Introduction
Coronary-pulmonary artery fistulas are rare and usually arise from the left anterior descending or the right coronary artery. They are mostly asymptomatic, but the clinical presentation could include dyspnea, angina, endocarditis, arrhythmias, heart failure, myocardial ischemia, or myocardial infarction.1) We report the case of a man who presented with a myocardial infarction and in whom the coronary angiogram showed tight stenosis of the left anterior descending and the right coronary arteries co-existing with substantial coronary-pulmonary fistulas involving all three major coronary arteries.
Case
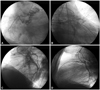
A 47-year-old man with a history of smoking and being overweight presented with an acute anterior ST-segment elevation myocardial infarction. He was more than three hours away from the nearest catheterization laboratory and thus received systemic thrombolysis associated with a loading dose of clopidogrel and aspirin. The treatment was successful during the transfer period. The deferred coronary angiography showed a significant stenosis with thrombus of the proximal left anterior descending coronary artery with Thrombolysis in Myocardial Infarction 3 flow and a tight stenosis of the proximal right coronary artery. Moreover, the coronary angiography highlighted substantial coronary-pulmonary fistulas involving all three major coronary arteries (Fig. 1). The patient received curative unfractionated heparin for 8 days with the standard pharmacological treatment. Echocardiography showed septal akinesis with a left ventricular ejection fraction of 50%. A 99mTc-methoxyisobutylisonitrile single photon emission computerized tomography scintigraphy was performed at day 14 and showed anterior myocardial infarction with inferior myocardial ischemia. The patient was referred for surgery, but he refused intervention. He was discharged under medical treatment.
Discussion
Bilateral coronary-pulmonary artery fistulas were previously described,2)3) but multiple coronary artery fistulas (CAF) arising from all 3 major coronary arteries draining into the pulmonary artery are extremely rare.4) In our case, coronary-pulmonary artery fistulas arising from all 3 major coronary arteries co-existed with myocardial infarction.
Myocardial infarction in patients with CAF seems to have multiple potential etiologies,5) including a prothrombotic tendency, abnormal myocardial perfusion pressure, flow-mediated inflammatory vascular changes, and obviously classical coronary atherosclerosis. In our case, the coronary lesions were close to the CAF which supports the idea of a link between these two pathologies. The decreased coronary blood flow distal to the fistula can also promote myocardial ischemia and myocardial infarction.1) A coronary artery steal by the CAF is a rare cause of myocardial ischemia by itself but may potentiate myocardial ischemia in the presence of another cardiac disease, such as significant coronary stenosis as in our patient.6)
The natural course of CAF is variable. Spontaneous thrombosis with secondary spontaneous closure has been reported.7) Although some doubts have been raised about the treatment strategy in asymptomatic patients with CAF, an interventional option is advocated in symptomatic cases as in our patient.1) Surgical intervention with ligation is the classical therapeutic method. Transcatheter closure of the CAF using coils, chemicals, or covered stents is another therapeutic option. Due to the co-existence of three coronary-pulmonary artery fistulas and coronary lesions, surgical therapy was recommended in our patient, but he refused the procedure.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download