Abstract
Background and Objectives
The renin angiotensin system seems to play an important role in the development of cardiac and vascular hypertrophy in hypertension. The changes in pathology, and gene expressions of the angiotensin II receptor type 1A (ATIA) and angiotensin converting enzyme (ACE) were investigated in order to explore the effects of losartan in spontaneously hypertensive rat (SHR) models.
Materials and Methods
Twelve week-old male Wistar rats were grouped as follows: control (C) group, hypertension (H) group, and losartan (L) group in which SHR was treated with losartan (10 mg/kg/day). Western blot and reverse transcription-polymerase chain reaction analysis regarding seven genes such as endothelin-1, ACE, ATIA, neutrophil cytosolic factor, brain natriuretic peptide, troponin I, endothelial nitric oxide synthase were performed.
Hypertension or elevated arterial blood pressure is a substantial public health issue in industrialized societies. It is a major risk factor in regards to many common causes of morbidity and mortality including stroke, myocardial infarction, congestive heart failure, and end-stage renal disease.1) Although hypertension is linked to many diseases, it's definite causes are still poorly understood. Various factors mediate hypertension. The renin-angiotensin-aldosterone system (RAAS) seems to play a key role in the development of hypertension.2) The principle mediator regarding the physiological actions of the RAAS is the octapeptide angiotensin (QAT).3) There is considerable evidence supporting the involvement for the inappropriately elevated levels of angiotensin (AT) II in many forms of hypertension.4)
Angiotensin II is intimately involved in many regulatory mechanisms in the cardiovascular system beside blood pressure. It stimulates the proliferation of smooth muscle cells (SMCs) in the arterial wall,5) enhances collagen deposition, influences matrix components,6)7) alters structure and thickness of the arterial wall in both resistant as well as conduit arteries, modulates sympathetic activity,8) stimulates endothelin (ET)-1 release from vascular endothelium and tunica adventitia,9) and influences bioavailability of nitric oxide and endothelial functions.10)
Pathological alterations in the majority of these regulatory systems were observed in hypertension. Most of the known AT II effects are mediated via the AT II receptor type 1A (ATIA) and therefore administration of an AT receptor blocker offers the possibility to modify numerous AT II actions within the cardiovascular system.
The spontaneously hypertensive rats (SHR) of the Okamoto-Aoki strain were developed by the selective breeding of Wistar-Kyoto stock for higher blood pressure.11) SHRs spontaneously and consistently develop moderate-to-severe hypertension between 7 and 15 weeks of age and have served as models of genetic hypertension in humans. Several studies were reported in SHR models.12-19)
Losartan is a highly specific, non-peptide antagonist of the AT II receptor type 1.4) AT II receptor antagonists are a group of drugs that are used in the treatment of hypertension. Their mechanism of action involves the specific blockade of AT II receptors, which inhibits vasoconstriction and prevents vascular and cardiac hypertrophy. There have been several articles concerning the effect of losartan in the SHR model.12-19)
The effects were different depending on the dose of losartan. However, there were rare reports with regards to gene changes.
The purpose of this study was to investigate the changes in pathology, and gene expressions of ATIA, and the angiotensin converting enzyme (ACE) in SHR models after losartan treatment.
Twelve-week-old male Wister-Kyoto rats, weighing approximately were used for this study. All rats were housed in climate-controlled conditions with a 12 hours light: 12 hours dark cycle, and had free access to chow and water.
The rats were grouped as follows: control (C) group (n=18), hypertension (H) group (n=18), losartan (L) group (n=18) in which losartan was administrated daily by gavage in a dose of 10 mg/kg/day.
The rats were sacrificed in weeks 3 and 5. The heart and kidney tissues were removed and immediately frozen at -70℃ for protein and gene analysis, post-fixed in 10% formalin, and processed routinely for paraffin embedding. All protocols were approved by the Institutional Animal Care and Use Committees of the School of Medicine of Ewha Womans University (approval No. 11-0169).
The rats were weighed and their general appearance was observed during the study period. The animals were sacrificed at the scheduled time and the hearts and kidneys were rapidly removed. The wet weights of the left ventricle (LV) and kidney were measured, and the ratio of organ weight to body weight (BW) was calculated.
The animals were placed in the supine position and instrumented with an arterial pressure line (Physiological Pressure Transducer, MLT 1199; AD Instruments, Oxfordshire, UK). Arterial pressures were estimated using the input from an ambient-pressure reference (APR-1; Data Sciences) on day 1 in weeks 3 and 5.
LV including the interventricular septum was weighed after the right and left atria and the right ventricular free wall was dissected. The LV mass index was calculated by dividing the LV weight by the BW of each animal. The LV heart tissue was fixed in formaldehyde and embedded as a paraffin section in all three groups. Masson's Trichrome staining was used in order to observe the degree of fibrosis (i.e., degree of collagen penetrating the heart tissue). The area with the most and least degree of fibrosis within each group was selected and photographed under 200 HPF light microscopy. The photographs were processed through an image analysis program (analySIS) and the area of collagen penetration, i.e., the area stained blue with Masson's Trichrome staining was measured.
Total ribonucleic acid (RNA) was extracted by using TRIzol Reagent™ (Invitrogen, Carlsbad, CA, USA), according to the Trizol method protocol and resuspended in diethyl pyrocarbonate water. The final RNA amount was spectrophotometrically determined at 260/280 nm. Quality was assessed as the absence of smear for 18S and 28S bands analyzed by means of Bio analyzer 2100 (Agilent technologies, Palo Alto, CA, USA). RNA samples were stored at -70℃ prior to usage. complementary deoxyribonucleic acid (cDNA) synthesis were synthesized by 1 µg of total RNA, according to the manufacture's protocol (Hight Capacity RNA-to-cDNA kit, Appllied Biosystems, Foster City, CA, USA).20)
Real-time quantitative polymerase chain reaction (PCR) was performed in triplicate in 384-well plates. A 384-well high-throughput analysis was performed by using the ABI Prism 7900 Sequence Detection System Software (Applied Biosystems, Foster City, CA, USA) and white colored 384-well plates (ABgene, Hamburg, Germany) for intensification of the fluorescent signals by a factor of three. The system operated using a thermal cycler and a laser that is directed via fiber optics to each of the 384 sample wells. Fluorescent emissions from each sample were collected by a charge-coupled device-camera and the quantitative data were analyzed using the Sequence Detection System Software (SDS version 2.0, Applied Biosystems, Foster City, CA, USA). Reaction mixtures contained 10 pmol/µL of each primer and 2X SYBR Green PCR Master Mix (Applied Biosystems, Foster City, CA, USA), which included the HotStarTaqt DNA-Polymerase in an optimized buffer, the dNTP mix (with dUTP additive), the SYBRs Green I fluorescent dye, and ROX dye as a passive reference. Each of the 384-well real-time quantitative PCR plates included serial dilutions (1, 1/2 and 1/4) of cDNA, which were used to generate relative standard curves for genes.20)
The resulting first-strand of cDNA normalized by the glyceraldehyde 3-phosphate dehydrogenase (GAPDH) gene. The normalized cDNA was used as a template for the PCR process. The specific primers for rat ET-1 were 5'-TCTCGGAGAG CAGAGACACA-3' (forward) and 5'-TGGACTTTGGA GTTTC TCCCT-3' (reverse).
The specific primers for ACE were 5'-GCC CAC CGA CTC TAC AAC AT-3' (forward) and 5'-ATG GGA CAC TCC TCT GTT GG-3' (reverse).
The specific primers for AT1A were 5'-CTGCGGTGATGTCACTAT GG-3' (forward) and 5'-AAATGTCCTCGTGGTAGGGT-3' (reverse).
The specific primers for neurophil cytosolic factor (NCF) 1were 5'-GGC CAA AGA TGG CAA GAA TA-3' (forward) and 5'-ACC CTT CTC GTA GTC AGC GA-3' (reverse).
All primers were amplified using the same conditions. Thermal cycling conditions included 2 minutes in 50℃, 10 minutes in 95℃, followed by 40 cycles at 95℃ for 30 seconds and 60℃ for 30 seconds, and 72℃ for 30 seconds. In order to exclude the presence of unspecific products, a melting curve analysis regarding the products was performed routinely after finishing amplification through high-resolution data collection during an incremental temperature increase from 60℃ to 95℃ with a ramp rate of 0.21℃/sec. We then converted real-time PCR cycle numbers to gene amounts (ng) according to the equation. The real-time PCR analysis was performed on an Applied Biosystems Prism 7900 Sequence Detection System (PE Applied Biosystems, Foster City, CA, USA).
The tissue was homogenized in a 10 mM Tris HCl buffer, pH 7.4 containing 0.5 mM ethylenediaminetetraacetic acid, pH 8.0, 0.25 M sucrose, 1 mM PMSF, 1 mM Na4VO3 and a protease inhibitor cocktail (Roche-Boehringer-Mannheim). After centrifugation, the supernatant was subjected to sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE). Samples equivalent to 25 µg of protein content were loaded and separated by size in 10% SDS-PAGE. The proteins on the acrylamide gel were transferred to a polyvinylidene difluoride membrane (Millipore, Bedford, MA, USA) at 400 mA in a transfer buffer containing 25 mM Tris and 192 mM glycine, pH 8.4. The peripheral vascular disease membranes were blocked in TBS with 5% non-fat dry milk at room temperature for 1 hour in 0.1% Tween 20 and incubated with the appropriate primary antibodies, including ET-1, ACE, ATIA, NCF, endothelial nitric oxide synthase (eNOS), brain natriuretic peptide (BNP), troponin I (Cell Signaling Technology Inc., Danvers, MA, USA) and GAPDH (Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA) at 4℃ overnight. The membrane was incubated with a horseradish peroxidase-conjugated secondary antibody (Cell Signaling Technology Inc., Danvers, MA, USA) for 1 hour at room temperature. After undergoing washing, the membrane was visualized by a chemiluminescent reaction using an enhanced chemiluminescence-detection kit system (Amersham Biosciences, Buckinghamshire, UK).
The cell lysate from the solubilized tissue was mixed with Pierce BCA reagents (Pierce, Rockford, IL, USA) and incubated for 30 minutes. Moreover, the protein content was quantified with a Molecular Devices enzyme linked immuno sorbent assay reader (Amersham Pharmacia Biotechnology, Sunnyvale, CA, USA) at 562 nm based on the bovine serum albumin standard curve.
Results were expressed as the mean±standard deviation. An unpaired two-tailed t-test and Mann-Whitney test were used, and a p of less than 0.05 was considered statistically significant. Statistical Package for the Social Sciences (SPSS) 12.0 for Windows (SPSS, Chicago, IL, USA) was used for all statistical analyses.
Blood pressure was significantly higher in the H group compared with the C group on day 1 (219.8±10.5 mm Hg vs. 130.7±5.8 mm Hg, p<0.05), in week 3 (211.5±16.1 mm Hg vs. 131.3±7.4 mm Hg, p<0.05), and week 5 (221.2±14.2 mm Hg vs. 175±6.2 mm Hg, p<0.05). Blood pressure was significantly lower in the L group compared with the H group in week 3 (147.7±7.5 mm Hg, p<0.05) and week 5 (139.0±16.9 mm Hg, p<0.05) (Fig. 1).
Body weight was statistically lower in the H group compared with the C group in week 3 (327.7±24.7 g vs. 474.8±12.9 g, p<0.05) and week 5 (320±10.2 g vs. 480±27.2 g, p<0.05).
Left heart (LH) weight was significantly higher in the H group compared with the C group (0.98±0.08 g vs. 0.84±0.01 g, p<0.05) in week 3 and significantly decreased in the L group compared with the H group in week 3 (0.88±0.01 g vs. 0.98±0.08 g, p<0.05).
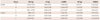
Kidney/BW ratio was significantly higher in the H group compared with the C group in week 5 (0.40±0.02 g vs. 0.32±001 g, p<0.05) and significantly decreased in the L group compared with H group in week 5 (0.37±0.01 vs. 0.40±0.02, p<0.05) (Table 1).
Under light microscopy, collagen was observed to penetrate between the LV myocardiocytes, staining blue as noted in Fig. 2. The degree of penetration was not equally dispersed and differed in each area. Most areas presented little collagen infiltration and these areas were similar in each group. By quantitative analysis, collagen penetration in the H group was significantly higher than that in the C group (1280.8±863.1 vs. 457.1±270.2, p<0.05).
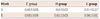
There was no statistically significant difference between the H and the L group but the L group showed a slight decrease in collagen (Table 2).
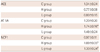
Serum renin levels were significantly higher in the H group compared with the C group in week 3 (9.6±2.3 ng/mL/hr vs. 5.4±1.5 ng/mL/hr, p<0.05) and week 5 (8.0±2.5 ng/mL/hr vs. 4.0±0.9 ng/mL/hr, p<0.05). Also, there was no significant difference between the L and H group (Fig. 3A).
Serum aldosterone levels were significantly higher in the H group compared with the C group in week 5 (78.5±5.3 pg/mL vs. 36.5±9.0 pg/mL, p<0.05) and significantly lower in the L group (65.2±2.8 pg/mL, p<0.05) compared with the H group in week 5 (Fig. 3B).
Serum ACE level did not significantly differ among the three groups (Fig. 3C).
Serum AT levels were significantly higher in the H group compared with the C group on day 1 (1.18±0.23 pg/mL vs. 0.57±0.34 pg/mL, p<0.05), in week 3 (3.66±2.2 pg/mL vs. 0.59±0.18 pg/mL, p<0.05) and week 5 (3.1±1.78 pg/mL vs. 0.52±0.16 pg/mL, p<0.05). In addition, the serum AT level in the L group was significantly lower than that in the H group on day 1 (0.75±0.08 pg/mL in week 3 (0.60±0.2 pg/mL, p<0.05) and week 5 (0.9±0.51 pg/mL, p<0.05) (Fig. 3D).
Serum high sensitive-C reactive protein (hs-CRP) levels were significantly decreased in week 3 in the L group compared with the H group (p<0.05) (Table 3).
Endothelin-1 protein contents were not different among the three groups (Fig. 4A).
Angiotensin converting enzyme protein content was significantly higher in the H group compared with that in the C group in weeks 3 and 5 (p<0.05) and significantly lower in the L group compared with the H group in week 5 (p<0.05) (Fig. 4B).
The ATIA protein level was significantly higher in the H group compared with the C group in weeks 3 and 5 (p<0.05) and significantly lower in the L group compared with the H group in week 5 (p<0.05) (Fig. 4C). NCF 1 protein contents were significantly higher in the H group compared with the C group in weeks 3 and 5 (p<0.05) and significantly lower in the L group compared with the H group in week 5 (p<0.05) (Fig. 4D).
Brain natriuretic peptide and troponin I protein contents were significantly higher in the H group compared with the C group in week 5 (p<0.05) but there was no difference between the H group and the L group. eNOS protein contents were significantly higher in the H group compared with the C group in weeks 3 and 5 (p<0.05), but there was no difference between the H group and the L group (data was not shown).
We demonstrated hypertension-related cardiac changes in the SHR model including left ventricular hypertrophy and LH/BW ratio in week 3, increased BNP and troponin I protein content by western blot analysis in week 5, and increased collagen content by histology.
We initiated this study because the RAAS has an important role in systemic hypertension. Specifically, AT II is a major effector of vasoconstriction, cell growth, sodium and water retention, and sympathetic activation. It appears to promote endothelial dysfunction, inflammation, oxidative stress, insulin resistance, and reduced β-cell responsiveness.21) The close relationship between RAAS and hypertension has led to a compelling indication to block the formation or activity regarding AT II through the use of ACE inhibitors and AT receptor blockers.22) The mechanism by which the AT II receptor type 1 blocker, one of the RAAS metabolites, mediates hypertension seems to be important.
In our SHR model, increased serum renin and aldosterone levels as well as increased protein expression levels for ACE and ATIA were observed, confirming that RAAS has an important role in the SHR.
Increased eNOS protein content was also noted in our SHR model. Hypertension is associated with impaired endothelial function, which can be explained by a decrease in nitric oxide generation or by an enhanced inactivation of NO after its release from the endothelial function.19) AT II stimulates ET-1 release from the vascular endothelium and tunica adventitia9) and influences the bioavailability of NO and endothelial functions.10)
Our study has shown the structural and functional changes of the LV with losartan, an AT II receptor type 1 blocker.
The findings were as follows: In week 1, losartan lowered serum AT levels. In week 3, blood pressure was significantly lowered and LH weight and serum hs-CRP levels also significantly decreased. In week 5, kidney/BW ratio and serum aldosterone levels were significantly decreased. Furthermore, in week 5, NCF gene expressions and protein contents (ACE, ATIA, and NCF) were significantly decreased.
The preventive effect of losartan administration on the enlargement of arterial wall mass may have been reasonably explained by the protective effect of losartan on endothelial cells,23) and inhibition for the proliferative action of AT II on SMCs.24) Tea et al.24) found that the AT2 receptor-mediated vascular mass regression by stimulating SMC apoptosis in vivo, an effect seen during the AT1 receptor blockade. Decreased mass of SMC in the vessel wall may participate in the antihypertensive effect of losartan. Our results revealed several losartan effects in the SHR models.
First, the effect of losartan on decreasing blood pressure appears in week 3 following the onset of losartan treatment. Blood pressure lowering treatments can prevent cardiovascular disease. So, RAAS is targeted by antihypertensive medication such as losartan. The antihypertensive effect differs according to the dose of losartan.
Second, losartan has decreasing effects on LH weight, and kidney/BW ratio in our study. Collagen content was decreased after losartan treatment. Cardiac fibrosis is a detrimental process that causes an imbalance between the extracellular matrix (ECM) deposition and the degradation within the heart resulting in excessive fibroblast proliferation as well as a buildup of ECM proteins within the cardiac interstitial space. As a result, it causes progressive stiffening of the ventricular wall. Fibrosis is associated with hypertension, in addition to congestive heart failure, valvular defects and aging.25) Losartan has beneficial effects on the heart, which affects not only the myocytes but also the production of collagen and other matrix tissues.25)
Third, serum AT levels were significantly decreased following the treatment of losartan from day 1. The aldosterone level decreased as well, leading to decreased water and sodium retention. Actual measurements of serum aldosterone levels showed lower levels in the L group compared to the H group, which is significant in regards to the effects of losartan on aldosterone in the RAAS.
Fourth, down regulated ATIA signifies the inhibition of vasoconstriction, sodium retention, somatic nervous system activation, inflammation, and growth-promoting effects. Protein levels of ACE and ATIA were significantly decreased in the L group compared with the H group. We identified decreased messenger ribonucleic acid (mRNA) levels of NCF1 and serum hs-CRP levels.3) This means that hypertension is speculated to be a response to inflammation. It also suggests that losartan provides an anti inflammatory action.16) A low dose of losartan did not have an effect on ET-1 and eNOS protein content in this study.
In conclusion, losartan has an effect on blood pressure, cardiac hypertrophy, the serum aldosterone level, the mRNA level of ATIA, and the protein level of ACE, ATIA, and NCF.
The most important limitation is that these are data from rats. Also, the physiology and pathology of rats differ from humans. Moreover, the sample size is relatively small. Thus, we plan to research the gene expression levels affected by high doses of losartan treatment.
Figures and Tables
Fig. 1
Systemic blood pressures after losartan treatment. Blood pressure was significantly higher in the H group compared with the C group on day 1, week 3, and week 5. Blood pressure was significantly lower in the L group compared with the H group in weeks 3 and 5. *Significantly different from group C group p<0.05, †Significantly different from group H group p<0.05. C: control, H: hypertension, L: losartan.

Fig. 2
Change of collagen by Masson's Trichrome staining in the heart tissues (×200). Collagen penetration in the H group was significantly higher than that in the C group. There was no statistically significant difference between the H and the L group but the L group showed a slight decrease in collagen. C: control, H: hypertension, L: losartan.

Fig. 3
Serum renin (A), aldosterone (B), ACE (C), angiotensin (D) levels after losartan treatment. *Significantly different from group C group p<0.05, †Significantly different from group H group p<0.05. C: control, H: hypertension, L: losartan.

Fig. 4
Endotehlin-1 (A), ACE (B), angiotensin II receptor type 1A (C), neutrophil cytosolic factor 1 (D) protein contents by western blot analysis in the heart tissues. *Significantly different from group C group p<0.05, †significantly different from group H group p<0.05. ET: endothelin, ACE: angiotensin converting enzyme, AT: angiotensin, NCF: neutrophil cytosolic factor; C: control, H: hypertension, L: losartan.

References
1. Li JJ, Fang CH, Hui RT. Is hypertension an inflammatory disease? Med Hypotheses. 2005. 64:236–240.
2. Schillaci G, Pirro M, Gemelli F, et al. Increased C-reactive protein concentrations in never-treated hypertension: the role of systolic and pulse pressures. J Hypertens. 2003. 21:1841–1846.
3. Efimova O, Szankasi P, Kelley TW. Ncf1 (p47phox) is essential for direct regulatory T cell mediated suppression of CD4+ effector T cells. PLoS One. 2011. 6:e16013.
4. Galzerano D, Capogrosso C, Di Michele S, et al. New standards in hypertension and cardiovascular risk management: focus on telmisartan. Vasc Health Risk Manag. 2010. 6:113–133.
5. Freeman EJ, Ferrario CM, Tallant EA. Angiotensins differentially activate phospholipase D in vascular smooth muscle cells from spontaneously hypertensive and Wistar-Kyoto rats. Am J Hypertens. 1995. 8:1105–1111.
6. López B, González A, Varo N, Laviades C, Querejeta R, Díez J. Biochemical assessment of myocardial fibrosis in hypertensive heart disease. Hypertension. 2001. 38:1222–1226.
7. Rosendorff C. The renin-angiotensin system and vascular hypertrophy. J Am Coll Cardiol. 1996. 28:803–812.
8. Ruiz-Gayo M, Somoza B, Bravo R, Fernández-Alfonso MS, González C. Chronic losartan treatment decreases angiotensin II-mediated facilitation of noradrenaline release in the caudal artery of spontaneously hypertensive rats. Life Sci. 2000. 67:3153–3162.
9. An SJ, Boyd R, Wang Y, Qiu X, Wang HD. Endothelin-1 expression in vascular adventitial fibroblasts. Am J Physiol Heart Circ Physiol. 2006. 290:H700–H708.
10. Yokoyama H, Averill DB, Brosnihan KB, Smith RD, Schiffrin EL, Ferrario CM. Role of blood pressure reduction in prevention of cardiac and vascular hypertrophy. Am J Hypertens. 2005. 18:922–929.
11. Okamoto K, Aoki K. Development of a strain of spontaneously hypertensive rats. Jpn Circ J. 1963. 27:282–293.
12. Koprdova R, Cebova M, Kristek F. Long-term effect of losartan administration on blood pressure, heart and structure of coronary artery of young spontaneously hypertensive rats. Physiol Res. 2009. 58:327–335.
13. Rizzoni D, Porteri E, Piccoli A, et al. Effects of losartan and enalapril on small artery structure in hypertensive rats. Hypertension. 1998. 32:305–310.
14. Zhao LL, Chen HJ, Chen JZ, Yu M, Ni YL, Zhang WF. Losartan reduced connexin43 expression in left ventricular myocardium of spontaneously hypertensive rats. J Zhejiang Univ Sci B. 2008. 9:448–454.
15. Choi SM, Seo MJ, Kang KK, Kim JH, Ahn BO, Yoo M. Beneficial effects of the combination of amlodipine and losartan for lowering blood pressure in spontaneously hypertensive rats. Arch Pharm Res. 2009. 32:353–358.
16. Dai Q, Xu M, Yao M, Sun B. Angiotensin AT1 receptor antagonists exert anti-inflammatory effects in spontaneously hypertensive rats. Br J Pharmacol. 2007. 152:1042–1048.
17. Fortuño MA, Ravassa S, Etayo JC, Díez J. Overexpression of Bax protein and enhanced apoptosis in the left ventricle of spontaneously hypertensive rats: effects of AT1 blockade with losartan. Hypertension. 1998. 32:280–286.
18. Diep QN, El Mabrouk M, Yue P, Schiffrin EL. Effect of AT(1) receptor blockade on cardiac apoptosis in angiotensin II-induced hypertension. Am J Physiol Heart Circ Physiol. 2002. 282:H1635–H1641.
19. Slaninka-Miceska M, Bogdanska J, Korneti P, Kostova E, Jovanoska E, Petrov S. Effect of angiotensin II type 1 (AT1) receptor antagonist on the endothelial dysfunction in spontaneously hypertensive rats in correlation with the nitric oxide system. Bratisl Lek Listy. 2003. 104:342–346.
20. Koo HS, Kim KC, Hong YM. Gene expressions of nitric oxide synthase and matrix metalloproteinase-2 in monocrotaline-induced pulmonary hypertension in rats after bosentan treatment. Korean Circ J. 2011. 41:83–90.
21. Mondry A, Swynghedauw B. Biological adaptation of the myocardium to chronic mechanical overload. Molecular determinants of the autonomic nervous system. Eur Heart J. 1995. 16:Suppl I. 64–73.
22. Ferrario CM. Addressing the theoretical and clinical advantages of combination therapy with inhibitors of the renin-angiotensin-aldosterone system: antihypertensive effects and benefits beyond BP control. Life Sci. 2010. 86:289–299.
23. Garg UC, Hassid A. Nitric oxide-generating vasodilators and 8-bromocyclic guanosine monophosphate inhibit mitogenesis and proliferation of cultured rat vascular smooth muscle cells. J Clin Invest. 1989. 83:1774–1777.
24. Tea BS, Der Sarkissian S, Touyz RM, Hamet P, deBlois D. Proapoptotic and growth-inhibitory role of angiotensin II type 2 receptor in vascular smooth muscle cells of spontaneously hypertensive rats in vivo. Hypertension. 2000. 35:1069–1073.
25. Pellman J, Lyon RC, Sheikh F. Extracellular matrix remodeling in atrial fibrosis: mechanisms and implications in atrial fibrillation. J Mol Cell Cardiol. 2010. 48:461–467.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download