1. Fenelon G, Wijns W, Andries E, Brugada P. Tachycardiomyopathy: mechanisms and clinical implications. Pacing Clin Electrophysiol. 1996; 19:95–106. PMID:
8848384.
2. Horenstein MS, Saarel E, Dick M, Karpawich PP. Reversible symptomatic dilated cardiomyopathy in older children and young adolescents due to primary non-sinus supraventricular tachyarrhythmias. Pediatr Cardiol. 2003; 24:274–279. PMID:
12545317.
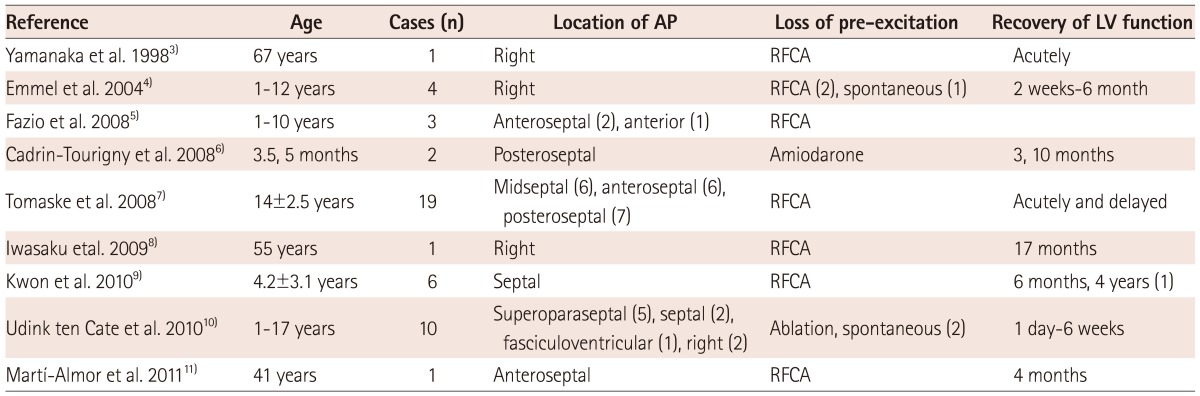
3. Yamanaka S, Shirayama T, Inoue K, Kawata K, Yagi T, Azuma A, et al. Improved cardiac function after catheter ablation in a patient with type B Wolff-Parkinson-White syndrome with an old myocardial infarction. Jpn Circ J. 1998; 62:860–862. PMID:
9856605.
4. Emmel M, Balaji S, Sreeram N. Ventricular preexcitation associated with dilated cardiomyopathy: a causal relationship? Cardiol Young. 2004; 14:594–599. PMID:
15679994.
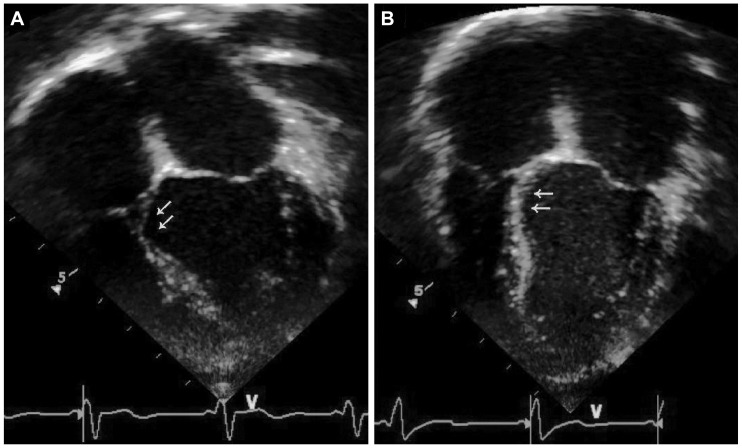
5. Fazio G, Mongiovi' M, Sutera L, Novo G, Novo S, Pipitone S. Segmental dyskinesia in Wolff-Parkinson-White syndrome: a possible cause of dilatative cardiomyopathy. Int J Cardiol. 2008; 123:e31–e34. PMID:
17292982.
6. Cadrin-Tourigny J, Fournier A, Andelfinger G, Khairy P. Severe left ventricular dysfunction in infants with ventricular preexcitation. Heart Rhythm. 2008; 5:1320–1322. PMID:
18774110.
7. Tomaske M, Janousek J, Rázek V, et al. Adverse effects of Wolff-Parkinson-White syndrome with right septal or posteroseptal accessory pathways on cardiac function. Europace. 2008; 10:181–189. PMID:
18256123.
8. Iwasaku T, Hirooka K, Taniguchi T, et al. Successful catheter ablation to accessory atrioventricular pathway as cardiac resynchronization therapy in a patient with dilated cardiomyopathy. Europace. 2009; 11:121–123. PMID:
19028709.
9. Kwon BS, Bae EJ, Kim GB, Noh CI, Choi JY, Yun YS. Septal dyskinesia and global left ventricular dysfunction in pediatric Wolff-Parkinson-White syndrome with septal accessory pathway. J Cardiovasc Electrophysiol. 2010; 21:290–295. PMID:
19804548.
10. Udink ten Cate FE, Kruessell MA, Wagner K, et al. Dilated cardiomyopathy in children with ventricular preexcitation: the location of the accessory pathway is predictive of this association. J Electrocardiol. 2010; 43:146–154. PMID:
19879594.
11. Martí-Almor J, Bazan V, Morales M, Guerra JC. [Heart failure in a patient with Wolff-Parkinson-White syndrome]. Rev Esp Cardiol. 2011; 64:1217–1218. PMID:
21664748.
12. Udink Ten Cate FE, Wiesner N, Trieschmann U, Khalil M, Sreeram N. Dyssynchronous ventricular activation in asymptomatic wolff-Parkinson-white syndrome: a risk factor for development of dilated cardiomyopathy. Indian Pacing Electrophysiol J. 2010; 10:248–256. PMID:
20552060.
13. DeMaria AN, Vera Z, Neumann A, Mason DT. Alterations in ventricular contraction pattern in the Wolff-Parkinson-White syndrome. Detection by echocardiography. Circulation. 1976; 53:249–257. PMID:
1245032.
14. Francis GS, Theroux P, O'Rourke RA, Hagan AD, Johnson AD. An echocardiographic study of interventricular septal motion in the Wolff-Parkinson-White syndrome. Circulation. 1976; 54:174–178. PMID:
181165.
15. Ticzon AR, Damato AN, Caracta AR, Russo G, Foster JR, Lau SH. Interventricular septal motion during preexcitation and normal conduction in Wolff-Parkinson-White syndrome: echocardiographic and electrophysiologic correlation. Am J Cardiol. 1976; 37:840–847. PMID:
1266749.
16. Lebovitz JA, Mandel WJ, Laks MM, Kraus R, Weinstein S. Relationship between the electrical (electrocardiographic) and mechanical (echocardiographic) events in Wolff-Parkinson-White syndrome. Chest. 1977; 71:463–469. PMID:
852320.
17. Grines CL, Bashore TM, Boudoulas H, Olson S, Shafer P, Wooley CF. Functional abnormalities in isolated left bundle branch block. The effect of interventricular asynchrony. Circulation. 1989; 79:845–853. PMID:
2924415.
18. Prinzen FW, Cheriex EC, Delhaas T, et al. Asymmetric thickness of the left ventricular wall resulting from asynchronous electric activation: a study in dogs with ventricular pacing and in patients with left bundle branch block. Am Heart J. 1995; 130:1045–1053. PMID:
7484735.
19. Tantengco MV, Thomas RL, Karpawich PP. Left ventricular dysfunction after long-term right ventricular apical pacing in the young. J Am Coll Cardiol. 2001; 37:2093–2100. PMID:
11419893.
20. Thambo JB, Bordachar P, Garrigue S, et al. Detrimental ventricular remodeling in patients with congenital complete heart block and chronic right ventricular apical pacing. Circulation. 2004; 110:3766–3772. PMID:
15583083.
21. Prinzen FW, Peschar M. Relation between the pacing induced sequence of activation and left ventricular pump function in animals. Pacing Clin Electrophysiol. 2002; 25(4 Pt 1):484–498. PMID:
11991375.
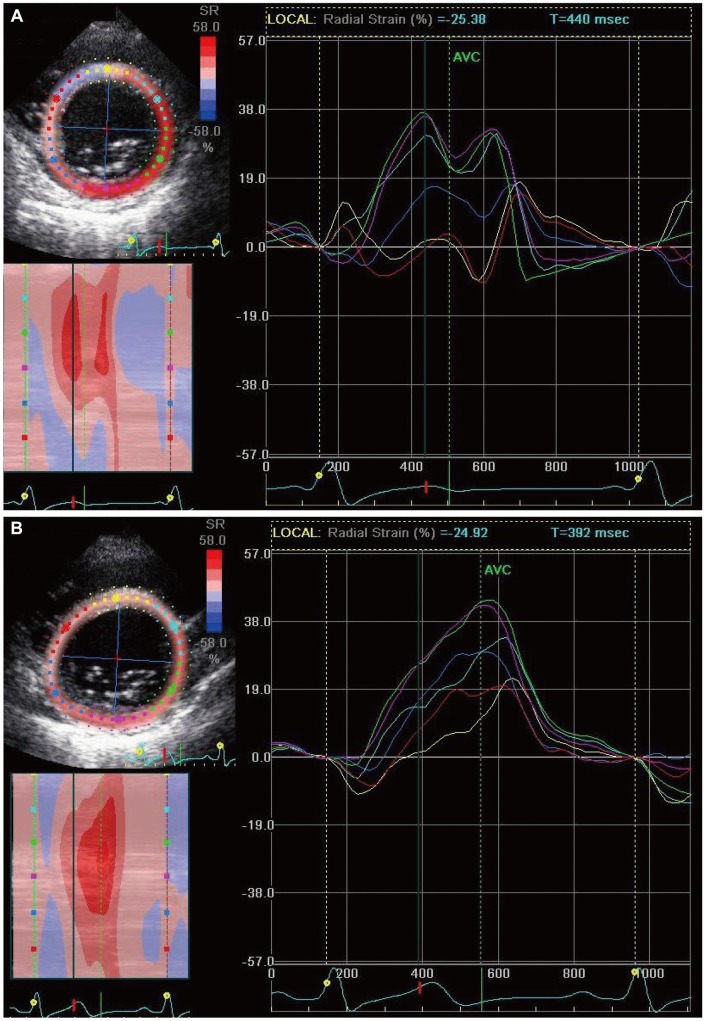
22. De Boeck BW, Teske AJ, Leenders GE, et al. Detection and quantification by deformation imaging of the functional impact of septal compared to free wall preexcitation in the Wolff-Parkinson-White syndrome. Am J Cardiol. 2010; 106:539–546. PMID:
20691313.
23. Kugler JD, Danford DA, Houston KA, Felix G. Pediatric Radiofrequency Ablation Registry of the Pediatric Radiofrequency Ablation Registry of the Pediatric Electrophysiology Society. Pediatric radiofrequency catheter ablation registry success, fluoroscopy time, and complication rate for supraventricular tachycardia: comparison of early and recent eras. J Cardiovasc Electrophysiol. 2002; 13:336–341. PMID:
12033349.
24. Saul JP, Hulse JE, Papagiannis J, Van Praagh R, Walsh EP. Late enlargement of radiofrequency lesions in infant lambs. Implications for ablation procedures in small children. Circulation. 1994; 90:492–499. PMID:
8026036.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download