Introduction
Coronary artery ectasia (CAE) is defined as coronary artery dilatation with a diameter of 1.5 times or more than that of the adjacent normal coronary artery.1) But the incidence of multivessel coronary artery aneurysms (MCAA) among patients undergoing coronary artery angiography is very rare.2) As a matter of fact, all three coronary vessels can be affected by CAE, but in almost 75% of patients only an isolated artery is ectatic.3)4) In this report, we present two cases with inferior myocardial infarction which were likely caused by thrombus formation within the CAE and subsequent distal embolization.
Cases
Case 1
A 39 year-old man presented with one hour duration of central chest pain on rest that was associated with diaphoresis. He was a chronic smoker for 29 years and hypertensive for five years. On physical examination, he had a heart rate of 51 beats/min and a blood pressure of 180/100 mm Hg. His chest roentgenogram, pulmonary breath sounds and heart sounds were normal. Electrocardiography showed ST elevations in leads II, III, AVF, and V3R-V5R. Serial cardiac enzymes levels were elevated. Transthoracic echocardiography revealed a left ventricular ejection fraction of 50% and hypokinesia in inferior and right ventricle free walls.
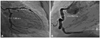
The patient was admitted to the coronary intensive care unit with a diagnosis of acute inferior and right ventricle myocardial infarction. He underwent thrombolytic treatment with streptokinase, and subcutaneous enoxaparin, oral aspirin, clopidogrel, and atorvastatin. His chest pain did not recur following medical therapy in the coronary intensive care unit. Thus, coronary angiography was performed on the same day; segmental ectasia was revealed in all three coronary arteries and total thrombotic occlusion in the midportion of the right coronary arteries (Fig. 1). Renal arteriography was performed because of the presence of hypertension, but it was normal. He refused interventional therapy. Specific laboratory examinations failed to find collagen tissue disease, vasculitis or procoagulant risk factors.
The patient was discharged with medical therapy on the fifth day. He was followed-up for two months and experienced no chest pain.
Case 2
A 52 year-old man presented with intermitent chest pain of two days duration. The pain was initially associated with exertion, but also occurred at rest on the morning that he was admitted to the hospital. He was a chronic smoker and a hypertensive for seven years, and diabetes and hyperlipidemia were newly diagnosed. On a physical examination, he had a heart rate of 96 beats/min and a blood pressure of 100/60 mm Hg. Electrocardiography showed ST elevations in leads II, III, AVF. Serial cardiac enzyme levels were elevated. Transthoracic echocardiography revealed a left ventricular ejection fraction of 55% and hypokinesia in the inferior free wall.
The patient was admitted to the coronary intensive care unit with a diagnosis of acute inferior myocardial infarction. He underwent thrombolytic treatment with streptokinase, and subcutaneous enoxaparin, oral aspirin, clopidogrel, metoprolol and atorvastatin. Coronary angiography revealed segmental ectasia in all three coronary arteries. He had no thrombotic occlusion in all three coronary arteries, probably due to the reperfusion after thrombolytic therapy. But he did have a non-critical lesion in the mid left anterior descending artery (Fig. 2). The patient was discharged with medical therapy on the fourth day.
Discussion
Coronary artery ectasia is defined as coronary artery dilatation with a diameter of 1.5 times or more than that of the adjacent normal coronary artery.1) Several large series of patients undergoing coronary angiography have shown aneurysmal dilatation in 0.15-4.9% of cases.5) But the incidence of MCAA among patients undergoing coronary artery angiography is very rare.2) As a matter of fact, all three coronary vessels can be affected by CAE, but in almost 75% of patients an isolated artery is ectatic.3)4) The proximal and middle segments of the right coronary arteries are the most common sites for CAEs, followed by the proximal left anterior descending and the left circumflex arteries.1)
Coronary artery ectasia is attributed to atherosclerosis in 50% of cases, whereas 20-30% have been considered to be congenital in origin. Only 10% to 20% of cases of CAE have been reported as occurring in association with inflammatory or connective tissue diseases such as scleroderma, in Ehlers-Danlos syndrome, in different types of antineutrophil cytoplasmic antibody-related vasculitis, in syphilitic aortitis, or in Kawasaki disease.6) Our two cases had no clinical history and laboratory tests suggested vasculitis as an underlying disease.
Coronary ectasias may be asymptomatic, or they may be complicated by thrombosis, rupture of the involved segments, and embolism of the intracoronary thrombus to the distal artery tree, producing a small area of infarction.1)7) Our cases presented with inferior myocardial infarction which was likely caused by thrombus formation within the CAE and subsequent distal embolization.
Multivessel coronary artery aneurysms are rare, but can develop in the presence of underlying atherosclerotic vessel disease.8) The diagnosis of MCAA occurs frequently in patients suspected of angina pectoris or myocardial infarction secondary to thrombosis with the aneurysm leading to total occlusion or distal embolization as presented in our cases.4)9) It is one of the less frequent causes of myocardial infarction and management of this angiographic entity requires meticulous medical and interventional therapy.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download