Abstract
Background and Objectives
Subjects and Methods
Results
Conclusion
Figures and Tables
Fig. 1

Fig. 2

Fig. 3

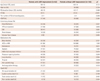
Table 1
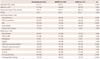
*ICMP vs. NICMP. NICMP: non-ischemic cardiomyopathy, ICMP: ischemic cardiomyopathy, SD: standard deviation, F/U: follow-up, EF: ejection fraction, HTN: hypertension, DM: diabetes mellitus, ACEI: angiotensin-converting-enzyme inhibitor, ARB: angiotensin II receptor blocker, HMG-CoA: hydroxymethylglutaryl CoA
Table 3
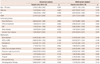
*Adjusted with age (>70 years old), sex, EF, ICMP, atrial fibrillation, HTN, DM, renal disease, valvular heart disease, beta-blockers, ACEI or ARB, amiodarone, digitalis, HMG-CoA reductase inhibitor, potassium sparing diuretics, loop diuretics, thiazide, anti-platelet drug, and anticoagulation. CI: confidence interval, EF: ejection fraction, ICMP: ischemic cardiomyopathy, HTN: hypertension, DM: diabetes mellitus, ACEI: angiotensin-converting-enzyme inhibitor, ARB: angiotensin II receptor blocker, HMG-CoA: hydroxymethylglutaryl CoA
Table 4
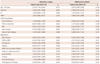
*Adjusted with age (>70 years old), sex, EF, ICMP, atrial fibrillation, HTN, DM, renal disease, valvular heart disease, beta-blockers, ACEI or ARB, amiodarone, digitalis, HMG-CoA reductase inhibitor, potassium sparing diuretics, loop diuretics, thiazide, anti-platelet drug, and anticoagulation. CI: confidence interval, EF: ejection fraction, ICMP: ischemic cardiomyopathy, HTN: hypertension, DM: diabetes mellitus, ACEI: angiotensin-converting-enzyme inhibitor, ARB: angiotensin II receptor blocker, HMG-CoA: hydroxymethylglutaryl CoA
Table 5
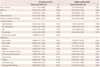
*Adjusted with age (>70 years old), sex, EF, revascularization, previous myocardial infarction, atrial fibrillation, HTN, DM, renal disease, valvular heart disease, beta-blockers, ACEI or ARB, amiodarone, digitalis, HMG-CoA reductase inhibitor, potassium sparing diuretics, loop diuretics, thiazide, anti-platelet drug, and anticoagulation. †Adjusted with age (>70 years old), sex, EF, revascularization, previous myocardial infarction, atrial fibrillation, HTN, DM, renal disease, beta-blockers, ACEI or ARB, amiodarone, digitalis, HMG-CoA reductase inhibitor, potassium sparing diuretics, loop diuretics, thiazide, anti-platelet drug, and anticoagulation. CI: confidence interval, EF: ejection fraction, ICMP: ischemic cardiomyopathy, HTN: hypertension, DM: diabetes mellitus, ACEI: angiotensin-converting-enzyme inhibitor, ARB: angiotensin II receptor blocker, HMG-CoA: hydroxymethylglutaryl CoA
Table 6
LVEF improvement: improvement of >25% in the LV systolic function compared to the baseline. *p estimated by chi-square methods except classification of deaths, †p estimated by Kaplan-Meier curve and log-rank test. ICMP: ischemic cardiomyopathy, SD: standard deviation, F/U: follow-up, EF: ejection fraction, HTN: hypertension, DM: diabetes mellitus, ACEI: angiotensin-converting-enzyme inhibitor, ARB: angiotensin II receptor blocker, LVEF: left ventricular ejection fraction




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download