Abstract
Aortic coarctation is usually diagnosed and repaired in childhood and early adulthood. Survival of a patient with an uncorrected coarctation to more than 70 years of age is extremely unusual, and management strategies for these cases remain controversial. We present a case of a 75-year-old woman who was first diagnosed with aortic coarctation and severe aortic valve stenosis 5 years ago and who underwent a successful one-stage repair involving valve replacement and insertion of an extra-anatomical bypass graft from the ascending to the descending aorta.
Aortic coarctation is a congenital cardiovascular malformation that should be diagnosed and corrected early in life.1) Survival of a patient to more than 70 years of age is extremely unusual in cases of uncorrected coarctation. There are a few case reports of patients who were first diagnosed with coarctation at a very late age,2-4) and their management remains controversial. We report a case of a woman who was first diagnosed with coarctation of the aorta at the age of 75 years and underwent a successful total simultaneous repair of coarctation and severe aortic valve stenosis.
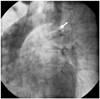
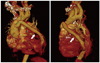
A 75-year-old woman was referred to our emergency room because of squeezing pain in the chest and dyspnea (New York Heart Association Class III). She had a medical history of uncontrolled hypertension for 10 years and was diagnosed with aortic valve stenosis 5 years ago at a local hospital. On physical examination, blood pressure was 170/80 mm Hg in both arms. A systolic ejection murmur was heard at the right upper sternal border. Electrocardiography showed left ventricular hypertrophy and T-wave inversion in the precordial leads. An enlarged cardiac silhouette and rib notching were observed on chest radiography. On echocardiography, severe degenerative aortic valve stenosis, concentric left ventricular hypertrophy and normal left ventricular systolic function were observed. The peak and mean pressure gradient of the aortic valve were estimated at 140 mm Hg and 80 mm Hg, respectively. Therefore, an aortic valve replacement was planned and coronary angiography was performed with aortography for evaluation of chest pain and uncontrolled blood pressure despite antihypertensive drug medication. Coronary angiography revealed normal coronary arteries, while aortography showed severe stenosis of the descending aorta just below the origin of the left subclavian artery (Fig. 1). We suspected aortic coarctation and computed tomographic angiography was performed. Severe aortic coarctation and compensatory dilatation of the intercostal and internal thoracic arteries were noted (Fig. 2). Ankle-Brachial index was 0.53. The blood pressure was 170/80 mm Hg in both upper arms, and 90/60 mm Hg in the lower extremities. The patient underwent a single-stage correction of the coarctation and aortic valve stenosis. After a median sternotomy, cardiopulmonary bypass was established through cannulation of the aortic arch and the right atrium. After retrograde cold blood cardioplegic arrest and incision of the ascending aorta, the calcified bicuspid aortic valve was excised, and a porcine tissue valve prosthesis (21 mm, Hancock II; Medtronic Inc, Minneapolis, MN, USA) was inserted. Afterwards, the supracoronary ascending aorta was anastomosed with a 14 mm polytetrafluoroethylene graft (GORE-TEX vascular graft; W.L Gore & Associates Inc, Flagstaff, AZ, USA) by an end-to-side technique. And then through a posterior pericardial approach, a final end-to-side anastomosis between the bypass graft and the descending aorta completed the repair (Fig. 3). The cardiopulmonary bypass and aortic cross-clamp times were 224 minutes and 163 minutes, respectively. The postoperative course was uneventful. Control of arterial hypertension required minimal doses of angiotensinconverting enzyme inhibitor and β blocker. Warfarin was also prescribed. The patient is doing very well 2 years after discharge.
Aortic coarctation, which is usually diagnosed and corrected early in life, accounts for approximately 9% of all congenital cardiovascular malformations.1) Prognosis of an unrepaired coarctation is very unfavorable. Approximately 90% of cases die before 50 years of age. Another 5% die at 50-60 years and the remaining 5% die at an even older age.2) Death in these patients is usually secondary to heart failure, coronary artery disease, aortic rupture/dissection, concomitant aortic valve disease, infective endarteritis/endocarditis, or cerebral hemorrhage.2)3)
A review of the literature over the past 30 years revealed 10 cases over 70 years of age who were first diagnosed with uncorrected aortic coarctation. Although surgery is considered the treatment of choice for aortic coarctation in children and adults, management strategies for older patients are controversial and there is no consensus on the management of these patients. One patient underwent successful coarctation repair4) and one patient died during surgical repair.5) Two patients underwent coronary artery bypass graft surgery for myocardial ischemia without coarctation repair6)7) and another five patients were conservatively managed for heart failure and hypertension.
Although one might argue that highly developed collateral circulation might allow elderly patients to tolerate the coarctation without its surgical repair,8-12) there are benefits associated with symptomatic improvement and with blood pressure reduction after surgical repair in patients older than 50 years.13) A direct approach to coarctation repair may come across difficulties in the adult population, and a large collateral formation and lung failure after thoracotomy may present technical challenges while total aortic crossclamping, with diminished collaterals, has been involved as a causal factor in paraplegia. For these reasons, extra-anatomic bypass grafting has been used as an alternative surgical option.14)
Severe coarctation of the aorta in combination with intracardiac pathology such as severe valvular stenosis or regurgitation and coronary artery disease in elderly patients requires surgery. The simultaneous operative management of both lesions is desirable because of the higher morbidity and mortality associated with staged procedures, and there has been only one reported case of a patient older than 70 years of age who underwent extra-anatomic bypass and simultaneous correction of intracardiac pathology.14)
We considered coarctation repair surgery because of the highpressure gradient (80 mm Hg) between the ascending and descending aorta and the markedly uncontrolled hypertension despite antihypertensive drugs. Because two-stage procedures for aortic valve replacement and coarctation repair are associated with high rates of perioperative morbidity and mortality, we performed a onestage total simultaneous repair of the coarctation and aortic valve replacement. After surgical intervention, blood pressure was well controlled with minimal doses of antihypertensive medication.
In conclusion, patients with aortic coarctation rarely survive till old age for their first diagnosis. As this case illustrates, simultaneous repair of coarctation of the aorta in combination with an intracardiac pathology can be safely and successfully done even in elderly patients.
Figures and Tables
References
1. Grech V. Diagnostic and surgical trends, and epidemiology of coarctation of the aorta in a population-based study. Int J Cardiol. 1999. 68:197–202.
2. Campbell M. Natural history of coarctation of the aorta. Br Heart J. 1970. 32:633–640.
3. Jenkins NP, Ward C. Coarctation of the aorta: natural history and outcome after surgical treatment. QJM. 1999. 92:365–371.
4. Patel Y, Jilani MI, Cho K. Coarctation of the aorta presenting in a 79-year-old male. Thorac Cardiovasc Surg. 1998. 46:158–160.
5. Liberthson RR, Pennington DG, Jacobs ML, Daggett WM. Coarctation of the aorta: review of 234 patients and clarification of management problems. Am J Cardiol. 1979. 43:835–840.
6. Cevik S, Izgi C, Cevik C. Asymptomatic severe aortic coarctation in an 80-year-old man. Tex Heart Inst J. 2004. 31:429–431.
7. Convens C, Vermeersch P, Paelinck B, Van den Heuvel P, Van den Branden F. Aortic coarctation: a rare and unexpected cause of secondary arterial hypertension in the elderly. Cathet Cardiovasc Diagn. 1996. 39:71–74.
8. Haldane JH. Coarctation of aorta in an elderly man. Can Med Assoc J. 1983. 128:1298–1299.
9. Bartlett LC. Coarctation of the aorta in an elderly man. Can Med Assoc J. 1983. 129:529.
10. O'Byrne E, Mather J, Hargreaves MR. Coarctation of the aorta: an unusual cause of hypertension in a 73-year-old woman. Int J Clin Pract. 1997. 51:466–467.
11. Bobby JJ, Emami JM, Farmer RD, Newman CG. Operative survival and 40-year follow-up of surgical repair of aortic coarctation. Br Heart J. 1991. 65:271–276.
12. Kountouris E, Potsis T, Nikas D, Siogas K. A severe coarctation of aorta in a 72-year-old female: a case report. Cases J. 2009. 2:6308.
13. Bauer M, Alexi-Meskishvili VV, Bauer U, Alfaouri D, Lange PE, Hetzer R. Benefits of surgical repair of coarctation of the aorta in patients older than 50 years. Ann Thorac Surg. 2001. 72:2060–2064.
14. Morris RJ, Samuels LE, Brockman SK. Total simultaneous repair of coarctation and intracardiac pathology in adult patients. Ann Thorac Surg. 1998. 65:1698–1702.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download