneficial effects on long-term mortality.13-17) The difference in the study populations may be another explanation for the discrepancies in these results. We included not only STEMI, but also NSTEMI.
To the best of our knowledge, the present study is the first study to evaluate the impact of concurrent CTO that was revascularized on 12-month mortality in patients with AMI. A previous study reporting the impact of concurrent CTO on mortality in patients with AMI did not include the CTO lesions that were successfully revascularized.
Our study had several limitations.
First, the number of patients, especially of patients with CTO, was small. Therefore, the statistical power to detect differences in mortality between patients with or without CTO lesion was limited. Second, this study was a retrospective study, not a randomized controlled study. We could not investigate the benefit of opening the concurrent CTO lesion. Selection bias might have occurred in deciding to attempt CTO revascularization. Third, there was a possibility of the inclusion of patients who had the occlusion for less than 3 months.
Patients with MVD have a higher one-year mortality than patients with SVD, which can be explained by a greater prevalence of associated risk factors in patients with MVD. However, the presence of a CTO was not an independent predictor of one-year mortality in AMI patients after including successfully revascularized CTO lesions. A larger patient population in a randomized controlled trial is needed to assess the possible benefit of successful revascularization of concurrent CTO lesion.
Figures and Tables
References
1. O'Keefe JH Jr, Rutherford BD, McConahay DR, et al. Early and late results of coronary angioplasty without antecedent thrombolytic therapy for acute myocardial infarction. Am J Cardiol. 1989. 64:1221–1230.
2. Moreno R, García E, Soriano J, et al. Early coronary angioplasty for acute myocardial infarction: predictors of poor outcome in a non-selected population. J Invasive Cardiol. 2001. 13:202–210.
3. van der Schaaf RJ, Timmer YR, Ottervanger JP, et al. Long-term impact of multivessel disease on cause-specific mortality after ST elevation myocardial infarction treated with reperfusion therapy. Heart. 2006. 92:1760–1763.
4. De Boer MJ, Suryapranata H, Hoorntje JC, et al. Limitation of infarct size and preservation of left ventricular function after primary coronary angioplasty compared with intravenous streptokinase in acute myocardial infarction. Circulation. 1994. 90:753–761.
5. Shihara M, Tsutsui H, Tsuchihashi M, Tada H, Kono S, Takeshita A. Japanese Coronary Invention Study (JCIS) Group. In-hospital and oneyear outcomes for patients undergoing percutaneous coronary intervention for acute myocardial infarction. Am J Cardiol. 2002. 90:932–936.
6. Parodi G, Memisha G, Valenti R, et al. Five year outcome after primary coronary intervention for acute ST elevation myocardial infarction: results from a single centre experience. Heart. 2005. 91:1541–1544.
7. Waldecker B, Wass W, Haberbosch W, Voss R, Heizmann H, Tillmanns H. Long-term follow-up after direct percutaneous transluminal coronary angioplasty for acute myocardial infarction. J Am Coll Cardiol. 1998. 32:1320–1325.
8. Christofferson RD, Lehmann KG, Martin GV, Every N, Caldwell JH, Kapadia SR. Effects of chronic total coronary occlusion on treatment strategy. Am J Cardiol. 2005. 95:1088–1091.
9. van der Schaaf RJ, Vis MM, Sjauw KD, et al. Impact of multivessel coronary disease on long-term mortality in patients with ST-elevation myocardial infarction is due to the presence of a chronic total occlusion. Am J Cardiol. 2006. 98:1165–1169.
10. Claessen BE, Hoebers LP, van der Schaaf RJ, et al. Prevalence and impact of a chronic total occlusion in a non-infarct-related artery on longterm mortality in diabetic patients with ST elevation myocardial infarction. Heart. 2010. 96:1968–1972.
11. French JK, White HD. Clinical implications of the new definition of myocardial infarction. Heart. 2004. 90:99–106.
12. Claessen BE, van der Schaaf RJ, Verouden NJ, et al. Evaluation of the effect of a concurrent chronic total occlusion on long-term mortality and left ventricular function in patients after primary percutaneous coronary intervention. JACC Cardiovasc Interv. 2009. 2:1128–1134.
13. Schömig A, Mehilli J, Antoniucci D, et al. Mechanical reperfusion in patients with acute myocardial infarction presenting more than 12 hours from symptom onset: a randomized controlled trial. JAMA. 2005. 293:2865–2872.
14. Piscione F, Galasso G, De Luca G, et al. Late reopening of an occluded infarct related artery improves left ventricular function and long term clinical outcome. Heart. 2005. 91:646–651.
15. Suero JA, Marso SP, Jones PG, et al. Procedural outcomes and longterm survival among patients undergoing percutaneous coronary intervention of a chronic total occlusion in native coronary arteries: a 20-year experience. J Am Coll Cardiol. 2001. 38:409–414.
16. Hoye A, van Domburg RT, Sonnenschein K, Serruys PW. Percutaneous coronary intervention for chronic total occlusions: the Thoraxcenter experience 1992-2002. Eur Heart J. 2005. 26:2630–2636.
17. Joyal D, Afilalo J, Rinfret S. Effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis. Am Heart J. 2010. 160:179–187.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download