Abstract
Background and Objectives
We hypothesized that fetal echocardiography (echoCG) is an accurate diagnostic tool reflecting well postnatal echoCG findings and outcomes.
Subjects and Methods
We reviewed the medical records of 290 pregnant women, including 313 fetuses, who were examined by fetal echoCG at the Seoul National University Children's Hospital from January 2008 through April 2011.
Results
The mean gestational age at diagnosis was 26.2±5.2 weeks. The mean age of mothers at diagnosis was 31.7±3.8 years. We identified indications for fetal echoCG in 279 cases. The most common indication was abnormal cardiac findings in obstetrical screening sonography (52.0%). Among the 313 echoCG results, 127 (40.6%) were normal, 13 (4.2%) were minor abnormalities, 35 (11.2%) were simple cardiac anomalies, 50 (16.0%) were moderate cardiac anomalies, 60 (19.2%) were complex cardiac anomalies, 16 (5.1%) were arrhythmias, and 12 (3.8%) were twin-to-twin transfusion syndrome. The most common congenital heart disease was tetralogy of Fallot (23 fetuses, 15.9%). One hundred forty-eight neonates were examined by echoCG. We analyzed differences between fetal echoCG and postnatal echoCG. In 131 (88.5%) cases, there was no difference; in 15 (10.1%), there were minor differences; and in only 2 (1.4%) cases, there were major differences.
Congenital heart disease (CHD) is one of the most common congenital anomalies,1)2) and approximately half of infant deaths are due to CHD.3)4) The reported prevalence of moderate and severe CHDs in the United States is about 6 per 1000 live births, and the prevalence of CHDs, including mild forms, is 75 per 1000 live births.5) Recent studies report that the overall prevalence of CHDs is 8.1-18.7 per 1000 live births,4)6)7) and the prevalence of major CHDs (defects requiring intervention during the first year of life) is 3.0-4.4 per 1000 live births.4)8)
Because early detection of CHD makes early medication, transcatheter intervention, or even surgery possible, prenatal diagnosis is considered essential. Use of fetal echocardiography (echoCG) for prenatal diagnosis has increased since it was introduced in 1964.9) Prenatal diagnosis with fetal echoCG has improved the preoperative condition,3)10)11) morbidity,10)12)13) and mortality11)13) of patients with CHD. Fetal echoCG is now widely used in pediatric cardiology and perinatology14) and even for fetal cardiac intervention.10)15)
As a tertiary referral center in South Korea, we aimed to investigate recent trends in the indications of fetal echoCG, postnatal outcomes of CHD, and the discrepancies between pre- and postnatal echoCG. Particularly, we intended to evaluate the reliability of fetal echoCG as a method for prenatal diagnosis.
We searched our database for fetal echoCGs performed at Seoul National University Children's Hospital from January 1, 2008, through April 8, 2011, and reviewed the medical records of these pregnant women and fetuses. The clinical data we collected for this retrospective study were gestational age (GA) at exam, maternal age at exam, indications and results of fetal echoCG, and postnatal courses, including treatments and outcomes.
A total of 313 fetuses of 290 women were examined by fetal echoCG. The difference between the number of women and fetuses is due to twin or triplet pregnancies and examinations in siblings. The mean GA at prenatal diagnosis was 26.2±5.2 weeks. The mean age of mothers at prenatal diagnosis was 31.7±3.8 years. This study was performed after obtaining approval of the Institutional Review Board at our institution (H-1109-050-378). The requirement for informed consent was waived because of the retrospective nature of the study.
We created a classification system for indications based on the indications reported by John and Schowengerdt.14) The two major categories of indications were fetal risks, and maternal or familial risks. We further classified fetal risks into 6 subcategories: abnormal cardiac findings of obstetric screening ultrasonography (USG), abnormal extracardiac findings of obstetric screening USG, arrhythmia, twin-to-twin transfusion syndrome (TTTS), increased nuchal translucency at the first trimester, and other fetal risk (such as hydrops fetalis or twin reversed arterial perfusion syndrome). Maternal or familial risks included 5 subcategories: maternal diabetes mellitus (DM), previous child with CHD diagnosis, parents with CHD diagnosis, maternal systemic lupus erythematosus or lupus nephritis, and other maternal or familial risk (such as another twin pregnancy suspicious for CHD or another twin pregnancy with increased nuchal translucency).
Referring to the grading of the CHDs that Choi et al.16) suggested, we defined 5 classes of fetal echoCG results: normal, minor abnormalities, simple cardiac anomalies, moderate cardiac anomalies, and complex cardiac anomalies. The criteria of these classes are as follows: simple cardiac anomalies are defined as a simple defect or a defect able to be corrected completely by medical treatment, such as ventricular septal defect (VSD), atrial septal defect (ASD), possible coarctation of the aorta (possible CoA). Moderate cardiac anomalies are defects able to be corrected surgically with a low risk for reoperation, such as tetralogy of Fallot (TOF), CoA, atrioventricular septal defect (AVSD), complete transposition of the great arteries (TGA). Complex cardiac anomalies are defined as defects able to be corrected anatomically by surgery but with a high risk for sequelae or a Fontan operation candidate, such as double outlet right ventricle (DORV), TGA with pulmonary stenosis (PS), critical PS, and Fontan candidates {pulmonary atresia with intact ventricular septum (PA with IVS), functional single ventricle (f-SV), hypoplastic left heart syndrome (HLHS)}.
We added 2 more classes for nonstructural anomalies: arrhythmias and TTTS. We gathered the following data for cases in each class: completion of pregnancy (aborted or not aborted), treatments for cardiac problems, and results of cardiac treatments. Thus, we could describe the brief postnatal outcomes of disease for each class of fetal echoCG results, with particular interest in the CHD classes (simple, moderate, and complex cardiac anomalies).
We compared the results of fetal and postnatal echoCG to assess the reliability of fetal echoCG as a method for prenatal diagnosis. Based on Berkley's suggestions, we classified differences as minor or major difference. A minor difference is one that does not result in a change in treatment plan, and a major difference does result in a change in treatment plan.17) If the surgical plan changed significantly, we identified the difference between fetal and postnatal echoCG as a major difference (e.g., if total correction of multiple anomalies was required when a simple defect closure had been planned, or if biventricular repair was planned but a univentricular repair strategy was ultimately adopted).
We used the Statistical Package for the Social Sciences (SPSS), version 19 (SPSS, Inc, an IBM Company, Chicago, IL, USA) and Microsoft office Excel 2007 (Microsoft, Inc., Redmond, WA, USA) for statistical analysis of data. With SPSS, we estimated the mean value of the maternal and GA at fetal echoCG. With Microsoft office Excel 2007, we sorted the data and tabulated frequencies. Data are expressed as means±standard deviation. We rejected null hypotheses of no difference if p were less than 0.05.
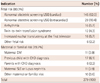
We were able to identify indications for fetal echoCG in 279 cases (Table 1). The most common indication was abnormal cardiac findings of obstetric screening USG (52.0%). The second most common indication was abnormal extracardiac findings of obstetric screening USG (10.4%). Approximately two-thirds of fetal echoCG were due to abnormal findings of obstetric screening USG, which was performed at 18-22 weeks of gestation. Obstetricians were consulted in most cases. Among maternal or familial risks, the most common indication was a previous child with a CHD diagnosis (6.1%).
Among the 313 fetal echoCG results, 127 (40.6%) were normal, 13 (4.2%) were minor abnormalities, 35 (11.2%) were simple cardiac anomalies, 50 (16.0%) were moderate cardiac anomalies, 60 (19.2%) were complex cardiac anomalies, 16 (5.1%) were arrhythmias, and 12 (3.8%) were TTTS. Fetal echoCG results and brief courses of the 7 classes of CHD are summarized in Table 2.
There were 145 diagnoses of CHD (simple, moderate, and complex), and their clinical courses are outlined in Fig. 1. Of 35 fetuses with simple cardiac anomalies, 20 were born at our hospital. One of the 20 neonates expired immediately after delivery because of hydrops fetalis. The other 19 neonates survived after observation (n=14) or operation (4 VSD and 1 bicuspid aortic valve).
Of 50 fetuses with moderate cardiac anomalies, 43 were born at our hospital. Five of these 43 neonates were placed under observation (3 neonates with TOF and 1 neonate with Fallot-type DORV were initially under observation with later surgery planned, when they are stable; the other case was severe PS). One neonate with CoA with left ventricle (LV) and mitral valve hypoplasia was on medical treatment only (the diameter of the isthmus of the aortic arch was acceptable after birth, and we planned to observe his lesion). Four underwent percutaneous interventional treatment only (all of them were severe PS). One case of complete AVSD with TOF was referred to another hospital because there was no bed available for a new admission at the time of delivery. Two of the 43 neonates expired before surgery (1 TOF with bilateral renal agenesis, 1 complete AVSD with stillbirth). Thirty patients were treated surgically; 2 of them, both with complete AVSD, expired after surgery. Twenty-eight of 30 were still alive at the time of this study: 14 cases of TOF, 6 cases of TGA, 4 cases of CoA, 3 cases of complete AVSD, and 1 case of Fallot-type DORV. Of the 30 neonates who underwent surgery for moderate cardiac anomaly, 1 with complete AVSD had a staged operation for univentricular repair and survived. Twenty-seven patients underwent 1-stage repair, and all survived. We were unable to classify 2 surgeries for complete AVSD; both of these patients died.
Thirty-nine of 60 fetuses with complex cardiac anomalies were born at our hospital; pregnancy was aborted in 3 cases. We lost 18 fetuses to follow-up. Of the 39 neonates, 2 were placed on medical treatment only (1 for RV and tricuspid valve hypoplasia, the other for Ebstein anomaly); 1 case of PA with IVS was managed with interventional treatment (balloon pulmonary valvuloplasty) only; 3 expired before surgery (1 f-SV, 1 4-chamber enlargement, and 1 Ebstein anomaly) and 33 underwent operation. Of the 33 neonates who underwent surgery, 23 were living at the time of this study: 3 cases of double inlet LV, 3 cases of PA with IVS, 2 cases of TGA with VSD, 2 cases of HLHS variant, 2 cases of Taussig-Bing anomaly, and 11 cases of other complex CHDs. Ten of 33 who underwent surgery expired postoperatively: 4 cases of HLHS; 2 cases of PA; and 1 case each of f-SV, TOF with PA, TGA, and tricuspid atresia.
Of the 33 neonates who underwent surgery for complex cardiac anomalies, 14 underwent a staged procedure for univentricular repair, and 8 of these survived. Eleven patients underwent 1-stage repair and all survived.
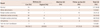
Congenital heart diseases were diagnosed by fetal echoCG in 145 fetuses. The distribution of CHDs diagnosed by fetal echoCG was shown in Table 3. The most common CHD was TOF, including TOF with absent pulmonic valve and TOF with PA (23 cases, 15.9%). The second most common CHD was isolated VSD (19 cases, 13.1%). There were 9 (6.2%) cases each of complete AVSD, TGA and DORV, and 8 (5.5%) cases each of CoA, HLHS, PS (not including critical PS), and PA with IVS. Notably, DORV accounted for only 9 cases, because we counted these separately from biventricular physiology and f-SV with univentricular physiology (6, 4.1%).
For the 313 fetuses that underwent echoCG, 213 neonates were born in our center, and 148 of these underwent echoCG after birth. We compared fetal and postnatal echoCG results. The difference was minor in 10.1%. Major differences resulting in a change of treatment plan, especially surgery, occurred in only 1.4%. Cases with normal prenatal results that were diagnosed as secondary ASD, peripheral PS, PDA, or patent foramen ovale (PFO) after birth were considered to have no difference in prenatal and postnatal echoCG. There were 2 cases with major differences. The first was diagnosed as perimembranous VSD in utero but the postnatal diagnosis was TOF. The second case was diagnosed as TGA with VSD and PS in utero, but the postnatal diagnosis was PA with VSD (the confluent pulmonary artery was present).
Indications for fetal echoCG have changed with time. In the 1990s, the major indications for fetal echoCG were a family history of CHDs, maternal DM, and arrhythmia.18-20) In 2004, Friedberg reported that the most common indication was family history of CHD (23%), and the second most common indication was maternal DM (18%). Obstetrical ultrasound suspicious for CHD accounted for only 13%.19) Similar results were obtained by Meyer-Wittkopf, who reported that the most common indication for fetal echoCG was family history of CHD (44.5%). In the latter study, however, the second most common indication in 2001 was suspected CHD on obstetric scan (25.8%), instead of maternal DM.21) In these 2 studies, abnormal cardiac findings of obstetric screening USG accounted for 18%19) and 25.8%21) of indications, and these increased from 4-5% in the 1990s.18)20) Obstetric screening USG has recently found an even greater prevalence of cardiac abnormalities. Our results show that approximately half of all fetal echoCGs were performed because of abnormal cardiac findings of obstetric screening USG (52.0%). Family history of CHDs, maternal DM, and arrhythmia accounted for only 8.3%, 3.9%, and 5.7% of fetal echoCGs, respectively. The distribution of indications can be expected to differ according to institute and nation. At our tertiary referral center, with a dedicated fetal cardiologist and an obstetrician familiar with fetal echoCG, more than half of fetal echoCGs are now due to abnormal cardiac findings of obstetric screening USG. For the 145 cases diagnosed with CHD by fetal echoCG, 102 neonates were born in our hospital. We lost one-third of those with complex heart diseases and about one-half of those with simple he-art diseases to follow-up. Most with moderate heart diseases were born in our hospital. Regarding complex heart diseases lost to follow-up, pregnancies may have been aborted at other hospitals. In our study, most fetuses with moderate heart disease were born after parental counseling, which shows the importance of counseling after fetal echoCG.
There is a delicate issue involved in evaluating the course of disease in this context. We could not follow-up artificially terminated pregnancies. In South Korea, induced abortion is legal only in cases of hereditary or infectious parental disease as specified by presidential decree, pregnancies due to sexual assault, pregnancies between close relatives, or high-risk pregnancies. In reality, many illegal abortions are performed because of fetal anomalies. In our study, the 3 terminations due to complex CHD were performed in 2008. No pregnancies have been terminated at our hospital since 2009. Many of the pregnancies involving fetuses that were lost to follow-up, especially those with complex heart disease, were probably terminated illegally. This is an important legal and ethical issue in South Korea.
In general, isolated VSD is the most common CHD defect, and ASD is the second most common.4-7) Among cyanotic CHDs, TOF is considered most common.5)6) In our study, however, TOF (15.9%) was the most common CHD, and isolated VSD (13.1%) was the second most common. Because our patients were referred and we performed fetal echoCGs, the distribution of CHDs we observed may differ from the distribution of CHDs in live births. Several studies have reported results similar to ours; the most common CHD diagnosed with prenatal echoCG is not VSD, but TOF19) or HLHS.17)22) To explain this difference, we considered the detection rate of prenatal echoCG for certain CHDs. Zhang et al.4) showed that the prenatal detection rate for major defects (requiring intervention or surgery during the first year of life) is higher than the rate for minor defects (83% vs. 3%, p<0.0001). This may be because the structural anomalies of moderate to complex CHDs can be detected much more easily by fetal echoCG than those of simple CHDs. In particular, secondary ASD, small VSD, and mild PS, which are common in CHDs, are very hard to identify in the fetal period; thus, most of them are diagnosed by postnatal echoCG. Some neonates with normal cardiac findings on fetal echoCG would have minor cardiac abnormalities or mild CHDs.
In our study, of the 148 paired prenatal and postnatal echoCGs, 29 were normal before birth. Of the 29 neonates with normal prenatal results, 17 had CHD: 7 cases of secondary ASD; 3 cases of VSD; 2 cases of isthmus hypoplasia of the aorta; 2 cases of isolate peripheral PS; and 1 case each of PDA, PFO, and RV enlargement. These are minor abnormalities or simple defects that do not require a change in treatment.
Many studies have mentioned discrepancies between prenatal and postnatal echoCG results23-25); however, few articles describe the diagnostic accuracy of fetal echoCG with respect to the frequency of these variations.17)21)26) Only Berkley qualified the degrees of the discrepancy.17) They reported that 3 (5.7%) of 53 paired prenatal and postnatal echoCG reports had minor variations, and 3 (5.7%) had major variations.17) In comparison, we observed a lower rate of major differences, 1.4%, and 10.1% minor differences. We could assume that minor differences are acceptable, because they do not result in a change in treatment plan17) or surgical strategy. If we consider minor differences in diagnosis of CHD to be acceptable, then the diagnostic accuracy of fetal echoCG in our study is 98.6%. This is within the previously reported range of the diagnostic accuracy of fetal echoCG (94.3-99.0%).17)21)26)
The diagnostic accuracy of fetal echoCG performed by a pediatric cardiologist is much higher than the reported diagnostic accuracy of screening USG performed by an obstetrician (59%).21) Thus, it is reasonable for obstetricians to consult with pediatric cardiologists for fetal echoCG if findings of obstetric screening USG are suspicious.
In conclusion, the recent increase in abnormal cardiac findings of obstetric USG screenings that indicate fetal echoCG. Complex or moderate CHD is likely to account for more cases of CHD diagnosed by fetal echoCG at a tertiary referral center. We found that TOF is the most common prenatal CHD diagnosis. Fetal echoCG is still a good, accurate diagnostic method for CHD.
Figures and Tables
Fig. 1
Postnatal outcomes of simple (A), moderate (B), and complex (C) cardiac anomalies on fetal echocardiography. Of 35 fetuses with simple cardiac anomalies, 20 were born at our hospital and 19 neonates survived after observation or operation. Forty-three of 50 fetuses with moderate cardiac anomalies were born at our hospital, 28 were survived after surgery in 30 patients. Thirty-nine of 60 fetuses with complex cardiac anomalies were born at our hospital, 23 were still alive after operation in 33 patients. Obs.: observation, DAB: died after birth, Tf.: transfer, Mx.: medication, Ix.: intervention, Op.: operation, Pre-Op D.: preoperative death, Surv.: survival, Exp.: expired, CHD: congenital heart disease, F/U: follow-up.

Table 3
Congenital heart diseases diagnosed by fetal echocardiography

TOF: tetralogy of Fallot, PV: pulmonary valve, PA: pulmonary atresia, VSD: ventricular septal defect, AVSD: atrioventricular septal defect, TGA: transposition of the great arteries, DORV: double outlet right ventricle, f-SV: functional single ventricle, CoA: coarctation of the aorta, SubAo AS: subvalvar aortic stenosis, HLHS: hypoplastic left heart syndrome, PA with IVS: pulmonary atresia with intact ventricular septum, PS: pulmonary valve stenosis, ASD: atrial septal defect, DILV: double inlet left ventricle, AV: aortic valve, IAA: interruption of the aortic arch
References
1. Lee JE, Jung KL, Kim SE, et al. Prenatal diagnosis of congenital heart disease: trends in pregnancy termination rate, and perinatal and 1-year infant mortalities in Korea between 1994 and 2005. J Obstet Gynaecol Res. 2010. 36:474–478.
2. Tennstedt C, Chaoui R, Körner H, Dietel M. Spectrum of congenital heart defects and extracardiac malformations associated with chromosomal abnormalities: results of a seven year necropsy study. Heart. 1999. 82:34–39.
3. Schultz AH, Localio AR, Clark BJ, Ravishankar C, Videon N, Kimmel SE. Epidemiologic features of the presentation of critical congenital heart disease: implications for screening. Pediatrics. 2008. 121:751–757.
4. Zhang Y, Riehle-Colarusso T, Correa A, et al. Observed prevalence of congenital heart defects from a surveillance study in China. J Ultrasound Med. 2011. 30:989–995.
5. Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002. 39:1890–1900.
6. Reller MD, Strickland MJ, Riehle-Colarusso T, Mahle WT, Correa A. Prevalence of congenital heart defects in metropolitan Atlanta, 1998-2005. J Pediatr. 2008. 153:807–813.
7. Cymbron T, Anjos R, Cabral R, Macedo C, Pereira Duarte C, Mota-Vieira L. Epidemiological characterization of congenital heart disease in São Miguel Island, Azores, Portugal. Community Genet. 2006. 9:107–112.
8. Acharya G, Sitras V, Maltau JM, et al. Major congenital heart disease in Northern Norway: shortcomings of pre- and postnatal diagnosis. Acta Obstet Gynecol Scand. 2004. 83:1124–1129.
9. Friedman AH, Kleinman CS, Copel JA. Diagnosis of cardiac defects: where we've been, where we are and where we're going. Prenat Diagn. 2002. 22:280–284.
10. Feinstein JA, Benson DW, Dubin AM, et al. Hypoplastic left heart syndrome: current considerations and expectations. J Am Coll Cardiol. 2012. 59:1 Suppl. S1–S42.
11. Franklin O, Burch M, Manning N, Sleeman K, Gould S, Archer N. Prenatal diagnosis of coarctation of the aorta improves survival and reduces morbidity. Heart. 2002. 87:67–69.
12. Apitz C, Webb GD, Redington AN. Tetralogy of Fallot. Lancet. 2009. 374:1462–1471.
13. Martins P, Castela E. Transposition of the great arteries. Orphanet J Rare Dis. 2008. 3:27.
14. Jone PN, Schowengerdt KO Jr. Prenatal diagnosis of congenital heart disease. Pediatr Clin North Am. 2009. 56:709–715.
15. Turner CG, Tworetzky W, Wilkins-Haug LE, Jennings RW. Cardiac anomalies in the fetus. Clin Perinatol. 2009. 36:439–449. xi
16. Choi EY, Lee CH, Yoon MJ, et al. Impact of fetal diagnosis of congenital heart disease on parents. Korean J Pediatr. 2006. 49:1073–1078.
17. Berkley EM, Goens MB, Karr S, Rappaport V. Utility of fetal echocardiography in postnatal management of infants with prenatally diagnosed congenital heart disease. Prenat Diagn. 2009. 29:654–658.
18. Smythe JF, Copel JA, Kleinman CS. Outcome of prenatally detected cardiac malformations. Am J Cardiol. 1992. 69:1471–1474.
19. Friedberg MK, Silverman NH. Changing indications for fetal echocardiography in a University Center population. Prenat Diagn. 2004. 24:781–786.
20. Cooper MJ, Enderlein MA, Dyson DC, Rogé CL, Tarnoff H. Fetal echocardiography: retrospective review of clinical experience and an evaluation of indications. Obstet Gynecol. 1995. 86(4 Pt 1):577–582.
21. Meyer-Wittkopf M, Cooper S, Sholler G. Correlation between fetal cardiac diagnosis by obstetric and pediatric cardiologist sonographers and comparison with postnatal findings. Ultrasound Obstet Gynecol. 2001. 17:392–397.
22. Boldt T, Andersson S, Eronen M. Outcome of structural heart disease diagnosed in utero. Scand Cardiovasc J. 2002. 36:73–79.
23. Russo MG, Paladini D, Pacileo G, et al. Changing spectrum and outcome of 705 fetal congenital heart disease cases: 12 years, experience in a third-level center. J Cardiovasc Med (Hagerstown). 2008. 9:910–915.
24. Berg C, Lachmann R, Kaiser C, et al. Prenatal diagnosis of tricuspid atresia: intrauterine course and outcome. Ultrasound Obstet Gynecol. 2010. 35:183–190.
25. Gedikbasi A, Oztarhan K, Gul A, Sargin A, Ceylan Y. Diagnosis and prognosis in double-outlet right ventricle. Am J Perinatol. 2008. 25:427–434.
26. Plesinac S, Terzic M, Stimec B, Plecas D. Value of fetal echocardiography in diagnosis of congenital heart disease in a Serbian university hospital. Int J Fertil Womens Med. 2007. 52:89–92.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download