Abstract
Metabolic syndrome (MetS) is characterized by a cluster of cardiovascular risk factors, such as hypertension, glucose intolerance, high triglycerides, and a low high density lipoprotein-cholesterol level. MetS is known to be associated with cardiovascular diseases. In order to diagnose MetS, definitions such as National Cholesterol Education Program Adult Treatment Panel III, American Heart Association/National Heart Lung and Blood Institute, International Diabetes Federation, World Health Organization, European Group for the Study of Insulin Resistance and American College of Endocrinology are widely used. However, using different criteria may lead to confusion regarding the diagnosis and treatment of patients with MetS in the primary care setting. Our objected was to review 3 aspects concerning MetS using the Metabolic Syndrome Research Initiatives study of 123892 healthy Koreans (1994-2001) that had a maximum follow-up of 12 years. The 3 aspects were reviewed by determination of the association of MetS with the development of atherosclerotic cardiovascular disease (ASCVD) and ischemic heart disease (IHD). Based on our findings, each metabolic factor associated with MetS was not weighted equally. The hazard ratio (HR) was higher in individuals with higher glucose compared with the HR in individuals with higher body mass index. Individuals with pre-MetS (having 1 or 2 metabolic factors) had 1.5-2.3 fold higher risk of developing ASCVD and IHD in both genders. In the presence of MetS, both singly and in combination, precede the development of ASCVD and IHD and individuals with pre-MetS must not be ignored as there is no apparent threshold in defining MetS. Furthermore, MetS may complement the Framingham Risk Score and can be used as the first line approach to treat the ASCVD or IHD.
Metabolic syndrome (MetS), known as insulin resistance syndrome, is characterized by a cluster of cardiovascular risk factors such as hypertension, glucose intolerance, high triglycerides, and low high density lipoprotein-cholesterol (HDL-C) concentrations.1) MetS confers an increased risk for vascular disease-associated morbidity and mortality as well as all-cause mortality, even in the absence of clinically evident cardiovascular disease (CVD) and/or diabetes mellitus (DM).2-5) Several organizations have established their own diagnostic criteria for MetS.6) In 1998, the World Health Organization (WHO) standardized a definition of MetS.7) This was revised in 1999 after consultation with the European Group for the Study of Insulin Resistance (EGIR).8) In 2003, the American College of Endocrinology (ACE) provided a new definition of MetS.9) However, the number of risk factors needed for the diagnosis of the MetS has not specified in the ACE definition.9) Therefore in 2001, the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) proposed a practical definition of MetS.10) This was adopted by the Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical Practice in 2003.11) The International Diabetes Federation (IDF), the American Heart Association (AHA), and the National Heart Lung and Blood Institute (NHLBI) issued each diagnostic criteria for the MetS.12) These definitions retained most of the NCEP ATP III criteria and AHA/NHLBI suggested an adjustment of waist circumference to lower thresholds only in some ethnic groups, such as Asians, as well as a lower threshold for elevated fasting glucose (≥100 mg/dL).12)
In fact, different combinations of following metabolic factors are required in each definition of the MetS, including: insulin resistance, dysglycemia, low HDL-C, hypertriglyceridemia, obesity or increased waist circumference, hypertension, impaired glucose tolerance or DM, microalbuminuria, and hyperinsulinemia (Table 1). Furthermore, the importance of each metabolic factor is different in each diagnostic criteria of the MetS. For example, the NCEP ATP III considers that each metabolic factor has the same importance,10) whereas the WHO requires impaired glucose tolerance among its criteria to diagnose MetS.7) The EGIR definition includes insulin determination as an essential component.8) Therefore, this may lead to confusion regarding the diagnosis and treatment of the MetS in the primary care setting when patients are being diagnosed using different criteria.13)
In addition, MetS was found to be inferior to the Framingham Risk Score (FRS) in predicting either type 2 DM or CVD from previous studies. Nonetheless, MetS predicted both type 2 DM, CVD, and vascular diseases.14) While it has not been established whether MetS is a better predictor of diseases, such as type 2 DM, CVD, and other vascular diseases, MetS may be a good all-purpose predictor compared with the FRS.15) Therefore, we intended to review 3 aspects that primarily concerned MetS using the Metabolic Syndrome Research Initiatives (MSRI) study of Koreans with a maximum follow-up of 12 years. Three aspects regarding MetS are as follows: 1) each metabolic factor has different importance; 2) there is an apparent threshold effect; 3) FRS is superior to MetS in relation to the risk of atherosclerotic cardiovascular disease (ASCVD), including myocardial infarction (MI), ischemic heart disease (IHD), total stroke, hemorrhagic stroke and ischemic stroke.
This study included 123892 healthy Koreans (men: 67615, women: 56277) aged 20-80 years, who visited the Health promotion centers for routine health examination from 1994 to 2001 located at both Severance hospital and Samsung hospital. Detailed purpose and methods of data collection were described in our previous study.16) General characteristics of study participants in the MSRI study are described in Table 2.
For data collection, during a standardized examination at the Health promotion centers, their demographic characteristics such as age, gender, and family and past history of clinical diseases, cigarette smoking status (never smoker, ex-smoker and current smoker) and alcohol consumption status (never-drinker and ever-drinker) were collected via a standardized health questionnaire. Body mass index (BMI) was calculated as weight (kg) divided by the square of height (m2). A waist circumference was measured midway between the lower rib and iliac crest. Systolic and diastolic blood pressures were measured in a seated position with a mercury sphygmomanometer or automatic manometer. In addition, MetS components, such as fasting blood glucose, total cholesterol, triglyceride and HDL-C were measured using the Hitachi-7600 analyzer (Hitachi Ltd., Tokyo, Japan).
The principal outcome variables were the incidence of ASCVD including MI, IHD, and stroke subtypes (ischemic, hemorrhagic, and total stroke), as recorded in hospital admission discharge records from 1994-2007. We ascertained these outcomes from health insurance claim data from the National Health Insurance Corporation and checked fatal cases from the National death certificate data.17)18) MI, IHD, ischemic stroke, hemorrhagic and total stroke were defined by the International Classification of Diseases 10th Revision codes: MI, I20; IHD, I20-I25; ischemic stroke, I63-I69; hemorrhagic stroke, I60-I62; total stroke, I60-I69. Morbidity was recorded according to the International Classification of Diseases 10th Revision codes in a standardized manner.17-19) The accuracy rate of the International Classification of Diseases codes for cerebrovascular diseases in medical claims for men in Korea was reported as 83.0% in 2000.20)
Metabolic syndrome was defined by the Third report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (NCEP/ATP III) and the AHA/NHLBI.10) High waist circumferences were defined as ≥90 cm for men and ≥80 cm for women according to Asia-Pacific criteria.21)
In the MSRI study, the prevalence of MetS was 23.8% among men and 16.8% among women. The prevalence of MetS increased with age but decreased among patients aged 70 and older than 70 years. When compared the prevalence of MetS in the MSRI study with that in the Korean National Health and Nutrition Examination Survey, similar patterns of the prevalence of MetS were obtained (data not shown). For outcome variable incident events, the number of incident events of outcome variables in this MSRI study is as follows: MI, 440 events in men, 122 events in women; IHD, 2255 events in men, 1102 events in women; total stroke. There were 1597 events in men, 1046 events in women; ischemic stroke, 1022 events in men, 626 events in women; hemorrhagic stroke, 356 events in men, 265 events in women; All ASCVD; 4153 events in men, and 2560 events in women.
Metabolic syndrome seems to have 3 potential etiological categories: obesity and disorders of adipose tissue; insulin resistance; and a constellation of independent factors, such as molecules of hepatic, vascular, and immunologic origin, that mediate specific components of the MetS.22)
Persons with MetS have at least a 2-fold increase in risk for ASCVD, compared to those without.23) However, the relationship between metabolic risk factors and development of ASCVD is complex and certainly not well understood. Nonetheless, a brief review of hypothesized mechanisms may be of interest. The most common mechanisms in the development of ASCVD include atherogenic dyslipidemia and hyperglycemia.24)
Atherogenic dyslipidemia is characterized by an increase in elevated triglyceride {increased very low-density lipoprotein (VLDL) particle number}, increased small low density lipoprotein (LDL) particles, and low HDL-C.10) For elevated triglyceride, triglyceride-rich lipoproteins were thought not to be atherogenic. However, smaller triglyceride-rich lipoprotein is proven to be atherogenic by studies performed in laboratory animals, in meta-analysis of epidemiological studies, and in clinical trials.24) For small LDL particles, small LDL particles are a surrogate for an increased LDL particle number because the total number of lipoprotein particles in LDL fraction is usually increased in the presence of small LDL particles.25) A low HDL-C level is another characteristic of atherogenic dyslipidemia.10) The increased number of VLDL and LDL particles accounts for the increased level of total apo B usually observed with atherogenic dyslipidemia.10) As low HDL-C rivals an elevated total apo B, it could be said that HDL-C is intimately involved in the atherogenic process. In addition, the presence of a low HDL-C level is strongly associated with the development of ASCVD.23)
In epidemiological studies, the onset of diabetes is accompanied by increased risk for ASCVD, suggesting that hyperglycemia per se is atherogenic.23) Examples include non-enzymatic glycosylation of lipids and proteins, pathogenic effects of advanced glycation products, increased oxidative stress, activation of protein kinase C, and microvascular disease of the vasa vasorum of the coronary arteries.26) However, a direct role of hyperglycemia in ASCVD is still controversial. Another possibility is that insulin resistance per se is independently atherogenic. The risk of ASCVD was found to be increased in persons with insulin resistance.27) Still, further investigation about pathophysiology of MetS in the development of ASCVD is needed.
As mentioned above, several organizations have established their own diagnostic criteria for MetS such as NCEP ATP III, AHA/NHLBI, IDF, WHO, EGIR, and ACE.6) In these diagnostic criteria of the MetS, different combinations of following metabolic factors are required, including: insulin resistance, dysglycemia, low HDL-C, hypertriglyceridemia, obesity or increased waist circumference, hypertension, impaired glucose tolerance or DM, microalbuminuria and hyperinsulinemia (Table 1). However, the importance of each metabolic factor is different in each diagnostic criteria of the MetS. For example, the NCEP ATP III and AHA/NHLBI consider that each metabolic factor has the same importance.10) However, the NCEP-ATP II and AHA/NHLBI does not include a measure of insulin resistance, and it relies upon fasting glucose measurement rather than determination of glucose tolerance. The EGIR definition includes insulin determination as an essential component, while the IDF definition does not essentially require insulin resistance.7)8)28) The IDF definition requires obesity for diagnosis of MetS. This guideline explains that central obesity is a prerequisite for the diagnosis of the MetS, because it is easy to assess and independently associated with each of other MetS components.28) Although increased waist circumference is an important component of MetS, some individuals with multiple risk factors and increased risk for certain diseases, such as CVD, may have normal waist circumference.29)30) Therefore, except for in Asians, the IDF requirement of an increased waist circumference warranted caution because a large proportion of individuals with normal waist circumference have multiple risk factors additionally, and an increased risk of mortality.29)
The WHO guidelines indicate that the presence of diabetes, impaired glucose tolerance, or insulin resistance is necessary for a diagnosis of MetS, because this condition is considered a special classification for individuals with the potential for diabetes (manifested as impaired glucose tolerance, impaired fasting glucose, or insulin resistance determined using the hyperinsulinemic-euglycemic clamp).7)31) A recent study in the Japanese population revealed that the hazard ratio (HR) for CVD was higher among those with high blood glucose compared to those without high blood glucose.32) This finding may suggest that glucose tolerance plays an important role in CVD mortality. Some reports have shown higher HRs with use of the WHO rather than the NCEP definition of MetS. It means that the participants with impaired glucose tolerance have higher HRs.33)
Still, another study among Americans showed unadjusted and adjusted predictive abilities of MetS and their individual components for angiographic coronary artery disease (CAD). In that study, among metabolic factors, HDL and high fasting glucose, but not triglyceride, blood pressure, or BMI, were predictive of CAD in unadjusted and adjusted analyses.34)
In addition, we identified HRs of each metabolic factor for IHD and stroke among Korean men in the MSRI study after adjusting for age, smoking and alcohol consumption, and exercise. For both IHD and stroke, higher HRs was obtained in individuals with higher glucose compared to the HRs in individuals with higher BMI (Fig. 1). It was hard to say that each metabolic factor may have the same importance through the findings obtained in our study using the MSRI cohort study. Importance of each metabolic factor was different in this study. It could be said that it depended on what definitions of MetS were used in predicting certain diseases such as CVD and other vascular diseases. However, the use of different definitions may lead to confusion regarding the diagnosis and treatment of the MetS in the primary care setting when patients are being diagnosed using different criteria.13) Therefore, the use of diagnostic criteria of MetS must be carefully considered in accordance with the characteristics of specific ethnic groups.
The IDF, the AHA, and the NHLBI each subsequently issued diagnostic criteria for the MetS. These definitions retained most of NCEP ATP III criteria and AHA/NHLBI suggested an adjustment of waist circumference to lower thresholds only in some ethnic groups, such as Asians, as well as lower threshold for elevated fasting glucose (≥100 mg/dL).35) However, the IDF definition for other ethnic groups, apart from Asians, retained 3 of the 5 the NCEP ATP III diagnostic criteria, ie hypertension, hypertriglyceridemia, and HDL-C. The IDF set lower thresholds for the remaining 2 diagnostic criteria; for abdominal obesity (waist circumference ≥94 cm for Europid men and ≥80 cm for Europid women) and fasting plasma glucose {≥5.6 mmol/L (100 mg/dL)}.34) Such threshold effects can be obtained in determining the association of MetS with certain diseases such as CVD and other vascular diseases. For example, from a study about MetS and incident cardiovascular morbidity and mortality in a hypertensive population, hypertensive subjects with 3 or more components of MetS had 3-fold higher risk for cardiac events, 2.59 for cerebrovascular and 2.26 for total cardiovascular events compared with those with no other components. In that study, the MetS was defined by the NCEP ATP III.36)
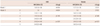
We tried to evaluate age-adjusted and multivariable adjusted HRs for development of ASCVD according to the number of MetS components using NCEP ATP III definition in Korean men and women in the MSRI study (Fig. 2A). Both age-adjusted and multivariable adjusted HRs for development of ASCVD increased with increasing numbers of MetS components in men and women. In a multivariable adjusted analysis, compared to those with no MetS components, men with 3 or more components of MetS components had up to 3.44-fold higher risk for development of ASCVD, while women with 3 or more components of MetS components had up to 4.42-fold higher risk for development of ASCVD. Still, there was no definite apparent threshold effect of the number of MetS and ASCVD. Similar patterns were observed in the association between MetS and development of IHD and stroke among Koreans in the MSRI study (Fig. 2B) (Table 3). Interestingly, in our findings using the MSRI study, when MetS was defined by either NCEP ATP III or AHA/NHLBI, MetS was found to be an independent risk factor for development of IHD. However, this relationship was attenuated when we used IDF definition (data not shown).
However, concerns may arise regarding pre-MetS or those having 1 or 2 metabolic factors in the relationship with the development of ASCVD or IHD. Although those having 1 or 2 metabolic factors are considered as not having MetS, they still had increased risk of development of both ASCVD and IHD in the MSRI study. For example, in the MSRI study, men and women with 1 or 2 metabolic factors had 1.5-2.3 fold higher risk of the development of ASCVD and IHD. From a previous study among middle-aged Japanese men, the multivariate-adjusted relative risk of incidence of CVD compared with absence of MetS components, defined by the WHO, was 3.18, 3.48, 12.55 and 14.15 (p for trend <0.001), for presence of 1, 2, 3 and > or =4 MetS components, respectively. The corresponding relative risks of incidence of type 2 diabetes were 1.92, 4.36, 6.44 and 15.08 (p for trend <0.001).37) There could have the possibility of misleading clinicians in the treatment of individuals who had 1 or 2 metabolic factors.14) Therefore, in the presence of MetS, both singly and in combination, precede the development of ASCVD and IHD and participants with pre-MetS (having 1 or 2 metabolic factors) must not be ignored as there is no apparent threshold in defining MetS.
The FRS was initially designated to predict fatal and nonfatal coronary heart disease (CHD) in the North American population, but this predictive model has also proven its reliability in different ethnic groups.38) The FRS predicts the 10-year risk of CHD according to a gender-specific chart that includes age, smoking status, cholesterol, systolic blood pressure, and diabetic status.39)
Metabolic syndrome is associated with a significantly increased risk of developing type 2 DM and CVD and has been widely promoted as a means of identifying patients for lifestyle intervention to reduce risk factors and incident disease, in particular CVD.40) From previous studies, MetS was found to be inferior to the FRS in predicting either type 2 DM or CVD.14) Some recent US studies also indicated that MetS is inferior to the FRS in predicting CHD.14)22)40) Nonetheless, MetS predicted both type 2 DM, CVD and other vascular diseases.15) It has not been established whether the FRS is a better predictor of the risk of diseases, such as type 2 DM, CVD and other vascular disease than the FRS. MetS could be a good all-purpose predictor compared with the FRS.15)
From a previous study about the comparison between MetS and FRS for prediction of CHD, stroke and type 2 DM, the FRS was a better predictor of CHD and stroke than the MetS but less predictive of type 2 DM. Areas under the receiver-operating characteristic (ROC) curves for FRS vs. the number of metabolic factors were 0.68 vs. 0.59 for CHD, 0.60 vs. 0.70 for type 2 DM and 0.66 vs. 0.55 for stroke (p<0.001 for all).41) From another study showing whether MetS may improve identification of individuals at risk of CHD, comparison of ROC indicated that the MetS did not improve the CHD risk prediction beyond the level achieved by the FRS.39) Therefore, MetS may be used as the first line approach to treat the risk of ASCVD or diabetes. In other words, MetS may complement the FRS. Still, comparing the ability of predictability of MetS vs. the FRS for CVD risk is not a fair comparison.
From a clinical or public health perspective, having a definition of the MetS is useful only if it identifies individuals at high risk of disease and particularly if it identifies individuals who are candidates for a specific treatment that they would not otherwise receive. A prospective study of 123892 healthy Koreans within more than 10 years revealed the substantial effects of the MetS. Our findings suggested that MetS is a risk factor for the development of ASCVD and stroke in the Korean population. There was no apparent threshold relationship between the number of MetS components and ASCVD/stroke. However, pre-MetS or those having 1 or 2 metabolic factors in relation to the risk of both ASCVD and stroke should be concerned as they still had increased risk for ASCVD/stroke. It could result in misleading clinicians in the treatment of individuals who had 1 or 2 metabolic factors.
In conclusion, MetS may be used as the first line approach. Population based cohort studies, in particular in Japan and Korea, are warranted in the near future.
Figures and Tables
Fig. 1
HR for IHD and stroke according to the metabolic syndrome component in Korean men in the MSRI after adjusting for age, smoking, alcohol consumption, and exercise (all p<0.0001). HR: hazard ratio, IHD: ischemic heart disease, BMI: body mass index, TG: triglyceride, HDL-C: high density lipoprotein-cholesterol, BP: blood pressure, MSRI: Metabolic Syndrome Research Initiatives.

Fig. 2
HRs for development of ASCVD and IHD according to MetS in Korean men and women in the MRSI after adjusting for age, smoking, alcohol consumption, and exercise. A: HRs for development of ASCVD according to MetS using NCEP definition. B: HRs for development of IHD according to MetS using NCEP and AHA definition. HR: hazard ratio, ASCVD: atherosclerotic cardiovascular disease, IHD: ischemic heart disease, Mets: Metabolic syndrome, NCEP: National Cholesterol Education Program, MSRI: Metabolic Syndrome Research Initiatives, AHA: American Heart Association.
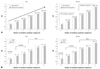
Table 1
Definition, importance of each metabolic factors and limitations of each metabolic syndrome diagnostic criteria

*Other features in AACE include: polycystic ovary syndrome; sedentary lifestyle; age; ethnicity (certain groups); and family history of type 2 diabetes, hypertension, or cardiovascular disease. HDL-C: high density lipoprotein-cholesterol, IS: insulin resistance, IGT: impaired glucose tolerance, IFG: impaired fasting glucose, T2DM: type 2 diabetes mellitus
Acknowledgments
This work was supported by an extramural grant from the Seoul R&BD program, Republic of Korea (10526), a grant from the National R&D Program for Cancer Control, Ministry for Health, Welfare and Family Affairs, Republic of Korea (0920330) and the National Research Foundation of Korea (NRF) grant funded by the Korea government (MEST) (No.2011-0029348).
References
1. Isomaa B, Almgren P, Tuomi T, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001. 24:683–689.
2. Lakka HM, Laaksonen DE, Lakka TA, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002. 288:2709–2716.
3. Dekker JM, Girman C, Rhodes T, et al. Metabolic syndrome and 10-year cardiovascular disease risk in the Hoorn Study. Circulation. 2005. 112:666–673.
4. Ford ES. The metabolic syndrome and mortality from cardiovascular disease and all-causes: findings from the National Health and Nutrition Examination Survey II Mortality Study. Atherosclerosis. 2004. 173:309–314.
5. Alexander CM, Landsman PB, Teutsch SM, Haffner SM. Third National Health and Nutrition Examination Survey (NHANES III). National Ch-olesterol Education Program (NCEP). NCEP-defined metabolic syndrome, diabetes, and prevalence of coronary heart disease among NHANES III participants age 50 years and older. Diabetes. 2003. 52:1210–1214.
6. Eckel RH, Alberti KG, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2010. 375:181–183.
7. Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998. 15:539–553.
8. Balkau B, Charles MA. European Group for the Study of Insulin Resistance (EGIR). Comment on the provisional report from the WHO consultation. Diabet Med. 1999. 16:442–443.
9. Einhorn D, Reaven GM, Cobin RH, et al. American College of Endocrinology position statement on the insulin resistance syndrome. Endocr Pract. 2003. 9:237–252.
10. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA. 2001. 285:2486–2497.
11. De Backer G, Ambrosioni E, Borch-Johnsen K, et al. European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and Other Societies on cardiovascular disease prevention in clinical practice. Eur Heart J. 2003. 24:1601–1610.
12. Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005. 112:2735–2752. Erratum in: Circulation 2005;112:e297-8.
13. Kahn R, Buse J, Ferrannini E, Stern M. American Diabetes Association. European Association for the Study of Diabetes. The metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2005. 28:2289–2304.
14. Stern MP, Williams K, González-Villalpando C, Hunt KJ, Haffner SM. Does the metabolic syndrome improve identification of individuals at risk of type 2 diabetes and/or cardiovascular disease? Diabetes Care. 2004. 27:2676–2681. Erratum in: Diabetes Care 2005;28:238.
15. Meigs JB. Metabolic syndrome: in search of a clinical role. Diabetes Care. 2004. 27:2761–2763. Erratum in: Diabetes Care 2005;28:238.
16. Kimm H, Yun JE, Jo J, Jee SH. Low serum bilirubin level as an independent predictor of stroke incidence: a prospective study in Korean men and women. Stroke. 2009. 40:3422–3427.
17. Kim HC, Kang DR, Nam CM, et al. Elevated serum aminotransferase level as a predictor of intracerebral hemorrhage: Korea Medical Insurance Corporation Study. Stroke. 2005. 36:1642–1647.
18. Jee SH, Sull JW, Park J, et al. Body-mass index and mortality in Korean men and women. N Engl J Med. 2006. 355:779–787.
19. World Health Organization. International Classification of Diseases and Related Health Problems: Manual of the International Statistical Classification of Diseases, Injuries, and Causes of Death. 1992. 10th ed. Geneva: World Health Organization.
20. Park JK, Kim KS, Kim CB, et al. The accuracy of ICD codes for cerebrovascular diseases in medical insurance claims. Korean J Prev Med. 2000. 33:76–82.
21. Inoue S, Zimmet P, Caterson I, et al. The Asia-Pacific Perspective: Redefining Obesity and its Treatments: International Obesity Task Force. 2000. Sydney: Western Pacific Region of the World Health Organization, Health commuication.
22. Grundy SM, Brewer HB Jr, Cleeman JI, Smith SC Jr, Lenfant C. American Heart Association. National Heart, Lung, and Blood Institute. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association Conference on scientific issues related to definition. Circulation. 2004. 109:433–438.
23. Grundy SM, Hansen B, Smith SC Jr, Cleeman JI, Kahn RA. American Heart Association. National Heart, Lung, and Blood Institute. American Diabetes Association. Clinical management of metabolic syndrome: report of the American Heart Association/National Heart, Lung, and Blood Institute/American Diabetes Association conference on scientific issues related to management. Circulation. 2004. 109:551–556.
24. Grundy SM. Obesity, metabolic syndrome, and cardiovascular disease. J Clin Endocrinol Metab. 2004. 89:2595–2600.
25. Blake GJ, Otvos JD, Rifai N, Ridker PM. Low-density lipoprotein particle concentration and size as determined by nuclear magnetic resonance spectroscopy as predictors of cardiovascular disease in women. Circulation. 2002. 106:1930–1937.
26. Aronson D, Rayfield EJ. How hyperglycemia promotes atherosclerosis: molecular mechanisms. Cardiovasc Diabetol. 2002. 1:1.
27. Haffner SM. Cardiovascular risk factors and the prediabetic syndrome. Ann Med. 1996. 28:363–370.
28. Alberti KG, Zimmet P, Shaw J. Metabolic syndrome: a new world-wide definition: a Consensus Statement from the International Diabetes Federation. Diabet Med. 2006. 23:469–480.
29. Katzmarzyk PT, Janssen I, Ross R, Church TS, Blair SN. The importance of waist circumference in the definition of metabolic syndrome: prospective analyses of mortality in men. Diabetes Care. 2006. 29:404–409.
30. Yoon YS, Lee ES, Park C, Lee S, Oh SW. The new definition of metabolic syndrome by the international diabetes federation is less likely to identify metabolically abnormal but non-obese individuals than the definition by the revised national cholesterol education program: the Korea NHANES Study. Int J Obes (Lond). 2007. 31:528–534.
31. World Health Organization. Definition, Diagnosis and Classification of Diabetes Mellitus and Its Complications: Report of a WHO Consultation: Part 1: Diagnosis and Classification of Diabetes Mellitus. 1999. Geneva: World Health Organization.
32. Kadota A, Hozawa A, Okamura T, et al. Relationship between metabolic risk factor clustering and cardiovascular mortality stratified by high blood glucose and obesity: NIPPON DATA90, 1990-2000. Diabetes Care. 2007. 30:1533–1538.
33. Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care. 2005. 28:1769–1778.
34. Anderson JL, Horne BD, Jones HU, et al. Which features of the metabolic syndrome predict the prevalence and clinical outcomes of angiographic coronary artery disease? Cardiology. 2004. 101:185–193.
35. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2012. 35:Suppl 1. S64–S71.
36. Andreadis EA, Tsourous GI, Tzavara CK, et al. Metabolic syndrome and incident cardiovascular morbidity and mortality in a Mediterranean hypertensive population. Am J Hypertens. 2007. 20:558–564.
37. Nakanishi N, Takatorige T, Fukuda H, et al. Components of the metabolic syndrome as predictors of cardiovascular disease and type 2 diabetes in middle-aged Japanese men. Diabetes Res Clin Pract. 2004. 64:59–70.
38. D'Agostino RB Sr, Grundy S, Sullivan LM, Wilson P. CHD Risk Prediction Group. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001. 286:180–187.
39. Jaquet A, Deloumeaux J, Dumoulin M, Bangou J, Donnet JP, Foucan L. Metabolic syndrome and Framingham risk score for prediction of cardiovascular events in Caribbean Indian patients with blood glucose abnormalities. Diabetes Metab. 2008. 34:177–181.
40. McNeill AM, Rosamond WD, Girman CJ, et al. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the atherosclerosis risk in communities study. Diabetes Care. 2005. 28:385–390.
41. Wannamethee SG, Shaper AG, Lennon L, Morris RW. Metabolic syndrome vs Framingham Risk Score for prediction of coronary heart disease, stroke, and type 2 diabetes mellitus. Arch Intern Med. 2005. 165:2644–2650.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download