Abstract
Background and Objectives
The relationship between lipid profile and coronary plaque tissue characteristics in patients with stable angina pectoris (SAP) is unclear. The aim of this study was to evaluate the relationship between tissue characteristics and lipid profile and predictors of unstable plaques (UPs) in patients with SAP by virtual histology intravascular ultrasonography (VH-IVUS).
Subjects and Methods
VH-IVUS was performed for target lesions in patients with SAP (61.7±9.2 years, 174 males, n=266) at the time of coronary angiography. UPs are characterized by thin-cap fibroatheroma, ruptured plaque, or remaining thrombus with VH-IVUS.
Results
The present study showed that 34 SAP patients had UPs (61.6±9.2 years, 24 males, 12.8%). The percentage of plaque area in the minimum luminal area in high low density lipoprotein-cholesterol (LDL-C)/high density lipoprotein-cholesterol (HDL-C) ratio patients was significantly higher than in low LDL-C/HDL-C ratio patients (72.7±9.5% vs. 69.9±9.3%, p=0.035). An LDL-C/HDL-C ratio >2.0 was an independent predictor for UPs in SAP patients (odds ratio 5.252, 95% confidence interval 1.132-24.372, p=0.034).
Sudden changes in coronary plaque luminal surface morphology consisting of plaque rupture or fissure have been recognized as important mechanisms of acute coronary syndrome (ACS). Plaque disruption is a reflection of enhanced inflammatory activity within the plaque, and the risk of plaque rupture has been shown to be associated with plaque composition, which includes a large lipid core, a thin fibrous cap, and a high count of macrophages.1)2) The ability to visualize and quantify the different components of atherosclerotic lesions provides important information not only on the mechanism of coronary artery disease (CAD) but also on potential future therapeutic interventions to alter the disease process.3) Recently, virtual histology intravascular ultrasonography (VH-IVUS) using spectral analysis of radiofrequency ultrasound backscatter signals was introduced to clinical practice to characterize plaque composition.4)
The low density lipoprotein-cholesterol (LDL-C)/high density lipoprotein-cholesterol (HDL-C) ratio is a predictor of CAD risk and a surrogate marker of lipid-lowering therapies.5) Meta-analysis data from 4 studies using conventional IVUS has indicated a positive linear correlation between achieved LDL-C/HDL-C ratio and percent volume changes of coronary plaque burden.6) Moreover, Kimura et al.7) reported that an elevated LDL-C/HDL-C ratio may be a positive predictor for coronary lipid-rich plaques and plaque vulnerability in patients with chronic CAD. However, few reports have evaluated any link between the types of CAD, coronary plaque vulnerability, and blood lipid profiles.
Therefore, the purpose of this study was to determine the characteristics of coronary plaque tissue and to examine the relationship between coronary plaque tissue according to lipid profile characteristics visualized with VH-IVUS and lipid profiles in patients with stable angina pectoris (SAP).
This study was a retrospective, single-center study. From August 2007 to December 2010, we identified 266 consecutive patients (61.7±9.2 years, 174 males) with SAP who underwent coronary angiography (CAG) and VH-IVUS for target lesions before percutaneous coronary intervention (PCI). The presence of SAP was determined by typical effort-induced chest pain which was relieved by resting. Patients were divided into an unstable plaque (UP) group (61.6±9.2 years, 24 males, n=34) and a stable plaque (SP) group (61.7±9.2 years, 150 males, n=232). UPs are characterized by thin-cap fibroatheroma (TCFA), ruptured plaque, or remaining thrombus on VH-IVUS. The inclusion criterion was elective PCI in a de novo lesion due to symptomatic CAD without any prior history of PCI. In patients with single-vessel disease, the most severe lesion was considered the target lesion. In patients with multivessel disease and angina, the selection was determined by the combination of left ventricular wall motion abnormalities, electrocardiographic findings, single-photon emission computed tomography, and the closest corresponding coronary vessel containing the most severe lesion. We excluded patients with restenosis after PCI, coronary artery bypass grafting, total occlusions, bifurcation lesions, lesions with severe angulations, and heavily calcified lesions.
Fasting blood sampling was obtained for measuring lipid profiles, high sensitivity C-reactive protein (hs-CRP), and creatinine before CAG. The serum levels of total cholesterol, LDL-C, HDL-C, and triglyceride were measured by standard enzymatic methods. hs-CRP was analyzed turbidimetrically using sheep antibodies against human CRP; this has been validated against the Dade-Behring method.8) Lipoprotein A {Lp(a)} was measured by an immunonephelometric assay using a latex Lp(a) reagent composed of polystyrene particles coated with a rabbit anti-human Lp(a) γ-globulin fraction. Apolipoprotein A1, apolipoprotein B, and Lp(a) were measured using a Behring Nephelometer II (Dade Behring Inc., Deerfield, IL, USA).
Coronary angiogram was analyzed with a validated quantitative coronary angiography (QCA) system (Philips H5000 or Allura DCI program, Philips Medical System, Eindhoven, the Netherlands). With the outer diameter of the contrast-filled catheter as the calibration standard, the minimal lumen diameter, reference diameter, and diameter stenosis were measured in diastolic frames from orthogonal projections.
Virtual histology intravascular ultrasonography examination was performed before any intervention and after intracoronary administration of nitroglycerin 200 µg using a motorized transducer pullback system (0.5 mm/s). A 2.9 Fr IVUS imaging catheter (Eagle Eye; Volcano Corporation, Rancho Cordova, CA, USA) incorporated a 20 MHz phased-array transducer.
Conventional gray-scale quantitative IVUS analyses were performed according to the American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, Measurement, and Reporting of Intravascular Ultrasound Studies.9) Percent plaque area of the minimum luminal area (MLA) was defined as the plaque and media area divided by the external elastic membrane (EEM) area. A remodeling index (RI) was calculated as the lesion EEM divided by the mean reference EEM area. The IVUS sign of plaque rupture was a cavity that communicated with the lumen with an overlying residual fibrous cap fragment.10)11) Thrombus was an intraluminal mass having a layered or lobulated appearance, evidence of blood flow (microchannels) within the mass, and speckling or scintillation.9)12) VH-IVUS analysis classified tissue into four major color-coded components: green (fibrotic), yellow-green (fibro-fatty), white (dense calcium), and red {necrotic core (NC)}. VH-IVUS analysis was reported in absolute amounts and as a percentage of plaque area. VH-IVUS-derived TCFA was defined as a NC ≥10% of plaque area at the MLA site in ≥3 consecutive frames without evident overlying fibrous tissue in the presence of ≥40% plaque burden.13)
The Statistical Package for Social Sciences for Windows, version 15.0 (Chicago, IL, USA) was used for all analyses. Continuous variables were presented as mean±standard deviations, and differences between the 2 groups were evaluated by the Student's t-test. Categorical variables were presented as numbers (percentages), and comparisons across the 2 groups were performed by the chi-square test or Fisher's exact test. A multivariate logistic regression analysis was used to assess the independent predictors of UP. Patient baseline variables were entered into the regression model if they were statistically significant (p<0.2) by univariate analysis. All analyses were 2-tailed with clinical significance defined as values of p<0.05.
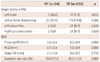
Two hundred sixty-six consecutive SAP patients were enrolled in the study. Thirty-four patients had a diagnosis of UP, and 232 had SP. HDL-C, LDL-C/HDL-C ratio >2.0 and Apolipoprotein A1 were significantly lower in the UP group than in the SP group, whereas other variables in the 2 groups were similar (Table 1).
Quantitative coronary angiography showed that the target artery of the left main was more common in the UP group than in the SP group (20.6% vs. 7.3%, p=0.012), the minimal luminal diameter (MLD) was significantly smaller in the UP group than in the SP group (0.7±0.4 mm vs. 1.0±0.4 mm, p=0.004), and the stenosis diameter (SD) was significantly higher in the UP group than in the SP group (79.0±11.0% vs. 70.3±13.0%, p=0.001) (Table 2).
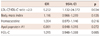
Gray-scale IVUS showed that the EEM cross-sectional area (CSA) of the lesion segment (18.0±6.7 mm2 vs. 13.1±3.9 mm2, p=0.001), percent plaque area of the MLA (77.7±7.0% vs. 71.1±9.6%, p=0.001), and the EEM CSA of the distal reference segment (13.7±6.6 mm2 vs. 11.0±4.0 mm2, p=0.037) were significantly larger in the UP group than in the SP group. RI was significantly higher in the UP group than in the SP group (1.13±0.18 vs. 0.97±0.20, p=0.001), and target lesions in all patients contained 4 thrombi (1.5%) and 22 ruptured plaques (8.3%). VH-IVUS showed that the NC area was significantly greater (2.2±1.6 mm2 vs. 1.4±1.0 mm2, p=0.024), and a tendency toward greater percentages of NC (27.9% vs. 21.6%, p=0.356) was present in the UP group. Target lesions in all patients contained 12 TCFAs (4.5%) (Table 3).
Multiple logistic regression analysis was performed using LDL-C/HDL-C ratio >2.0, body mass index, homocysteine, apolipoprotein A1, and HDL-C. In patients with SAP, LDL-C/HDL-C ratio >2.0 was the only independent predictor for UP (odds ratio 5.252, 95% confidence interval 1.132-24.372, p=0.034) (Table 4).
We evaluated the relationship between plaque vulnerability and lipid profiles using IVUS in patients with SAP. The present study showed that a high LDL-C/HDL-C ratio was a useful marker for UP in patients with SAP.
Coronary luminal stenosis as assessed by angiography has been considered a surrogate marker of atherosclerotic severity. However, CAG, a luminogram, has low predictive value to assess atherosclerotic plaque burden or to predict ACS events.14)15) Nevertheless, SAP patients have flow-limiting culprit lesions in their coronary arteries, and such lesions may be closely related to plaque vulnerability and plaque composition as a result of lower shear stress and endothelial dysfunction.16) It is also well known that a vulnerable plaque rarely develops in <40% plaque volume. Therefore, a culprit lesion with a coronary blood flow limiting site may have a considerable relation to plaque vulnerability compared to a non-flow limiting lesion. Although identification of mild/moderate vulnerable stenosis has the most relevant clinical implications, clinical validation and confirmation of VH data on culprit lesions, which are the lesion subset best studied, are required.
Virtual histology intravascular ultrasonography has the potential to provide detailed qualitative and quantitative information; the identification of 4 specific plaque components has been validated in explanted human coronary segments, as well as in retrieved directional coronary atherectomy specimens.17)
The rupture of a vulnerable plaque and subsequent thrombus formation are the most important mechanisms leading to ACS.2)18) One angioscopic study reported that plaque rupture and subsequent thrombus formation were observed in 17% of SAP patients.19) A study which investigated the relationship between clinical and angiographic observations with plaque rupture detected by IVUS has demonstrated that 22% of coronary plaques ruptured even in patients with stable angina or asymptomatic patients.20) IVUS studies have reported varying frequencies of plaque rupture in SAP patients: 15% by Hong et al.,21) 18.5% by Hur22) and 10.7% by Bae et al.23) In the present study, 12.8% of SAP patients had plaques with vulnerable characteristics.
It is well established that high serum levels of LDL-C constitute a strong predictor of CAD and that LDL-C-lowering therapy reduces CAD.24) The LDL-C/HDL-C ratio was found to be more accurate in determining CAD risk compared to LDL-C or HDL-C alone.5)25) Based on data from clinical trials using conventional IVUS (REVERSAL, CAMEROT, ACTIVATE, and ASTEROID),6)26-28) a high LDL-C/HDL-C ratio is associated with coronary plaque progression, while a low LDL-C/HDL-C ratio achieved by pharmacological intervention is associated with coronary plaque regression. According to a subanalysis of the MEGA Study, which focused on primary prevention of cardiovascular events in a Japanese population, the incidence of cardiovascular events was significantly lower in those with an LDL-C/HDL-C ratio of 2.0 or lower than in those with an LDL-C/HDL-C ratio exceeding 2.0 regardless of the HDL-C level.29) Nicholls et al.6) performed pooled analysis by integrating the data of 4 prospective, randomized trials using IVUS to assess plaque regression as a result of LDL-C lowering therapy for secondary prevention of CAD and demonstrated that plaques were regressed by controlling the LDL-C/HDL-C ratio at 1.5 or lower. In the present study, an LDL-C/HDL-C ratio >2.0 in patients with SAP was the independent predictor of plaques with vulnerable characteristics. In addition, the present study showed that the percent plaque area of MLA in high LDL-C/HDL-C ratio patients was significantly higher than in the low LDL-C/HDL-C ratio patients.
In the present study, characteristics of plaques detected using IVUS were associated with the LDL-C/HDL-C ratio. Therefore, increased LDL-C/HDL-C ratio represented by an increase in LDL-C and/or decrease in HDL-C might increase the percent plaque area of MLA and may be a useful predictor for plaque vulnerability, which is a potent predictor of future cardiovascular events. However, further investigations are needed to clarify this relationship.
Several limitations exist in the present study. First, the present study was retrospective and consisted of a relatively small number of patients from a single center. Therefore, a larger scale, well-organized prospective study is needed. Second, IVUS imaging was performed at the discretion of the individual operators. Thus, these situations might lead to potential selection bias. Third, the IVUS image was only a single slice at the MLD site of the target lesion. We believe, however, that flow-limiting lesions might be related to low shear stress and endothelial dysfunction in patients with CAD.
Figures and Tables
Acknowledgments
This study was supported by a grant of the Korea Healthcare technology R & D Project (A084869), Ministry for Health, Welfare & Family Affairs, Republic of Korea.
References
1. Ross R. Atherosclerosis: an inflammatory disease. N Engl J Med. 1999. 340:115–126.
2. Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. J Am Coll Cardiol. 2006. 47:8 Suppl. C13–C18.
3. Bae JH, Rihal CS, Lerman A. Tissue characterization of coronary plaques using intravascular ultrasound/virtual histology. Korean Circ J. 2006. 36:553–558.
4. Nair A, Margolis MP, Kuban BD, Vince DG. Automated coronary plaque characterisation with intravascular ultrasound backscatter: ex vivo validation. EuroIntervention. 2007. 3:113–120.
5. Manninen V, Tenkanen L, Koskinen P, et al. Joint effects of serum triglyceride and LDL cholesterol and HDL cholesterol concentrations on coronary heart disease risk in the Helsinki Heart Study: implications for treatment. Circulation. 1992. 85:37–45.
6. Nicholls SJ, Tuzcu EM, Sipahi I, et al. Statins, high-density lipoprotein cholesterol, and regression of coronary atherosclerosis. JAMA. 2007. 297:499–508.
7. Kimura T, Itoh T, Fusazaki T, et al. Low-density lipoprotein-cholesterol/high-density lipoprotein-cholesterol ratio predicts lipid-rich coronary plaque in patients with coronary artery disease: integrated-backscatter intravascular ultrasound study. Circ J. 2010. 74:1392–1398.
8. Roberts WL, Moulton L, Law TC, et al. Evaluation of nine automated high-sensitivity C-reactive protein methods: implications for clinical and epidemiological applications: part 2. Clin Chem. 2001. 47:418–425.
9. Mintz GS, Nissen SE, Anderson WD, et al. American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, Measurement and Reporting of Intravascular Ultrasound Studies (IVUS): a report of the American College of Cardiology Task Force on clinical expert consensus documents. J Am Coll Cardiol. 2001. 37:1478–1492.
10. Mintz GS, Maehara A, Bui AB, Weissman NJ. Multiple versus single coronary plaque ruptures detected by intravascular ultrasound in stable and unstable angina pectoris and in acute myocardial infarction. Am J Cardiol. 2003. 91:1333–1335.
11. Hong MK, Mintz GS, Lee CW, et al. Comparison of coronary plaque rupture between stable angina and acute myocardial infarction: a three-vessel intravascular ultrasound study in 235 patients. Circulation. 2004. 110:928–933.
12. Chemarin-Alibelli MJ, Pieraggi MT, Elbaz M, et al. Identification of coronary thrombus after myocardial infarction by intracoronary ultrasound compared with histology of tissues sampled by atherectomy. Am J Cardiol. 1996. 77:344–349.
13. Rodriguez-Granillo GA, García-García HM, Mc Fadden EP, et al. In vivo intravascular ultrasound-derived thin-cap fibroatheroma detection using ultrasound radiofrequency data analysis. J Am Coll Cardiol. 2005. 46:2038–2042.
14. Pasterkamp G, Falk E, Woutman H, Borst C. Techniques characterizing the coronary atherosclerotic plaque: influence on clinical decision making? J Am Coll Cardiol. 2000. 36:13–21.
15. Little WC, Constantinescu M, Applegate RJ, et al. Can coronary angiography predict the site of a subsequent myocardial infarction in patients with mild-to-moderate coronary artery disease? Circulation. 1988. 78(5 Pt 1):1157–1166.
16. Malek AM, Alper SL, Izumo S. Hemodynamic shear stress and its role in atherosclerosis. JAMA. 1999. 282:2035–2042.
17. Nasu K, Tsuchikane E, Katoh O, et al. Accuracy of in vivo coronary plaque morphology assessment: a validation study of in vivo virtual histology compared with in vitro histopathology. J Am Coll Cardiol. 2006. 47:2405–2412.
18. Naghavi M, Libby P, Falk E, et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: part 1. Circulation. 2003. 108:1664–1672.
19. De Feyter PJ, Ozaki Y, Baptista J, et al. Ischemia-related lesion characteristics in patients with stable or unstable angina: a study with intracoronary angioscopy and ultrasound. Circulation. 1995. 92:1408–1413.
20. Maehara A, Mintz GS, Bui AB, et al. Morphologic and angiographic features of coronary plaque rupture detected by intravascular ultrasound. J Am Coll Cardiol. 2002. 40:904–910.
21. Hong MK, Mintz GS, Lee CW, et al. Comparison of virtual histology to intravascular ultrasound of culprit coronary lesions in acute coronary syndrome and target coronary lesions in stable angina pectoris. Am J Cardiol. 2007. 100:953–959.
22. Hur SH. Lesion characteristics in patients with acute coronary syndrome: a comparison with lesion in patients with stable angina by intravascular ultrasound. Korean Circ J. 2004. 34:548–557.
23. Bae JH, Kwon TG, Kim KH, Hyun DW, Kim KY, Kim DS. In-vivo coronary plaque composition in patients with acute coronary syndrome: a virtual histology intravascular ultrasound study. Korean Circ J. 2007. 37:437–442.
24. Sakamoto T, Ogawa H. "Just make it lower" is an alternative strategy of lipid-lowering therapy with statins in Japanese patients: LDL-cholesterol: the lower, the better; is it true for Asians? (Con). Circ J. 2010. 74:1731–1741.
25. Kannel WB. Lipids, diabetes, and coronary heart disease: insights from the Framingham Study. Am Heart J. 1985. 110:1100–1107.
26. Schoenhagen P, Tuzcu EM, Apperson-Hansen C, et al. Determinants of arterial wall remodeling during lipid-lowering therapy: serial intravascular ultrasound observations from the Reversal of Atherosclerosis with Aggressive Lipid Lowering Therapy (REVERSAL) trial. Circulation. 2006. 113:2826–2834.
27. Brener SJ, Ivanc TB, Poliszczuk R, et al. Antihypertensive therapy and regression of coronary artery disease: insights from the Comparison of Amlodipine versus Enalapril to Limit Occurrences of Thrombosis (CAMELOT) and Norvasc for Regression of Manifest Atherosclerotic Lesions by Intravascular Sonographic Evaluation (NORMALISE) trials. Am Heart J. 2006. 152:1059–1063.
28. Nissen SE, Nicholls SJ, Sipahi I, et al. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA. 2006. 295:1556–1565.
29. Nakamura H, Mizuno K. MEGA Study Group. Abstract 6282: lowered ratio of low-density lipoprotein cholesterol to high-density lipoprotein cholesterol with lipid-lowering therapy associated with reduction of cardiovascular events in primary prevention: MEGA Study post-hoc analysis. Circulation. 2008. 118:S1174.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download