Abstract
We report a case of coronary-subclavian steal syndrome, which had been masked by a malfunctioning hemodialysis access vessel and then reappeared after a successful angioplasty of multiple stenoses in the arteriovenous fistula of the left arm in a 61-year-old man. This case suggests that coronary-subclavian steal syndrome should be considered before a coronary artery bypass grafting surgery using internal mammary artery conduit is done, especially when hemodialysis using the left arm vessels is expected.
Coronary-subclavian steal syndrome occurs when blood is diverted away from the coronary territory through the internal mammary artery to the upper limb as a result of a significant stenosis or an occlusion of the proximal subclavian artery. In the case we observed, the coronary-subclavian steal syndrome was masked due to a malfunctioning hemodialysis access vessel and recurred after a successful peripheral balloon angioplasty.
A 61-year-old man presented with angina pectoris, which was newly developed after a percutaneous transluminal angioplasty of the arteriovenous fistula (AVF) in his left arm 1 week ago. Four years prior to this, the AVF was formed in his left arm for hemodialysis. Seven years ago, the patient had been diagnosed with three-vessel coronary artery disease and underwent coronary artery bypass grafting, during which his left internal mammary artery was sequentially anastomosed to the mid portion of the left anterior descending artery, ramus intermedius, and the posterior descending branch of the right coronary artery. Six years after surgery, he had been asymptomatic but began experiencing a progressively worsening angina pectoris starting a year ago. The selective coronary angiography at the onset of angina pectoris showed no significant interval changes of the three-vessel coronary artery disease. However, to-and-fro flow was noted in the LIMA (Fig. 1A). The selective left internal mammary angiography showed no stenosis in the anastmotic sites or in the left internal mammary artery itself (Fig. 1B). On the aortography, the left subclavian artery was stenosed at its origin (Fig. 1C). Coronary-subclavian steal syndrome was suspected, and a balloon angioplasty (AVIATOR PLUS, 5.0×20 mm, Cordis, Warren, NJ, USA) followed by stenting (GENESIS 7.0×24 mm, Cordis, Warren, NJ, USA), which was performed successfully (Fig. 1D). Since the stenting of his left subclavian artery, the patient had been asymptomatic for one year. He was referred for a malfunctioning AVF in his left arm one week prior to his latest arrival in our clinic. The arteriovenous fistulogram showed three tight stenosed lesions of the venous outflow tract (Fig. 2A and B). A balloon angioplasty with a plain balloon (REEF HP™, 7×40 mm, Invatec, Roncadelle, Italy) and subsequently a cutting balloon (Peripheral Cutting Balloon®, 7×20 mm, Boston Scientific, Natick, MA, USA) was performed successfully (Fig. 2C and D). After the AVF angioplasty, the function of AVF during hemodialysis was good. However, the patient reported chest discomfort during activity requiring effort and during the hemodialysis. The coronary angiography showed no significant changes compared to what was reported a year ago. Retrograde flow was noted again in the left internal mammary artery (Fig. 3A and B). Aortography revealed that the left subclavian artery was restenosed at its stented position (Fig. 3C). Coronary-subclavian steal syndrome was suspected again, and a balloon angioplasty with peripheral cutting balloon (Peripheral Cutting Balloon®, 8×20 mm, Boston Scientific, Natick, MA, USA) was performed successfully (Fig. 3D). After the balloon angioplasty and instant restenosis of the left subclavian artery, the chest discomfort described by the patient was resolved.
For patients with a previous coronary artery bypass graft operation, during which the left internal mammary artery conduit is used, a great vessel disease, in particular subclavian artery stenosis, should be suspected.1) In the presence of a hemodynamically significant subclavian artery stenosis proximal to the origin of the LIMA, flow through the left internal mammary artery may reverse, and the patient can develop symptoms of angina.2) Subclavian artery stenosis or occlusions, AVFs, and coronary-pulmonary or graft-pulmonary fistulas may cause coronary steal.3-5)
Although the incidence of subclavian stenosis in coronary patients is less than 1% it is of utmost importance to rule out this entity before coronary surgery.6) Coronary-subclavian steal syndrome should be considered before a coronary artery bypass graft operation using the internal mammary artery conduit, especially when hemodialysis using the left arm vessels is expected to prevent additional coronary-subclavian steal syndrome. In the present case, we suspected that the coronary-subclavian steal syndrome had been masked by the stenoses of the hemodialysis access vessel in the patient's left arm and re-appeared after a successful angioplasty, presented as chest discomfort on effort and also during hemodialysis. We related the recurrence of chest pain during hemodialysis to the increase of blood flow to the hemodialysis access vessel due to the resolution of AVF stenoses in the left arm.
Figures and Tables
Fig. 1
Coronary angiography and left subclavian artery angioplasty 1 year prior to clinic admission. A: left coronary angiography demonstrating 'to-and-fro' flow reversal in the left internal mammary artery, suggesting coronary-subclavian steal syndrome. B: selective left internal mammary arteriography showed no significant stenosis of the left internal mammary artery graft itself while its anastomoses to native coronary arteries was demonstrated. C and D: selective left subclavian arteriography revealed a significant stenosis (80%) of the left subclavian artery (arrow) (C), which was resolved after balloon angioplasty with stenting of the left subclavian artery (D).
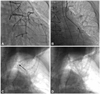
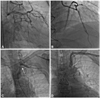
Fig. 2
Arteriovenous fistulogram of left arm 1 week prior to clinic admission. Multiple stenoses of the venous outflow tract (A and B), which resolved after successful balloon angioplasty (C and D), were observed.

Fig. 3
Coronary angiography and left subclavian artery angioplasty on admission. A: left coronary angiography showed 'to-and-fro' flow reversal in the left internal mammary artery, suggesting coronary-subclavian steal syndrome. B: selective left internal mammary arteriography demonstrated that no significant stenosis of the left internal mammary artery graft itself was present and its anastomoses to native coronary arteries was shown. C and D: selective left subclavian arteriography showed a significant instent restenosis (80%) of the left subclavian artery (arrow) (C), which was resolved after balloon angioplasty with peripheral cutting balloon of the left subclavian artery (D).
References
1. Walker PM, Paley D, Harris KA, Thompson A, Johnston KW. What determines the symptoms associated with subclavian artery occlusive disease? J Vasc Surg. 1985. 2:154–157.
2. Smith JM, Koury HI, Hafner CD, Welling RE. Subclavian steal syndrome: a review of 59 consecutive cases. J Cardiovasc Surg (Torino). 1994. 35:11–14.
3. Chavan A, Mügge A, Hohmann C, Amende I, Wahlers T, Galanski M. Recurrent angina pectoris in patients with internal mammary artery to coronary artery bypass: treatment with coil embolization of unligated side branches. Radiology. 1996. 200:433–436.
4. Ayres RW, Lu CT, Benzuly KH, Hill GA, Rossen JD. Transcatheter embolization of an internal mammary artery bypass graft sidebranch causing coronary steal syndrome. Cathet Cardiovasc Diagn. 1994. 31:301–303.
5. Schmid C, Heublein B, Reichelt S, Borst HG. Steal phenomenon caused by a parallel branch of the internal mammary artery. Ann Thorac Surg. 1990. 50:463–464.
6. Takach TJ, Reul GJ, Cooley DA, et al. Myocardial thievery: the coronary-subclavian steal syndrome. Ann Thorac Surg. 2006. 81:386–392.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download