Abstract
Diagnosing and selecting an appropriate treatment strategy for left main coronary artery (LMCA) obstruction is very important. Although this disease is not frequently encountered, it can cause severe hemodynamic deterioration resulting in a less favorable prognosis without a suitable management approach. Another aspect of LMCA that we must not overlook is coronary artery spasm, which can be an infrequent but important cause of acute coronary syndrome. Although it is rare, LMCA can cause critical complications. In this study, we report the case of a 35-year-old female who was admitted to the hospital with a diagnosis of acute myocardial infarction with ST-segment elevation in the aVR lead caused by a left main coronary spasm that was examined on intravascular ultrasound.
A ST-segment elevation in the aVR lead has been associated with fixed left main coronary artery (LMCA) lesions in patients with acute coronary syndrome (ACS).1-4) Although acute obstruction of the LMCA is infrequently encountered, predicting an LMCA obstruction is important for selecting the appropriate treatment strategy. Without a suitable management plan, acute LMCA obstruction usually causes severe hemodynamic deterioration resulting in a less favorable prognosis.
Coronary artery spasm is an infrequent but important cause of ACS. Its incidence among patients undergoing diagnostic coronary angiography for suspected ACSs is 3-4%.1) However, a spasm of the LMCA is very rare. In this study, we report the case of a 35-year-old female who was admitted to hospital with a diagnosis of acute myocardial infarction with ST-segment elevation in the aVR lead caused by a left main coronary spasm demonstrated by intravascular ultrasound (IVUS).
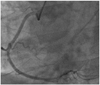
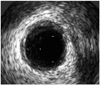
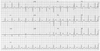
A 35-year-old female presented to our hospital with squeezing chest pain for a duration of 15 minutes. She was a current smoker (20 pack years) without any other risk factors of cardiovascular disease. On physical examination, her blood pressure was 145/80 mm Hg, and pulse rate was 96 beats per minute. Chest radiography showed mild cardiomegaly with mild pulmonary congestion. The initial electrocardiogram (ECG) revealed 2-mm ST segment depression in leads V3-6 and up to a 1-mm ST segment depression in leads I, aVL, II, aVF with a 2-mm ST segment elevation in the aVR lead (Fig. 1). An initial cardiac enzyme profile revealed elevation of creatine phosphokinase (CK), 195 U/L (normal range, 26-174); CK-MB, 49 µg/L (normal range, 0-3); and elevated troponin-I of 3.87 ng/mL (normal range, 0-0.05). Emergency coronary angiography showed a 90% narrowing of the LMCA (Fig. 2A) and a normal right coronary artery without significant narrowing (Fig. 3). During coronary angiography, the patient complained of chest pain with a sudden decrease in systolic blood pressure to 90 mm Hg. However, after administering 100 µg of intracoronary nitrate, the chest pain was relieved and a re-angiography showed a completely resolved LMCA spasm without residual luminal stenosis (Fig. 2B). IVUS showed only a minimal concentric plaque in the LMCA without significant narrowing (Fig. 4). Therefore, we stopped the procedure without intervention. After the procedure, an ST depression in leads I, aVL, II, aVF, and V3-6 and an ST elevation in aVR were completely resolved on the ECG (Fig. 5), and the cardiac enzymes had decreased to the normal range (CK, 41; CK-MB, 22 µg/L; and troponin-I, 1.31 ng/mL). The patient was discharged on the eighth hospital day receiving 40 mg of oral nitrate, 180 mg of diltiazem, 100 mg of aspirin, and 10 mg of rosuvastatin per day. A follow-up coronary angiography taken 9 months later showed no spasms or stenosis. The patient has exhibited no signs of angina for 2 years and has remained on medication in outpatient clinics.
ST-segment elevation in the aVR lead of a patient with clinically suspected ACS suggests a strong possibility of an LMCA obstruction.1)2) In addition to the diagnosis of LMCA obstruction, the finding of ST-segment elevation in the aVR lead also has prognostic significance.6) In a study by Kosuge et al.7) ST-segment elevation >0.5 mm on the aVR lead of an initial ECG and elevated troponin T levels were independent predictors of adverse clinical events at 90 days. According to Barrabés et al.8) ST-segment elevation in the aVR lead at the time of admission is superior to ST-segment depression in other leads for predicting the risk of death in patients with a non-ST-segment elevation acute myocardial infarction.
Coronary artery spasm is an important cause of chest pain and myocardial ischemia. In a prospective study reported by Ong et al.,5) 28% of 488 consecutive patients with ACS had no significant culprit lesions. Among the patients with ACS without any significant fixed stenosis, a coronary vasospasm was documented in nearly 50% of the patients tested with an intracoronary provocation test. Although coronary spasm has been implicated to cause a progression in atherosclerosis over years, few reports9) are available demonstrating a critical role for coronary artery spasm in rapid plaque progression and the development of ACS. It was assumed that a focal spasm may have contributed to rupture an atheromatous plaque, leading eventually to a myocardial infarction. Previous experimental studies have shown that a coronary artery spasm can cause an intraplaque hemorrhage and acute myocardial infarction in a swine model.10) Thus, coronary vasospasm may play an important role in the pathogenesis of not only variant angina but also ACS, as seen in our patient. Wakabayashi et al.11) defined coronary artery spasm as transient total or subtotal occlusion with ECG changes and/or typical chest symptoms. Ong et al.5) defined coronary artery spasm as when quantitative analysis confirms a 75% narrowing (compared with the relaxed state after nitroglycerin), and symptoms are reproduced. Although an ECG during a vasospasm is classically described with an ST elevation, ST depression can also be rarely documented, as in our case. When coronary angiography is normal or shows only nonobstructive plaques, and if a transient ST segment deviation can be demonstrated at the time at which the patient has the discomfort, the presumptive diagnosis of variant angina can be made, and no further tests are necessary. Additionally, a catheter-induced LMCA vasospasm should be meticulously considered.12) In our case, we distinguished a spontaneous spasm from a catheter-induced spam for the following reasons. One, the initial presenting ECG showed an aVR-lead ST segment elevation, which was resolved by intracoronary nitroglycerin. The other reason was the angiographic characteristics of the spasm. Usually, a catheter-induced spasm appears within 1 mm of the catheter tip in contrast to our case (spasm showed irregular and eccentric characteristics and was more than 5 mm from the ostium of the LMCA). IVUS at the time of angiography may help to identify minimal atherosclerotic disease suggesting a vasospasm.
In conclusion, coronary spasm is a frequent cause of ACS and should be regularly considered in the differential diagnosis. It is important not to ignore the aVR lead because it could provide essential diagnostic information in a range of clinical presentations.
Figures and Tables
Fig. 1
Initial electrocardiogram revealed a 2-mm ST segment depression in leads V3-6 and up to a 1-mm ST segment depression in leads I, aVL, II, aVF with a 2-mm ST-segment elevation in the aVR lead (arrows).

Fig. 2
Coronary angiography showing diffuse left main coronary artery vasospasm (A) and resolution of the spasm after administration of intracoronary nitrates (B).

References
1. Kosuge M, Kimura K, Ishikawa T, et al. Predictors of left main or three-vessel disease in patients who have acute coronary syndromes with non-ST-segment elevation. Am J Cardiol. 2005. 95:1366–1369.
2. Duygu H, Yavuzgil O, Erturk U, Zoghi M, Ozerkan F. ST-segment elevation in lead augmented vector right may also be caused by diffuse left main coronary artery vasospasm without fixed stenosis. Clin Cardiol. 2008. 31:179–182.
3. Engelen DJ, Gorgels AP, Cheriex EC, et al. Value of the electrocardiogram in localizing the occlusion site in the left anterior descending coronary artery in acute anterior myocardial infarction. J Am Coll Cardiol. 1999. 34:389–395.
4. Yamaji H, Iwasaki K, Kusachi S, et al. Prediction of acute left main coronary artery obstruction by 12-lead electrocardiography: ST segment elevation in lead aVR with less ST segment elevation in lead V(1). J Am Coll Cardiol. 2001. 38:1348–1354.
5. Ong P, Athanasiadis A, Hill S, Vogelsberg H, Voehringer M, Sechtem U. Coronary artery spasm as a frequent cause of acute coronary syndrome: the CASPAR (Coronary Artery Spasm in Patients with Acute Coronary Syndrome) Study. J Am Coll Cardiol. 2008. 52:523–527.
6. Nikus KC, Eskola MJ. Electrocardiogram patterns in acute left main coronary artery occlusion. J Electrocardiol. 2008. 41:626–629.
7. Kosuge M, Kmura K, Ishikawa T, et al. Combined prognostic utility of ST segment in lead aVR and troponin T on admission in non-ST-segment elevation acute coronary syndrome. Am J Cardiol. 2006. 97:334–339.
8. Barrabés JA, Figureras J, Moure C, Cortadellas J, Soler-Soler J. Prognostic value of lead VR in patients with a first non-ST-segment elevation acute myocardial infarction. Circulation. 2003. 108:814–819.
9. Nobuyoshi M, Tanaka M, Nosaka H, et al. Progression of coronary atherosclerosis: is coronary spasm related to progression? J Am Coll Cardiol. 1991. 18:904–910.
10. Kuga T, Tagawa H, Tomoike H, et al. Role of coronary artery spasm in progression of organic coronary stenosis and acute myocardial infarction in a swine model: importance of mode of onset and duration of coronary artery spasm. Circulation. 1993. 87:573–582.
11. Wakabayashi K, Suzuki H, Honda Y, et al. Provoked coronary spasm predicts adverse outcome in patients with acute myocardial infarction: a novel predictor of prognosis after acute myocardial infarction. J Am Coll Cardiol. 2008. 52:518–522.
12. Edris A, Patel PM, Kern MJ. Early recognition of catheter-induced left main coronary artery vasospasm: implication of revascularization. Catheter Cardiovasc Interv. 2010. 76:304–307.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download