Abstract
Background and Objectives
Patent ductus arteriosus (PDA) is a significant cause of morbidity and mortality in preterm infants. Measurement of plasma B-type natriuretic peptide (BNP) has been reported to be a useful bedside screening tool for the presence of hemodynamically significant PDA (hsPDA) in neonates. This study was conducted to investigate the usefulness of a BNP assay as a biochemical marker for the diagnosis of hsPDA and predictive biomarker of the response to indomethacin in preterm infants.
Subjects and Methods
Preterm infants born at <37 weeks' gestational age were prospectively enrolled within 24 hours of birth. Plasma BNP levels were measured on days 1, 4, and 7. Significant PDA was diagnosed by large ductal flow with left to right shunt on color Doppler echocardiography, along with clinical features of PDA. Following that, hsPDA was treated with indomethacin.
Results
A total of 28 preterm infants were prospectively enrolled in this study. Seven infants with PDA had higher on day 4 plasma BNP values (median 654.68 pg/mL; range 428.29-1280.00) compared to the control group (median 124.52 pg/mL; range 37.21-290.49). The area under the receiver operator characteristic curve for the detection of hsPDA was high: 0.998 (95% confidence interval: 0.995-1.002). The cutoff of BNP concentration for the diagnosis of hsPDA was determined to be 412 pg/mL (sensitivity: 100%; specificity: 95%).
Patent ductus arteriosus (PDA) refers to the persistent patency of the ductus arteriosus after birth. In most term infants, the ductus arteriosus closes during the first 48 hours after birth. However, in many small preterm infants the ductus remains open allowing an increasing systemic-to-pulmonary shunt as the pulmonary vascular resistance falls.1) In premature infants, the ductus frequently fails to undergo spontaneous closure due to the elevated sensitivity of the ductal tissue to the dilating effects of prostaglandins and low sensitivity to the effects of oxygen.2) As a result, the ductus of preterm infants can remain open for many days, and although it may constrict initially, it frequently reopens.3) PDA has been recognized as a cause of significant comorbidity in premature infants. In addition to pulmonary congestion and heart failure caused by the left-to-right shunt of PDA, clinical sequelae of the ductal steal of blood from the PDA present high risks of intraventricular hemorrhage,4) bronchopulmonary dysplasia,5) pulmonary hemorrhage,6) renal hypoperfusion,7) necrotizing enterocolitis, and death.8) Therefore, early diagnosis of hemodynamically significant PDA (hsPDA) allows early treatment and probable reduction of morbidity in preterm infants.6)9)
Because physical examination may be unreliable for determining the presence and magnitude of PDA in premature infants, echocardiography is used to document PDA shunting. However, routine echocardiography for the evaluation of PDA in premature infants has certain disadvantages, such as high cost, discomfort, disruption of the neonatal environment, and limited availability in some centers.10) Moreover, the hemodynamic effect of a PDA may be difficult to determine even by using echocardiography, and the clinical course cannot be predicted reliably.11)
B-type natriuretic peptide (BNP) is a cardiac natriuretic hormone, mainly produced by the cardiomyocytes and is characterized by diuretic, natriuretic and vasodilatatory properties. In particular, BNP is produced by ventricular cells in response to volume expansion and pressure load and in cardiac heart failure.12)13) BNP antagonizes the renin-angiotensin-aldosterone system, and reduces intravascular volume, and ventricular preload and afterload. It has been associated with the regulation of pulmonary vasculature, possibly including the ductus arteriosus.14)
B-type natriuretic peptide can be a useful bedside screening tool for the presence of hsPDA in premature infants.15) Recent studies have further demonstrated the potential of BNP to guide an indomethacin therapeutic strategy for these patients.16)
We evaluated the clinical usefulness of the measurement of plasma BNP levels in preterm infants. For accurate diagnosis of hsPDA, we performed repeated BNP level measurements and determined the best cut-off value of BNP on day 4 of life and the change in BNP level after treatment with indomethacin for predicting hsPDA.
This prospective study was conducted at the neonatal intensive care unit of Hallym University Sacred Heart Hospital. Preterm infants born at <37 weeks' gestational age (GA) were eligible for entry into the study. The infants were enrolled within 24 hours of birth. Preterm infants with congenital anomalies, cardiac abnormalities other than patent foramen ovale, and intraventricular hemorrhage occurring before 48 hours of life were excluded from this study. Thirty-three preterm infants were initially enrolled during a 5-month period (from April 2009 to August 2009). The data of 5 infants were excluded from analysis because the data were incomplete. Twenty-eight infants (12 male, 16 female) were eligible for evaluation. Their mean GA was 32.7 weeks (range: 28.4-35.8 weeks) and the mean birth weight was 1918 g (range: 1080-2830 g). We prospectively evaluated the infants for PDA within the first 7 days of life and administered indomethacin if hsPDA was diagnosed based on a large ductal flow with left to right shunt on color Doppler echocardiography.
Blood samples for BNP level were collected by umbilical venous catheter aspiration or from the peripheral vein and were transferred into ethylenediaminetetraacetic acid tubes. Blood samples were taken on days 1, 4, and 7 after birth. BNP concentrations were detected using a commercial diagnostics system (Aggott achitect BNP assay, Abbott Diagnostics, Abbott Park, IL, USA).
A GE Vivid 7 Dimension cardiovascular ultrasound machine with curvilinear 8 MHz transducer incorporating color-flow, pulsed-wave, and continuous-wave Doppler was used (GE Healthcare, Fairfield, CT, USA). A two-dimensional color flow Doppler echocardiography was performed on all infants within the fourth day of life for assessment of PDA and to rule out congenital heart disease. A significant PDA was diagnosed based on the presence of a large ductal flow with left to right shunt with retrograde flow in the descending aorta, as demonstrated on the two-dimensional color Doppler echocardiograph.17-19) To estimate the magnitude of left to right shunting across the PDA, a ratio of the diameters of the left atrial to aortic root (LA/AO) was evaluated in the parasternal long axis view at the level of the aortic valve. The infants with hsPDA were treated with three doses of indomethacin.20) Follow-up echocardiography was performed on day 8 of life by one investigator to avoid inter-observer variability.
Hemodynamically significant PDA was diagnosed if the infant fulfilled the echocardiographic criteria and had at least 3 of the following 6 clinical signs of cardiovascular dysfunction including 1) systolic or continuous murmur at the left sterna edge, 2) increased precordial impulse, 3) bounding peripheral pulses, 4) resting tachycardia, 5) unexplained deterioration of the respiratory status, and 6) increased pulmonary vascular markings and cardiac enlargement or signs of pulmonary edema on the chest radiograph. The echocardiographic criteria included 1) LA/AO diameter ratio >1.4. 2) Diastolic turbulence (backflow) on the Doppler echocardiograph of the pulmonary artery, and 3) ductal diameter of PDA >1.4 mm.21)
Indomethacin (Indocin®, Merck Sharp and Dohme, West Point, PA, USA) was given as a 60-minute intravenous infusion at 24-hour intervals for each course (3 doses). For the initial indomethacin dose, 0.2 mg/kg was administered to all patients regardless of their age.22) For the second or third dose, 0.1 mg/kg was administered when the patient was <48 hours old, and 0.2 mg/kg was administered when the patient was 2 to 7 days old, respectively.
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) version 15.0 (SPSS Inc., Chicago, IL, USA). Continuous variables are presented as mean values with standard deviation. We used the Fisher's exact test to compare categorical variables and the Mann-Whitney's rank sum U test to compare continuous variables. The Mann-Whitney's rank-sum U test was used to calculate the differences of BNP levels between the groups. Receiver operator characteristic (ROC) analysis was performed to determine the best cut-off values of plasma BNP levels for the detection of significant PDA. A p<0.05 was considered significant.
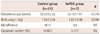
For a 5-month period, 28 preterm infants (12 male, 16 female) were prospectively enrolled in our study. Of the 28 infants, 21 infants had no hsPDA (control group, mean GA: 32.83 weeks; mean birth weight: 1930 g). The remaining 7 infants had hsPDA, which required treatment with indomethacin (hsPDA group, mean GA: 32.18 weeks; mean birth weight: 1850 g). The characteristics of the infants in these 2 groups are summarized in Table 1. No significant differences were observed in GA, birth weight, sex, or delivery type.
This study showed a significant correlation between BNP levels on day 4 of life and presence of PDA in preterm infants (Table 2). On day 4 of life, the mean BNP concentration in the hsPDA group was significantly higher than that in the control group (median 654.68 vs. 124.52 pg/mL; p<0.001) (Fig. 1). Seven infants in the hsPDA group showed clinical symptoms, such as continuous murmur at the left sterna edge, resting tachycardia, and tachypnea. on day 8 of life, the 7 infants in the hsPDA group became asymptomatic after the administration of 3 doses of indomethacin. All the infants in the hsPDA group completed their therapy with a single treatment course (3 doses), and without the need for a second course of indomethacin. At the second echocardiographic evaluation (on day 8 of life), the ductus of 5 infants in the hsPDA group were closed. In the remaining 2 infants with hsPDA, ductal shunt was reduced and ductal closure was confirmed 7 days later. After treatment with indomethacin, the BNP levels in the hsPDA group decreased significantly (median 654.68 vs. 288.48 pg/mL; p<0.001).
In the control group 18 infants demonstrated a progressive fall in plasma BNP level from day 1 to day 7. The remaining 3 control group infants demonstrated an initial fall and subsequent rise in the plasma BNP level. Upon reviewing the clinical records of these latter infants, they had late onset sepsis between day 4 and day 7 of life. All subjects in the hsPDA group had no sepsis by day 7 of life. In this study, there was no preterm infant with pulmonary hypertension.
At the first echocardiographic evaluation, a significant correlation was observed between the LA/AO diameter ratios and BNP levels (r=0.812; p<0.001) (Fig. 2).
The area under the ROC curve for the detection of PDA was statistically significant at 0.998 (95% confidence interval: 0.995-1.002). The level of plasma BNP on day 4 of life was a highly sensitive indicator of hsPDA (sensitivity 100%; specificity 95%) with a cutoff value of 412 pg/mL (Fig. 3).
B-type natriuretic peptide has a 32 amino acid ring structure. It acts on a cyclic guanosine monophosphate-coupled receptor via a transmembrane domain.23) The ventricles of the heart are the main site of BNP synthesis and release in response to volume and pressure loading, as well as ventricular stress.12)13)
B-type natriuretic peptides have a major role in the screening and diagnosis of cardiac disease and monitoring of the treatment response in children and adults. Recent studies have concentrated on the potential use of these markers in pediatric and neonatal medicine. In all neonates, BNP concentrations increase on day 1 of life and show a typical peak, even in the absence of a significant patent of the ductal arteriosus, and subsequently decrease with chronological age.24) The BNP levels in preterm infants were higher than in healthy term infants during the first few days after birth. In particular, when PDA is present in preterm infants, the BNP concentration is abnormally high and reflects the magnitude of shunting through the PDA. Holmström et al.11) reported that plasma levels of natriuretic peptides in preterm infants are strongly related to the hemodynamic influence of PDA. Since then, plasma natriuretic peptide levels, including increased BNP levels, were studied to determine the presence of hsPDA in preterm infants. Flynn et al.10) showed that BNP levels strongly correlated with ductal size in premature neonates. We measured the plasma BNP levels in preterm infants during the first 7 days of life. On day 4 of life, plasma BNP levels in infants with hsPDA were significantly higher than in infants without hsPDA, although the primary limitation of this study was its small sample size. The best cutoff BNP concentration on day 4 of life was 412 pg/mL; sensitivity was 100%, and specificity was 95%. Flynn et al.10) showed that the best cutoff of BNP concentration is 300 pg/mL and a lower cutoff of 105 pg/mL for infants at >2 days of life. Lee et al.25) showed that the best cutoff at 24 hours of age is 468.5 pd/mL and at 48 hours of age is 935 pg/mL. In another study, the best cutoff BNP concentration on day 3 of life was 1110 pg/mL.26)
Hsu et al.27) reported that the mean BNP levels decreased significantly in response to indomethacin. They classified as responders and non-responders in preterm infants with PDA. After treatment with indomethacin, the mean BNP levels in the responders decreased significantly from the baseline 24 hours after the final dose, whereas the BNP levels in the non-responders did not change significantly. We could not conduct a comparative study of indomethacin responsiveness because all the hsPDAs closed after indomethacin administration. Moreover, in our study, the sample size was smaller, the birth weights were larger, and the GA was higher than in the previous study. However, our results demonstrated that the mean BNP level in the hsPDA group decreased significantly after indomethacin treatment. Moreover, significantly decreasing BNP levels predicted a good response to indomethacin treatment and ductal closure.
In this study, 3 infants in the control group, with increased BNP concentration from day 4 to 7, had late onset sepsis but a lower mean BNP concentration on day 7 compared with the hsPDA group. In animal studies, plasma BNP levels have been shown to rise with induced endotoxemia, and the pro-inflammatory cytokine interleukin-6 has been linked with BNP production.28) In patients with severe sepsis or septic shock, BNP levels are highly elevated. In a comparative study on children with sepsis and those with acute left ventricular dysfunction, BNP levels were found to be higher in the latter group. Therefore, BNP serves as a marker for cardiac dysfunction associated with sepsis in preterm neonates.29)30)
Echocardiography is the main method used to detect PDA in newborns. Although BNP may not replace echocardiography for the diagnosis of PDA, it may obviate the need to perform repeated echocardiography in order to confirm ductal closure after treatment. BNP measurement can be used as an adjunct to echocardiography for diagnosing PDA. Although it is not a stand-alone test, the BNP assay is an immediate method for providing valuable information that indicates whether an infant requires intervention for PDA, and determines the clinical course of PDA in a preterm infant. BNP may be a useful screening tool for detecting the presence of a PDA in premature neonates, because levels of BNP are higher in the presence of a significant patent ductus. In addition, serial BNP measurements may be of value in assessing the clinical course of PDA and a possible alternative to repeated echocardiography in the diagnosis and management of PDA in preterm infants.
Figures and Tables
Fig. 1
Plasma B-type natriuretic peptide (BNP) values on days 1, 4 and 7 of life. PDA: patent ductus arteriosus.

Fig. 2
Correlation between LA/AO ratio and BNP level. BNP levels correlated positively with the LA/AO ratio (r=0.812; p< 0.001). BNP: B-type natriuretic peptide. LA: left atrium, AO: aorta.

Fig. 3
Receiver operator characteristic curve determines the B-type natriuretic peptide cutoff value for detecting hemodynamically significant patent ductus arteriosus in preterm infants.
References
1. Bancalari E, Claure N, Gonzalez A. Patent ductus arteriosus and respiratory outcome in premature infants. Biol Neonate. 2005. 88:192–201.
2. Clyman RI. Ductus arteriosus: current theories of prenatal and postnatal regulation. Semin Perinatol. 1987. 11:64–71.
3. Heymann MA, Rudolf AM. Control of the ductus arteriosus. Physiol Rev. 1975. 55:62–78.
4. Clyman RI. Mechanisms regulating the ductus arteriosus. Biol Neonate. 2006. 89:330–335.
5. Rojas MA, Gonzalez A, Bancalari E, Claure N, Poole C, Silva-Neto G. Changing trends in the epidemiology and pathogenesis of neonatal chronic lung disease. J Pediatr. 1995. 126:605–610.
6. Kluckow M, Evans N. Ductal shunting, high pulmonary blood flow, and pulmonary hemorrhage. J Pediatr. 2000. 137:68–72.
7. Hammerman C. Patent ductus arteriosus: clinical relevance of prostaglandins and prostaglandin inhibitors in PDA pathophysiology and treatment. Clin Perinatol. 1995. 22:457–479.
8. Cotton RB, Stahlman MT, Kovar I, Catterton WZ. Medical management of small preterm infants with symptomatic patent ductus arteriosus. J Pediatr. 1978. 92:467–473.
9. Walther FJ, Benders MJ, Leighton JO. Persistent pulmonary hypertension in premature neonates with severe respiratory distress syndrome. Pediatrics. 1992. 90:899–904.
10. Flynn PA, da Graca RL, Auld PA, Nesin M, Kleinman CS. The use of a bedside assay for plasma B-type natriuretic peptide as a biomarker in the management of patent ductus arteriosus in premature neonates. J Pediatr. 2005. 147:38–42.
11. Holmström H, Hall C, Thaulow E. Plasma levels of natriuretic peptides and hemodynamic assessment of patent ductus arteriosus in preterm infants. Acta Paediatr. 2001. 90:184–191.
12. Daniels LB, Maisel AS. Natriuretic peptides. J Am Coll Cardiol. 2007. 50:2357–2368.
13. Cantinotti M, Clerico A, Murzi M, Vittorini S, Emdin M. Clinical relevance of measurement of brain natriuretic peptide and N-terminal pro-brain natriuretic peptide in pediatric cardiology. Clin Chim Acta. 2008. 390:12–22.
14. Reynolds EW, Ellington JG, Vranicar M, Bada HS. Brain-type natriuretic peptide in the diagnosis and management of persistent pulmonary hypertension of the newborn. Pediatrics. 2004. 114:1297–1304. Erratum in: Pediatrics 2005;115:1454.
15. Puddy VF, Amirmansour C, Williams AF, Singer DR. Plasma brain natriuretic peptide as a predictor of haemodynamically significant patent ductus arteriosus in preterm infants. Clin Sci (Lond). 2002. 103:75–77.
16. Attridge JT, Kaufman DA, Lim DS. B-type natriuretic peptide concentrations to guide treatment of patent ductus arteriosus. Arch Dis Child Fetal Neonatal Ed. 2009. 94:F178–F182.
17. Evans N. Diagnosis of patent ductus arteriosus in the preterm newborn. Arch Dis Child. 1993. 68(1 Spec No):58–61.
18. Skelton R, Evans N, Smythe J. A blinded comparison of clinical and echochardiographic evaluation of the preterm infant for patent ductus arteriosus. J Paediatr Child Health. 1994. 30:406–411.
19. Skinner J. Diagnosis of patent ductus arteriosus. Semin Neonatol. 2001. 6:49–61.
20. Tammela O, Ojala R, Iivainen T, et al. Short versus prolonged indomethacin therapy for patent ductus arteriosus in preterm infants. J Pediatr. 1999. 134:552–557.
21. El Hajjar M, Vaksmann G, Rakza T, Kongolo G, Storme L. Severity of the ductal shunt: a comparison of different markers. Arch Dis Child Fetal Neonatal Ed. 2005. 90:F419–F422.
22. Young TE, Mangum B. Neofax: a Manual of Drugs Used in Neonatal Care. 2007. 20th ed. Montvale, NJ: Thompson Healthcare.
23. Levin ER, Gardner DG, Samson WK. Natriuretic peptides. N Engl J Med. 1998. 339:321–328.
24. Da Graca RL, Hassinger DC, Flynn PA, Sison CP, Nesin M, Auld PA. Longitudinal changes of brain-type natriuretic peptide in preterm neonates. Pediatrics. 2006. 117:2183–2189.
25. Lee HS, Choi WS, Choi BM, et al. Usefulness of B-type natriuretic peptide assay in predicting symptomatic patent ductus arteriosus in preterm infants. J Korean Soc Neonatol. 2004. 11:44–53.
26. Choi BM, Lee KH, Eun BL, et al. Utility of rapid B-type natriuretic peptide assay for diagnosis of symptomatic patent ductus arteriosus in preterm infants. Pediatrics. 2005. 115:e255–e261.
27. Hsu JH, Yang SN, Chen HL, Tseng HI, Dai ZK, Wu JR. B-type natriuretic peptide predicts responses to indomethacin in premature neonates with patent ductus arteriosus. J Pediatr. 2010. 157:79–84.
28. Tomaru Ki K, Arai M, Yokoyama T, et al. Transcriptional activation of the BNP gene by lipopolysaccharide is mediated through GATA elements in neonatal rat cardiac myocytes. J Mol Cell Cardiol. 2002. 34:649–659.
29. Ueda S, Nishio K, Akai Y, et al. Prognostic value of increased plasma levels of brain natriuretic peptide in patients with septic shock. Shock. 2006. 26:134–139.
30. El-Khuffash A, Molloy EJ. Are B-type natriuretic peptide (BNP) and N-terminal-pro-BNP useful in neonates? Arch Dis Child Fetal Neonatal Ed. 2007. 92:F320–F324.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download