Abstract
Coronary artery spasm is an uncommon, but well recognized, etiology for acute myocardial infarction. However, cardiogenic shock with myocardial infarction resulting from simultaneous multiple coronary artery spasm has been rarely reported, and not in Korea. Recently, we experienced such a case in a 50-year-old Korean man without previous diagnosis of variant angina. The patient, hospitalized for blood sugar control, developed severe chest pain accompanying ST-segment elevation in multiple leads. The patient immediately received cardiac catheterization because of cardiogenic shock. Coronary angiogram revealed the severe and simultaneous spasm of three major epicardial arteries, which was promptly relieved by an intracoronary administration of isosorbide dinitrate. This case highlights the need to rule out the potential mechanism of coronary spasm even in the most severe episodes of acute coronary syndrome.
Coronary artery spasm is usually a transient mechanism for episodes of variant angina, involving single epicardial coronary artery in most cases. However, sometimes coronary artery spasm occurs in more than one artery and it may last much longer than usual angina. Serious cardiac conditions, such as myocardial infarction or malignant arrhythmias, may ensue in proportion to the extent and duration of ischemia. Prolonged coronary artery spasm as an underlying cause for acute myocardial infarction has been recognized1-7) since the possibility was first suggested nearly 50 years ago.8) However, global ischemia induced by simultaneous multiple coronary artery spasm, with clinical presentation of cardiogenic shock, has been rarely reported. Only recently was such a case published for the first time in the English-language literature.9) To our knowledge, a case has never been reported in Korea.
A 50-year-old male was admitted to our hospital for optimal control of blood sugar. The patient had been diabetic for 1 year and was being treated with an oral hypoglycemic agent. A recent blood sugar profile indicated a poorly controlled state, with glycated hemoglobin of 9.6%. The patient had a 30-year smoking history. In the previous month, the patient had been hospitalized via the emergency department to evaluate acute chest pain and minimally elevated serum cardiac troponin I. Coronary angiography conducted under the impression of unstable angina revealed an intermediate lesion at mid-left anterior descending artery (LAD). The patient was treated with medical therapy. On discharge, the patient received a beta-adrenergic blocker and isosorbide dinitrate, but ceased taking the nitrate several days later because of severe headache.
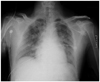
On the 5th hospital day in the morning, the patient developed excruciating chest pain followed by drop of systolic blood pressure to 70 mm Hg. Heart rate was 69 beats/min, and breathing rate was 28/min with 98% oxygen saturation on nasal oxygen (3 L/min). The patient was acutely ill looking, with a pale expression and profuse perspiration. Physical examination revealed fine rales on the bilateral lung field. However, cardiac murmur, friction rub, hepatomegaly, and peripheral edema were not present. An electrocardiogram showed wide QRS complex with right bundle branch block type morphology, and ST-segment elevation in multiple sites including inferior and anteroseptal leads (Fig. 1A). Chest radiography revealed evidence of pulmonary edema in both lung fields (Fig. 2). The patient was first treated with crystalloid fluid resuscitation and an infusion of an inotropic agent (dopamine). Initial assessment of the patient suggested the possibility of cardiogenic shock either from right ventricular infarction complicating acute inferior myocardial infarction or from extensive myocardial infarction due to proximal occlusion of left coronary artery. Because of the profound hemodynamic instability, the patient was immediately transferred for cardiac catheterization. On arrival at the catheterization room, the patient developed ventricular fibrillation (Fig. 1B) and was successfully resuscitated by immediate cardioversion without apparent neurological sequelae. A coronary angiogram revealed a severe spasm of the epicardial arteries, resulting in diffuse and near total occlusion of the proximal right coronary artery (RCA), subtotal occlusion of the left circumflex artery (LCX), and non-occlusive significant narrowing of the proximal LAD (Fig. 3A and B). The coronary lesions were promptly relieved by intracoronary administration of isosorbide dinitrate (Fig. 3C and D) with resolution of the chest pain as well as ST-segment elevation. Vital signs rapidly stabilized. The next day, transthroacic echocardiography revealed regional wall motion abnormality of LAD territory. Serum troponin-I peaked at 22.78 ng/mL and was normalized after 3 days. The patient was treated with amlodipine at a dose of 5 mg per day and with isosorbide dinitrate. Since discharge, the patient has been followed-up regularly in the outpatient clinic without any complaints of chest pain.
Prolonged coronary artery spasm without underlying coronary artery stenosis leading to acute myocardial infarction has been widely reported,10) but to our knowledge, simultaneous multiple coronary artery spasm causing myocardial infarction, cardiogenic shock, and ventricular fibrillation has not been reported in Korea. In the present case, coronary spasm not only involved multiple coronary arteries simultaneously, but also the entire length of each vessel. The extent of myocardial ischemia resulting from those spasms was considered comparable to that of main vessel occlusion. Consequently, the patient developed cardiogenic shock that required fluid resuscitation and inotropic support. Whether the left main coronary artery was also involved during the generalized spasm remains uncertain. However, the range of impaired wall motion involving territory of LAD suggests that infarction had actually developed from prolonged spasmodic occlusion of the vessel. Additional ischemia by severe vasospasm in RCA and LCX might have caused the hemodynamic collapse in the present case.
Clinical presentation of coronary vasospasm is severe but usually benign, because the attack involves a single vessel and resolves spontaneously in most cases. However, coronary spasm can cause life-threatening cardiac events if the spasm is prolonged and/or involves multiple segments of the coronary arterial tree. Fatal complications, such as myocardial infarction or malignant arrhythmia may ensue in proportion to the extent and duration of ischemia. Ventricular fibrillation complicating variant angina can be a life-long risk for sudden cardiac death.13) Nonetheless, the prognosis of patients with myocardial infarction caused by prolonged coronary artery spasm in the absence of significant coronary artery disease appears to be generally good,11)12) if the initial crisis is overcome.
The present case highlights the importance of identifying possible vasospasm for a variety of clinical manifestations of coronary artery disease. The patient was originally diagnosed and treated for unstable angina based on clinical presentations and angiographic finding of coronary stenosis. This case suggests that the previous angiographic lesion had probably arisen from coronary spasm. In the present case, withdrawal of nitrate due to headache might have invoked rebound vasospasm, as suggested in a previous report.1) Subsequent monotherapy with beta-adrenergic blocker could have also adversely influenced vasospasm. Had the diagnosis been made, subsequent dramatic clinical presentation of the multivessel spasm could have been avoided or abated. Furthermore, the administration of positive inotropic agent during the current episode may have actually aggravated the vasospasm, and contributed to the development of ventricular arrhythmia. The risk of developing a serious cardiac event from severe coronary spasm is increased by the low compliance of the patients or overlooking of the physicians. Thus, excluding the possibility of vasospasm is mandatory for every angiographic coronary lesion regardless of the severity of stenosis, even if spasm is not clinically suspected.
Figures and Tables
Fig. 1
Result of electrocardiograms. A: electrocardiogram demonstrating ST-segment elevation in multiple leads and wide QRS widening with right bundle branch block morphology. B: electrocardiogram taken on arrival in the catherization room, showing ventricular fibrillation.

Fig. 3
Results of coronary angiogram. A and B: coronary angiogram showing widespread spasm of the left circumflex artery and left anterior descending artery (A) and right coronary artery (B). C and D: coronary angiogram after intracoronary administration of isosorbide dinitrate showing prompt relief of vasospam in all three coronary arteries.

References
1. Lange RL, Reid MS, Tresch DD, Keelan MH, Bernhard VM, Coolidge G. Nonatheromatous ischemic heart disease following withdrawal from chronic industrial nitroglycerin exposure. Circulation. 1972. 46:666–678.
2. Severi S, Davies G, Maseri A, Marzullo P, L'Abbate A. Long-term prognosis of "variant" angina with medical treatment. Am J Cardiol. 1980. 46:226–232.
3. Waters DD, Szlachcic J, Miller D, Theroux P. Clinical characteristics of pa-tients with variant angina complicated by myocardial infarction or death within 1 month. Am J Cardiol. 1982. 49:658–664.
4. Waters DD, Miller D, Szlachcic J, et al. Factors influencing the long-term prognosis of treated patients with variant angina. Circulation. 1983. 68:258–265.
5. Mark DB, Califf RM, Morris KG, et al. Clinical characteristics and long-term survival of patients with variant angina. Circulation. 1984. 69:880–888.
6. Jeoung JY, Lim DS, Kang JA, et al. The study of coronary spasm by follow-up coronary angiography in variant angina. Korean Circ J. 2002. 32:791–797.
7. Doo YC, Kim JS, Chae KS, et al. Clinical and angiographic characteristics and long-term follow-up in patients with variant angina who presented as acute myocardial infarction. Korean Circ J. 1999. 29:276–284.
8. Leary T. Coronary spasm as a possible factor in producing sudden death. Am Heart J. 1935. 10:338–344.
9. Saito H, Itoh T, Itoh M, Kanaya Y, Suzuki T, Hiramori K. Simultaneous mul-tivessel coronary spasm causing acute myocardial infarction: a case report. Angiology. 2007. 58:112–117.
10. Vincent GM, Anderson JL, Marshall HW. Coronary spasm producing coronary thrombosis and myocardial infarction. N Engl J Med. 1983. 309:220–223.
11. Meisel SR, Mazur A, Chetboun I, et al. Usefulness of implantable cardioverter-defibrillators in refractory variant angina pectoris complicated by ventricular fibrillation in patients with angiographically normal coronary arteries. Am J Cardiol. 2002. 89:1114–1116.
12. Golzio PG, Orzan F, Ferrero P, et al. Myocardial infarction with normal coronary arteries: ten-year follow-up. Ital Heart J. 2004. 5:732–738.
13. Da Costa A, Isaaz K, Faure E, Mourot S, Cerisier A, Lamaud M. Clinical characteristics, aetiological factors and long-term prognosis of myocardial infarction with an absolutely normal coronary angiogram; a 3-year follow-up study of 91 patients. Eur Heart J. 2001. 22:1459–1465.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download