Abstract
Background and Objectives
In Korea, there hasn't been any previous literature that describes auscultatory blood pressure (BP) normative tables for adolescents. Using BP data, from the Korean National Health and Nutrition Examination Survey (KNHANES), we created normative auscultatory BP percentile tables for Korean adolescents.
Subjects and Methods
A total of 3508 adolescents (boys 1852, girls 1656), aged 10-17 in 2001, 2005 and 2007 from the KNHANES database years, were included. Auscultatory BP measurement was performed, using a Baumanometer Mercury Gravity Sphygmomanometer.
Results
The mean systolic BP of boys was higher than that of girls in adolescents older than 13 years of age, and the mean diastolic BP of boys was higher than that of girls in those older than 15 years. Systolic and diastolic BP was correlated with weight, height and age. Age-specific normative auscultatory systolic and diastolic BP percentiles for boys and girls were completed. The graph that showed age-specific prehypertensive and hypertensive systolic and diastolic BP for boys and girls was presented. For adolescents, the height-specific auscultatory BP percentiles for boys and girls were completed. A graph that shows the height-specific prehypertensive and hypertensive BP for boys and girls was also made.
Until recently, hypertension was considered to be a rare condition in children.1) But most recent large population-based surveys have reported a relatively high prevalence of elevated blood pressure (BP) in children and adolescents of several populations.2)3) The increasing prevalence of hypertension occurred in conjunction with a dramatic increase in the prevalence of overweight and obese children.4) Consensus guidelines recommend that BP should be measured in all children and adolescents at all medical encounters.5) Hypertension in children and adolescents is defined as systolic BP and/or diastolic BP, above the 95th percentile in a population. As such identifying abnormal BP values in children and adolescents need ethnic normative BP values. In Korea, there hasn't been a normative table of auscultatory measured BP until now. We have been using auscultatory BP standards table of the Fourth Report on the Diagnosis, Evaluation and Treatment of High Blood Pressure in Children and Adolescent in the United States.5) However, BP levels differ between different ethnic and geographical populations.6) In Korea, Lee et al.7) reported normative oscillometric BP standards for children and adolescents in 2008. Recently, they also suggested that when comparing BP readings, measured by oscillometers and mercury sphygmomanometers, one has to consider the differences between them, particularly in diastolic blood pressure (DBP), because DBP can be underestimated.8) The oscillometric systolic blood pressure (SBP) averaged 10 mm Hg higher, and the oscillometric diastolic pressure averaged 5 mm Hg higher than the auscultatory BP readings. Therefore, the BP readings by the two methods were not interchangeable.9)10) In a clinical setting, physicians still use mercury sphygmomanometry to measure the BP, although oscillometric devices are being used more frequently. The diagnosis of hypertension in children using the National High blood Pressure Education Program (NHBPEP) method is much more complex than that in adults, as it is based on normative data by age, gender and height percentile, which may not be readily available in many medical care settings.11)
The purpose of this study is to make auscultatory BP standard percentiles for Korean adolescents.
The data were obtained from the Korean National Health and Nutrition Examination Survey, conducted by the Ministry for Health, Welfare and Family Affairs in Korea. A total of 3508 adolescents, aged from 10-17 years in 2001, 2005 and 2007, were selected for this study. Data on height, weight, body mass index (BMI), and auscultatory measured BP (SBP and DBP) were obtained from the Health Examination Survey.
Auscultatory BP measurement was performed, using a Baumanometer Mercury Gravity Sphygmomanometer (W.A. Bauman Co., Copiague, NY, USA), according to the methods recommended by the American Heart Association Task Force.10) BP was measured, while subjects were in a sitting position, following a 5 minutes rest period. BP was measured twice with a mercury sphygmomanometer with a cuff of appropriate size (bladder width at least 40% of arm circumference, length 80-100% of arm circumference) on the right arm and averaged for a final BP reading.
Statistical analyses were performed using SAS (Version 9.22, SAS Institute, Cary, NC) and SUDAAN (Release10.0, Research Triangle Institute, Research Triangle Park, NC), a software package that incorporates sample weights and adjusts analyses for the complex sample design of the survey. The mean and standard deviation were computed for boys and girls, on behalf of a gender difference in BP levels by an analysis of variance, followed by the Bonferroni test for each age group. Statistical significance was accepted at the 5% level. Correlation coefficients were computed between BP levels and anthropometric variables.
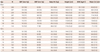
3508 Korean school children (1852 boys and 1656 girls), aged between 10-17 years, were included in this study. The sex and age-specific auscultatory measured mean SBP and DBP, and anthropometric measurements are presented in Table 1. The mean systolic BP of boys was higher than that of girls after 13 years-age and the mean diastolic BP of boys was higher than that of girls after 15 years-age.
Systolic BP correlated most strongly with weight (r=0.475 for boys, p<0.0001; r=0.278 for girls, p<0.0001) and less with BMI (r=0.404 for boys, p<0.0001; r=0.260 for girls, p<0.0001), followed by height (r=0.371 for boys, p<0.0001; r=0.188 for girls, p<0.0001) and age (r=0.32 for boys 6, p<0.0001; r=0.137 for girls, p<0.0001).
Diastolic BP correlated most strongly with weight (r=0.364 for boys, p<0.0001; r=0.271 for girls, p<0.0001) and less with height (r=0.346 for boys, p<0.0001; r=0.263 for girls, p<0.0001), followed by age (r=0.326 for boys, p<0.0001; r=0.262 for girls, p<0.0001) and BMI (r=0.258 for boys, p<0.0001; r=0.2016 for girls, p<0.0001).
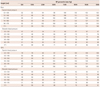
Table 2 showed sex-specific and age-specific normative auscultatory systolic and diastolic BP percentiles. Fig. 1 showed the age-specific prehypertensive (above 90 percentile) and hypertensive (above 95 percentile) systolic and diastolic BP graph for boys and girls. Slopes of systolic and diastolic pressures, according to age in boys were steeper than in girls.
Hypertension in children and adolescents is increasing as the prevalence of the pediatric obesity increases.12)13) It appears that not only the number of children and adolescents with hypertension is increasing, but the actual BP levels may be increasing as well.12)
There are two different ways of presenting BP standards in children. One method presents BP percentile values in a graphic form, according to age, such as those presented by the National Institute of Health Task Force-197714) and Task Force-1988.15) The other method, as recommended by the Working Group of the NHBPEP,16) presents data according to age and height percentiles in a tabular form, without showing the mean values. According to the NHBPEP recommendations, children three years of age or older should have their BP measured during a visit to a medical facility.5) Consensus guidelines define hypertension during childhood as BP that is, on three different visits, measured at or higher than the 95th percentile for age, sex, and height.5) Prehypertension is defined similarly with three or more visits, but as the average BP is at or higher than the 90th percentile for age, sex, and height, or more than 120/80 mm Hg, but less than the 95th percentile.2) Based on these definitions, numerous normal and abnormal cutoffs exist. Diagnosis of hypertension in children is very complicated because abnormal BP values vary with age, sex and height percentile; and therefore, it is difficult to diagnose hypertension or prehypertension in clinics.5)11)17) A few simplified BP tables were developed to facilitate recognition of elevated BP in children.18)19) Those screening tables can quickly and easily identify children and adolescents whose BP readings merit further evaluation by a physician and rule out abnormal BP in children and adolescents.
The BP standards of NHBPEP were made using auscultation methods. Although it is convenient to measure BP using an oscillometric device, the precise method for BP measurement is auscultation, using a mercury manometer device. Oscillometric BP measurement devices are not available at all private pediatric clinics.
Normative BP references for Korean children and adolescents were made, using an oscillometric device measuring BP, and adjusted for height percentiles, gender, and age.7) It is well known that normative BP values differ between the auscultatory and the oscillometric methods. The Dinamap systolic pressures were 8-12 mm Hg higher than the auscultatoy pressures, and the Dinamap diastolic pressures were 4 or 5 mm Hg higher than auscultatory K5 diastolic pressure.9) Our auscultatory normative systolic BP were 5-10 mm Hg lower when compared to the oscillometric BP of the 50th percentile of height in Korean children.7) But auscultatory diastolic BP are 5-10 mm Hg higher than oscillometric normative BP of the 50th percentile of height in Korean children.7) Compared to the oscillometrically measured BP in Chinese children in Hong Kong,20) our auscultatory mean systolic BP is 8 mm Hg lower in boys and 6 mm Hg lower in girls. But, our auscultatory diastolic mean BP is similar to oscillometric BP of Hong Kong Chinese children. This means that our auscultatory measured systolic BP is lower than oscillometric measured BP. However, auscultatory measured diastolic BP is even higher than oscillometric measured BP. Chio et al.21) suggested Dyna-Pulse diastolic was 5 mm Hg lower than that of K4, and is less than 1 mm Hg higher than K5 diastolic in adults. We suggest that our diastolic BP may be measured K4 sound instead of K5 by the auscultation method. By definition, K5 is the pressure at the disappearance of Kortkoff sound. However, in some children, Korotkoff sounds can be heard to 0 mm Hg. Under these circumstances, the BP measurement should be with less pressure on the head of the stethoscope. Only if the very low K5 persists should K4 (muffling of the sounds) be recorded as the diastolic BP.22) Lee et al.8) validated BP measurement with the Dinamap ProCare200 and concluded diastolic BP oscillometric can be underestimated.
Our auscultatory normative BP percentiles for Korean adolescents were adjusted for age. Compared to National Health and Nutrition Examination Survey (NHANES) normative BP data, our auscultatory BP of boys is similar to the BP of the 50th percentile height, but that of girls is lower than the BP of the 50th percentile height. This might be a reflection of genetic differences of the weight and height. We showed that the mean SBP of boys was higher than that of girls after 13 years of age, and that the mean DBP of boys was higher than that of girls after 15 years of age. NHANES data showed SBPs were higher in boys after 14 years old, but DBP of boys were not different from girls.
Our graph of age-specific 90th and 95th percentile SBP and DBP (Fig. 1) makes it easier to diagnose hypertension or prehypertension in adolescents when BP is measured using a mercury sphygomanometry in a clinical setting.
It is known that systolic and diastolic BP correlated most closely with weight, height, age, and BMI.20)23) Our result showed similar correlations. In adolescents, the height and weight may differ up to 20 cm and 30 kg in the same age group. Height and weight are more closely correlated in the pubertal stage than in age and gender. So, we thought that the age-specific normative BP data may have more limitations, especially in adolescents than in children.
Weight is most strongly correlated to BP. Currently, overweight and obese children have become a leading cause of increasing hypertension in children and adolescents. Therefore, the weight-specific normative BP data may have some risk in underdiagnosing hypertension in overweight and obese children and adolescents. For adjusting the limitations of the age-specific normative BP, we suggest the height-specific auscultatory BP percentiles tables are valuable to diagnose hypertension, especially in adolescents. The height-specific 90th and 95th percentile SBP and DBP curves are smoothly increasing, according to height in both girls and boys (Fig. 2). We suggest these graphs are simpler to use as a screening approach for prehypertension and hypertension in Korean adolescents.
The limitation of our study is the method of measuring diastolic pressure. In the case of children and adolescents, K5 diastolic BP could not be heard so we might measure K4 instead of K5. So, diastolic BP is a little higher even compared to oscillometric measured BP.7)9)20)
In conclusion, we provide the auscultatory age-and height-specific BP percentile for Korean adolescents. We present age-specific and height-specific prehypertension and hypertension standards, in graphic forms. These can be useful in screening hypertension of Korean adolescents in a clinical setting.
Figures and Tables
Fig. 1
The 90th and 95th percentile of systolic and diastolic pressures, according to age for boys (A) and girls (B). SBP: systolic blood pressure, DBP: diastolic blood pressure.

Fig. 2
The 90th and 95th percentile of systolic and diastolic blood pressures, according to height for boys (A) and girls (B). SBP: systolic blood pressure, DBP: diastolic blood pressure.

Table 1
Auscultatory measured mean BP (standard deviation) and body measurements in Korean adolescents
References
1. Sinaiko AR. Hypertension in children. N Engl J Med. 1996. 335:1968–1973.
2. Chiolero A, Bovet P, Paradis G, Paccaud F. Has blood pressure increased in children in response to the obesity epidemic? Pediatrics. 2007. 119:544–553.
3. Ippisch HM, Daniels SR. Hypertension in overweight and obese children. Prog Pediatr Cardiol. 2008. 25:177–182.
4. Francischetti EA, Genelhu VA. Obesity-hypertension: an ongoing pandemic. Int J Clin Pract. 2007. 61:269–280.
5. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004. 114:2 Suppl 4th Report. 555–576.
6. Harding S, Maynard M, Cruickshank JK, Gray L. Anthropometry and blood pressure differences in black Caribbean, African, South Asian and white adolescents: the MRC DASH study. J Hypertens. 2006. 24:1507–1514.
7. Lee CG, Moon JS, Choi JM, et al. Normative blood pressure references for Korean children and adolescents. Korean J Pediatr. 2008. 51:33–41.
8. Lee CG, Park HM, Shin HJ, et al. Validation study of the Dinamap Pro-Care 200 upper arm blood pressure monitor in children and adolescents. Korean J Pediatr. 2011. 54:463–469.
9. Park MK, Menard SW, Yuan C. Comparison of auscultatory and oscillometric blood pressures. Arch Pediatr Adolesc Med. 2001. 155:50–53.
10. Recommendations for human blood pressure determination by sphygmomanometers. Circulation. 1988. 77:501A–514A.
11. Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA. 2007. 298:874–879.
12. Flynn JT. Pediatric hypertension update. Curr Opin Nephrol Hypertens. 2010. 19:292–297.
13. Sorof J, Daniels S. Obesity hypertension in children: a problem of epidemic proportions. Hypertension. 2002. 40:441–447.
14. Blumenthal S, Epps RP, Heavenrich R, et al. Report of the task force on blood pressure control in children. Pediatrics. 1977. 59:5 2 suppl. I–II. 797–820.
15. Report of the Second Task Force on Blood Pressure Control in Children--1987. Task Force on Blood Pressure Control in Children. National Heart, Lung, and Blood Institute, Bethesda, Maryland. Pediatrics. 1987. 79:1–25.
16. National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. Update on the 1987 Task Force Report on High Blood Pressure in Children and Adolescents: a working group report from the National High Blood Pressure Education Program. Pediatrics. 1996. 98(4 Pt 1):649–658.
17. Park MK, Menard SW, Schoolfield J. Oscillometric blood pressure standards for children. Pediatr Cardiol. 2005. 26:601–607.
18. Mitchell CK, Theriot JA, Sayat JG, Muchant DG, Franco SM. A simplified table improves the recognition of paediatric hypertension. J Paediatr Child Health. 2011. 47:22–26.
19. Kaelber DC, Pickett F. Simple table to identify children and adolescents needing further evaluation of blood pressure. Pediatrics. 2009. 123:e972–e974.
20. Sung RY, Choi KC, So HK, et al. Oscillometrically measured blood pressure in Hong Kong Chinese children and associations with anthropometric parameters. J Hypertens. 2008. 26:678–684.
21. Chio SS, Urbina EM, Lapointe J, Tsai J, Berenson GS. Korotkoff sound versus oscillometric cuff sphygmomanometers: comparison between auscultatory and DynaPulse blood pressure measurements. J Am Soc Hypertens. 2011. 5:12–20.
22. Londe S, Klitzner TS. Auscultatory blood pressure measurement--effect of pressure on the head of the stethoscope. West J Med. 1984. 141:193–195.
23. Park MK, Menard SW, Yuan C. Comparison of blood pressure in children from three ethnic groups. Am J Cardiol. 2001. 87:1305–1308.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download