Abstract
Background and Objectives
We checked traditional and high-level precordial electrocardiogram (ECG) leads in patients who had undergone right ventricular outlet obstruction (RVOT) reconstruction surgery and evaluated the effect of ECG lead position on their QRS duration.
Subjects and Methods
We enrolled 34 patients who had undergone surgery for congenital heart disease with RVOT obstruction and who had received followed up care that included recorded ECG at a pediatric cardiac out-patient clinic. The control group included 29 patients who did not have hemodynamically significant intracardiac abnormality. We recorded traditional standard 12-leads ECG from the 4th intercostals space, and moved the precordial leads to the 3rd and 2nd intercostals spaces, and recorded ECGs repeatedly.
Results
In all groups, there was no significant difference of mean QRS duration and QTc interval between traditional standard 12-leads ECGs and ECGs at higher intercostals spaces. There was no significant difference of ECG parameters between groups. In the control group, the degree of the change between the 4th intercostals space (ICS) QRS and 3rd ICS QRS was significant (p=0.031), and although, it was insignificant, ECGs at the 3rd ICS showed decreased QRS duration in group 1 (V1: 3rd ICS 119.21±21.53 msec vs. 4th ICS 122.80±31.78 msec. V2: 3rd ICS 113.68±19.43 msec vs. 4th ICS 118.24±19.16 msec).
Conclusion
Although the positional change of ECG leads did not result in a significant effect on measuring QRS duration after surgery, ECG leads at the 3rd ICS rather than at the 4th ICS may cause alteration of ECG readings. Therefore, we suggest that ECGs should be recorded in as accurate a position as possible.
The electrocardiogram (ECG) is a simple method used to check cardiac condition. Abnormalities of QRS duration, presence of bundle branch blocks, intra-ventricular conduction delay, and ventricular arrhythmias can be detected by the analysis of the QRS complex, which represents ventricular depolarization.
In particular, ECG measurements in patients with congenital heart disease (CHD) can provide several types of information prior to operation and during follow-up after treatment. Surgery to treat right ventricular outlet obstruction (RVOT) can cause an injury to the right bundle branch block (RBBB) and can have an effect on regional delay in systolic activation of the RV wall. In addition, the volume or pressure loading of RV caused by residual pulmonary stenosis (PS) or regurgitation (PR) can result in prolongation of QRS duration and ventricular arrhythmias as long-term outcomes.1-7) Prolonged QRS duration has been recognized as a risk factor for sudden death and right ventricular dysfunction in patients with RVOT reconstruction surgery.6)8-10) Therefore, early detection of significantly prolonged QRS duration is helpful in avoiding life-threatening ventricular arrhythmias.
The previous study demonstrated that the electrodes for ECGs must be positioned at predefined anatomical landmarks because some ECGs recorded by incorrect electrode positions could cause a misdiagnosis of a pathology.11)12)
In the present study, we checked traditional and high-level precordial ECG leads in patients with RVOT reconstruction surgery and evaluated the effect of ECG lead position on their QRS duration.
A total of 34 patients were enrolled in this study. These patients visited the pediatric cardiac clinic at Kyungpook National University Hospital for follow-up care, and ECG recordings were performed. The patients were divided into 2 groups. Group 1 was composed of 19 patients who had received a trans-annular incision and right ventriculotomy for RVOT obstructive disease, such as tetralogy of Fallot (TOF), severe PS, and pulmonary atresia with intact ventricular septum. These patients had mild PS and/or PR with or without pulmonary valve replacement and findings determined that they did not need additional surgical correction. Group 2 was composed of 15 patients, whom we selected by the following criteria: 1) patients who had simple ventricular septal defect (VSD) and initial normal QRS duration on preoperative ECG, and 2) had undergone a right atrium (RA) or main pulmonary artery (PA) incision for correction and whose results revealed complete RBBB on postoperative ECG. Among group 2, none of the patients had significant residual shunt, valve problems and ventricular dysfunction on echocardiographic examination in the postoperative period. The control group included 29 children who met the following conditions: lack of a definite intracardiac abnormality, which was confirmed by 2D-echocardiagraphy or by the presence of a popular left to right shunt lesion {atrial septal defect (ASD), VSD, and patent ductus arteriosus (PDA)} in which the shunt was small and considered to be insignificant. They showed normal QRS duration, and we excluded cases of congenital RBBB.
The 6 precordial leads (V 1-6) and 6 limb leads (I, II, III, aVR, aVL, aVF) of the standard 12-leads were recorded in the supine position. Further, the V 1-2 leads of the high-level intercostals space (HICS) ECGs were recorded in the supine position. For HICS-ECG, the precordial leads (V 1 and V 2) were moved from the 4th intercostal space to the 3rd and 2nd intercostal spaces. ECG was recorded at the 25 mm/sec recording-speed rate and at normal sensitivity (10 mm/mV), and the QRS duration and corrected QT interval were measured from all leads. The patient ECG data were compared with those of the control group.
The data were expressed as mean±SD or median as appropriate. Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS), for Windows, version 18.0 (SPSS Inc., Chicago, IL, USA). The independent t-test was used to compare the electrocardiographic parameters between groups. Comparisons of the change of the electrocardiographic parameters according to lead position were made using the paired t-test and general linear model. P<0.05 was defined as significance.
Group 1 was composed of 19 patients: 14 males and 5 females. There were 17 patients with TOF, 1 with severe PS, and 1 with pulmonary atresia with intact ventricular septum. Their median age was 4 years (range: 1-21 years), and the range of follow-up period was from 1 year to 20 years after RVOT-PAtomy. Group 2 was composed of 15 patients: 7 males and 8 females. Their median age was 7 years (range: 1-16 years). There were 13 patients with RAtomy and 2 patients with PAtomy, and the range of follow-up period was from 1 year to 12 years after repair. The control group consisted of 29 children (17 males and 12 females). There were 22 normal hearts, 3 PDA, 3 VSD, and 1 ASD, and the median age was 8 years (range: 1-18 years).
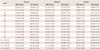
The QRS duration and QTc interval of checked leads are summarized in Table 1. In all limb leads, QRS duration of group 1 and 2 showed significantly more prolonged QRS duration than that of the control group (p=0.001). Group 1 showed the most prolonged QRS duration, but there was no significant difference compared to that of group 2. In all chest leads, QRS duration of group 1 and 2 showed significantly more prolonged QRS duration than that of the control group (p=0.000). The QTc interval showed the same results that the QRS duration revealed. In other words, the QTc intervals of group 1 and 2 were more prolonged than that of the control group, but there was no significant difference between the groups.
The comparison of QRS duration between standard and HICS V 1 and V 2 is summarized in Table 2. In group 1 and 2, there was no significant difference in the degree of intra-patient change and mean QRS duration between traditional standard 12-leads ECG and ECG at HICS. In the control group, the degree of the change between the 4th ICS QRS and 3rd ICS QRS was significant (p=0.031).
Most patients with CHD associated with RVOT obstruction, such as pulmonary atresia or TOF, had RVOT widening via trans-annular incision and right ventriculotomy. These operation methods resulted in injury to the distal part of the right bundle branch, the RBBB, and a prolongation of the QRS duration. Prolongation of QRS duration (>180 ms) is one of the indicators of localized areas of slow conduction and regional delay in systolic activation of the RV wall. In particular, this finding is related mainly to previous surgical repair and fibrosis, and the risk factors for sudden cardiac death after RVOT repair.13) Therefore, early detection of prolonged QRS duration is very important to ensure long-term positive outcomes in patients with RVOT repair, and regular ECG checking is necessary.
The position of ECG leads could have an effect on ECG results. For example, if we change the left and right upper limb leads on opposite sites, the ECG recording reveals opposite vectors of the P wave and T wave in the lead I, aVR, and aVL compared to those of the ECGs in their normal positions. When precordial leads (V 1)-ECG are placed at the HICS or at the right side, the QRS complex changes to the rSR type from the rS type normally. A recent study demonstrated that superior or inferior position of ECG electrodes caused alteration of QRS morphology and predictability of outflow tract ventricular tachycardia origin.14)
In contrast, a positional change of ECG lead is helpful in some cases. Recently, researchers have reported that the Brugada syndrome could be identified more easily using HICS for ECG.15-17) Brugada syndrome is a disease with a high risk of sudden cardiac death related to ventricular fibrillation in healthy adults. It is characterized by coved-type ST-segment elevation in the right precordial leads, but it is not easily detected in asymptomatic patients.18)19) ECGs recorded with precordial leads (V 1 and V 2) in the HICS (3rd ICS) are considered to reflect the potentials of the RVOT and are thought to be useful for detecting the Brugada sign.15-17) The J wave of the Brugada syndrome is generated by a voltage gradient across the myocardial wall of the right ventricular outflow tract. It can be recorded only by electrodes located very close to the site where that phenomenon originates. The positional change of the right precordial lead electrodes at one or two intercostal spaces above their conventional positions may reveal the diagnostic pattern.20)
Unlike cases with trans-annular incision and right ventriculotomy, sometimes, cases with patch closure for VSD can show postoperative RBBB because of injury of the proximal part of the right bundle branch.
From these previous studies, we considered that HICS-ECG lead position might cause alteration of QRS duration in patients with RVOT repair because HICS-ECG lead position may be closer to RVOT, and that it may be helpful to detect early significant prolongation of QRS duration. We attempted to compare the change of QRS duration by HICS-ECG in two different patients' groups with CHD and postoperative RBBB. However, there was no significant difference between traditional standard 12-leads ECG and HICS-ECG in the groups. We were also not able to find a difference between the RBBB by right ventriculotomy and the RBBB by patch closure for VSD. In contrast with our expectation, the positional change of ECG leads didn't have a significant effect on the change of QRS duration after cardiac surgery.
Electrocardiograms at the 3rd ICS showed significantly decreased QRS duration in the control group. Although it was insignificant, ECGs at 3rd ICS showed decreased QRS duration in group 1. This result suggests that, like the previous study,14) alteration of ECG lead position may cause alteration of ECG readings and meaning.
In the present study, the small number of patients and the heterogeneous age group are major limitations. Although 74% of the patients were less than 5 years old, the patients' age was variable, and the difference of QRS duration according to age was not considered. Second, a patient's cardiac condition was not considered. RV volume and pressure loading caused by PS and PR in patients with TOF repair might have an effect on QRS prolongation related to ventricular arrhythmia. Most patients enrolled in the present study did not have significant PR or PS, which was confirmed by echocardiography performed during the follow-up period, and, therefore, the effect of RV loading by PS and PR might not be significant.
In conclusion, although the positional change of ECG leads did not result in a significant effect on measuring QRS duration after surgery, ECG leads at the 3rd ICS rather than 4th ICS may cause alteration of ECG reading. Therefore, we suggest that it is necessary to record ECG as in accurate a position as possible.
Figures and Tables
References
1. Harrison DA, Harris L, Siu SC, et al. Sustained ventricular tachycardia in adult patients late after repair of tetralogy of Fallot. J Am Coll Cardiol. 1997. 30:1368–1373.
2. Kugler JD. Predicting sudden death in patients who have undergone tetralogy of fallot repair: is it really as simple as measuring ECG intervals? J Cardiovasc Electrophysiol. 1998. 9:103–106.
3. Marie PY, Marçon F, Brunotte F, et al. Right ventricular overload and induced sustained ventricular tachycardia in operatively "repaired" tetralogy of Fallot. Am J Cardiol. 1992. 69:785–789.
4. Garson A Jr, Porter CB, Gillette PC, McNamara DG. Induction of ventricular tachycardia during electrophysiologic study after repair of tetralogy of Fallot. J Am Coll Cardiol. 1983. 1:1493–1502.
5. Balaji S, Lau YR, Case CL, Gillette PC. QRS prolongation is associated with inducible ventricular tachycardia after repair of tetralogy of Fallot. Am J Cardiol. 1997. 80:160–163.
6. Gatzoulis MA, Balaji S, Webber SA, et al. Risk factors for arrhythmia and sudden cardiac death late after repair of tetralogy of Fallot: a multicentre study. Lancet. 2000. 356:975–981.
7. Lucron H, Marçon F, Bosser G, Lethor JP, Marie PY, Brembilla-Perrot B. Induction of sustained ventricular tachycardia after surgical repair of tetralogy of Fallot. Am J Cardiol. 1999. 83:1369–1373.
8. Abd El Rahman MY, Abdul-Khaliq H, Vogel M, Alexi-Meskishvili V, Gutberlet M, Lange PE. Relation between right ventricular enlargement, QRS duration, and right ventricular function in patients with tetralogy of Fallot and pulmonary regurgitation after surgical repair. Heart. 2000. 84:416–420.
9. Wu MH. Sudden death in pediatric populations. Korean Circ J. 2010. 40:253–257.
10. Lee YS, Baek JS, Kwon BS, et al. Pediatric emergency room presentation of congenital heart disease. Korean Circ J. 2010. 40:36–41.
11. Rudiger A, Hellermann JP, Mukherjee R, Follath F, Turina J. Electrocardiographic artifacts due to electrode misplacement and their frequency in different clinical settings. Am J Emerg Med. 2007. 25:174–178.
12. Batchvarov VN, Malik M, Camm AJ. Incorrect electrode cable connection during electrocardiographic recording. Europace. 2007. 9:1081–1090.
13. Babu-Narayan SV, Kilner PJ, Li W, et al. Ventricular fibrosis suggested by cardiovascular magnetic resonance in adults with repaired tetralogy of fallot and its relationship to adverse markers of clinical outcome. Circulation. 2006. 113:405–413.
14. Anter E, Frankel DS, Marchlinski FE, Dixit S. Effect of electrocardiographic lead placement on localization of outflow tract tachycardias. Heart Rhythm. 2012. 9:697–703.
15. Sangwatanaroj S, Prechawat S, Sunsaneewitayakul B, Sitthisook S, Tosukhowong P, Tungsanga K. New electrocardiographic leads and the procainamide test for the detection of the Brugada sign in sudden unexplained death syndrome survivors and their relatives. Eur Heart J. 2001. 22:2290–2296.
16. Sangwatanaroj S, Prechawat S, Sunsaneewitayakul B, Sitthisook S, Tosukhowong P, Tungsanga K. Right ventricular electrocardiographic leads for detection of Brugada syndrome in sudden unexplained death syndrome survivors and their relatives. Clin Cardiol. 2001. 24:776–781.
17. Shimizu W, Matsuo K, Takagi M, et al. Body surface distribution and response to drugs of ST segment elevation in Brugada syndrome: clinical implication of eighty-seven-lead body surface potential mapping and its application to twelve-lead electrocardiograms. J Cardiovasc Electrophysiol. 2000. 11:396–404.
18. Nanke T, Nakazawa K, Arai M, et al. Clinical significance of the dispersion of the activation--recovery interval and recovery time as markers for ventricular fibrillation susceptibility in patients with Brugada syndrome. Circ J. 2002. 66:549–552.
19. Takagi A, Nakazawa K, Sakurai T, Nanke T, Miyake F. Prolongation of LAS40 (duration of the low amplitude electric potential component (<40 microV) of the terminal portion of the QRS) induced by isoproterenol in 11 patients with Brugada syndrome. Circ J. 2002. 66:1101–1104.
20. Oreto G, Corrado D, Delise P, et al. Doubts of the cardiologist regarding an electrocardiogram presenting QRS V1-V2 complexes with positive terminal wave and ST segment elevation Consensus conference promoted by the Italian Cardiology Society. G Ital Cardiol (Rome). 2010. 11:11 Suppl 2. 3S–22S.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download