Abstract
Background and Objectives
Anticoagulation with vitamin K antagonists (VKAs) such as warfarin provides effective stroke prophylaxis in patients with atrial fibrillation (AF). We conducted a large multicenter survey of Korean patients with AF to determine trends in VKA use.
Subjects and Methods
Eligible patients were adults with AF that had been prescribed VKAs. Medical records from a total of 5616 patients {mean age 63.6±12.2 years, male 3150 (56.1%)} in 27 hospitals from Jan. 2001 to Oct. 2007 were reviewed.
Results
The mean international normalized ratio (INR) was 2.04±0.64, and mean dosage of VKA was 3.66±1.50 mg. Individuals in their sixties (1852 patients) accounted for about one third of patients studied. As patients grew older, INR increased and VKA dosage decreased. The dosage of VKA in male patients was larger than that in females for all ages. A total of 2146 (42.4%) patients had an INR of 2-3, and less than 40% patients in their sixties had an INR within optimal range. The dosage of oral anticoagulant for optimal INR level was 3.71 mg.
Since its first electrocardiographic description in 1909, atrial fibrillation (AF) has been recognized as a common arrhythmia, and more recently it has been associated with increased cardiovascular morbidity and mortality. With a prevalence of 1% among the adult population, AF is the most common arrhythmia that requires treatment. Current treatment guidelines recommend long-term oral anticoagulation with a vitamin K antagonist (VKA), such as warfarin, that is targeted at an international normalized ratio (INR) of 2.5 (range, 2.0 to 3.0) in patients with AF who are at a moderate to high risk of stroke based on the presence of two or more of the following risk factors: 1) age >75 years; 2) history of hypertension; 3) diabetes mellitus; and 4) moderately or severely impaired left ventricular systolic function and/or heart failure.1)2) However anticoagulants can cause severe adverse events, and physicians should therefore monitor the INR of patients taking these drugs to ensure that their ratios fall within a target range.3) Furthermore, anticoagulation with VKAs has many limitations. VKAs offer a narrow therapeutic range of INR of 2.0-3.0; consequently, when INR levels fall below this target range, patients are at an increased risk of ischemic stroke, and when they exceed 3.0, the risk of bleeding is increased. Therefore, frequent INR monitoring and dose adjustments are required. Furthermore, anticoagulation intensity can be influenced by multiple drug and food interactions, as well as by alcohol consumption. Therefore, patients taking VKAs have to be cautious about concomitant drug use and adhere to dietary and lifestyle restrictions.4) As Western countries as well as Korea are confronted with aging populations and an increasing prevalence of obesity, the number of patients with AF is expected to rise sharply over the next 50 years.5) There are racial/ethnic differences in the prevalence of certain polymorphisms in genes that influence warfarin pharmacokinetics and pharmacodynamics (e.g. cytochrome P450 2C9 and vitamin K epoxide reductase). The Asian population generally appears to require the lowest daily dose of warfarin to maintain a given INR target, whereas the White population requires an intermediate daily dose and the Black population requires the highest daily dose.6) Thus, estimating INR in the context of AF in Korea is important, however only a few studies of this kind have been conducted. We conducted a large multicenter survey of Korean patients with AF to determine trends in oral anticoagulation use. The aim of this study was to investigate the proportion of patients with optimal range INR and the dosage of oral anti-coagulation to achieve the optimal range according to age and gender in the Korean population.
This retrospective KORean Atrial Fibrillation investigation (KORAF) was conducted with patient medical record information collected between January, 2000 and October, 2007 in 27 Korean hospitals. Patients eligible for inclusion were adults with documented AF who had been taking VKAs for at least 1 year and with INR monitoring for more than two occasions. We excluded data from patients who received antiplatelet medications with their anticoagulants. We studied average INR levels according to age and average dosage of oral anticoagulant. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) version 15.0 for Windows (SPSS Inc., Chicago, IL, USA)
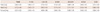
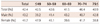
In total, 5616 patients were included in this study. The mean age of the surveyed population was 63.5±12.3 years and 56.1% were male. Patients were divided into age groups: below 50, 50-59, 60-69, 70-74, and over 75 years old. The average INR level was 2.04. There was a significant difference in INR level according to age group (Table1). Fig. 1 shows that the mean INR level of older patients was slightly higher than that of younger patients. Generally, old age is a high risk for stroke, so physicians want to maintain a higher INR in older patients. The mean dosage of oral anticoagulant was 3.66±1.59 mg. There was significant difference in dosage of oral anticoagulant according to age group (Table 2, Fig. 2). The dosage of oral anticoagulant decreased with increasing age. Table 3 and Fig. 3 show the average dosage of oral anticoagulant according to the INR group. The dosage of oral anticoagulant in the lower INR group was higher than in the higher INR group. An average 3.89 mg of oral anticoagulant was prescribed to individuals with INR over 3.5 in the male group, denoting possible drug over-prescription. In contrast, an average of 3.48 mg of oral anticoagulant was prescribed to individuals with INR 1-1.4, possibly indicating drug under-prescription. The proportion of individuals achieving an optimal INR level (2-3) was only 42.4% (Fig. 4). An INR of 1.5-2 was maintained in one-third of patients, while patients with INR below 2 accounted for more than half (51.3%) the cases studied. The proportion of individuals achieving optimal INR level was higher among younger women and older men (Table 4, Fig. 5). The dosage of oral anticoagulant to achieve an optimal INR level was 3.71 mg (Table 5, Fig. 6). With increasing age, the higher INR level was preserved with a lower dosage of oral anticoagulant. The dosage of oral anticoagulant in men was slightly higher than in women, and as shown in Fig. 6, the difference gradually decreased with increasing age.
This study provides insight into the proportion of individuals achieving optimal-range INR and oral anticoagulant dosage in Korean patients with AF. Among Korean patients with AF on VKAs, less than half reached therapeutic range levels of INR and the mean dosage of oral anticoagulant was 3.66 mg, which decreased with increasing age. The dosage of oral anticoagulant to achieve optimal INR levels was 3.71 mg.
Almost all studies have shown that AF is a potent risk factor for stroke, increasing its risk by nearly 5- fold; adjusted dose warfarin reduced the annual rate of any stroke by 68%.7)8) Besides anticoagulant use, it is necessary to use medications for rate and rhythm control.9) Compared with aspirin, oral anticoagulant use significantly decreases the risk of all strokes and cardiovascular events for patients with nonvalvular chronic or paroxysmal AF.10) While the prevalence of AF was 0.4% in Korean individuals that were 40-69 years of age,5) it may increase with the aging population rendering AF a public health problem of major concern.
This study was conducted as a large multicenter survey of Korean patients with AF to gain insight into trends of oral anti-coagulation use. The average INR level was 2.04 for AF patients. This level is within the therapeutic range for prevention of stroke. However, an optimal INR level (2-3) was achieved in only 42.4% of cases studied. In over half of the patients with AF, the INR value was out of range, especially in the sub-therapeutic range, which is of particular concern because of the increased risk of ischemic stroke. Subtherapeutic INR levels of less than 2.0 have been associated with more thromboembolic events and severe strokes.11) In this study, the mean dosage of oral anticoagulant was 3.66 mg, which decreased with age. Age of greater than 80 years and perceived bleeding risk were the most often cited reasons for not prescribing warfarin.12) For this reason, the proportion of optimal INR was higher in younger women and older men. With increasing age, dosage of oral anticoagulant needed to achieve optimal INR level (2-3) decreased. Therefore, when physicians prescribe oral anticoagulants to older patients with AF, dosage of oral anticoagulant needs to be decreased relative to that given to younger patients with AF. However patients with subtherapeutic INR have an increased risk of ischemic stroke, hence frequent INR monitoring and dose adjustments are required in older patients with AF. Physicians should adjust their clinical practices accordingly by aggressively correcting sub-therapeutic INR and avoiding overreaction to INR that narrowly exceeds 3.
Non-whites are at greater risk for several subtypes of ischemic stroke; cardioembolic stroke attributable to AF is more frequently implicated in Whites.13) In a recent systematic review of 67 anticoagulation studies (69% of which were for AF) by van Walraven et al.14) patients were in the therapeutic range 63.6% of the time overall in the USA. The percent-time on warfarin did not differ by race and ethnicity. The same study reported that Whites, Hispanic, and Asians had similar achieved anticoagulation intensity, however Blacks spent more time in the sub-therapeutic range (INR <2), which likely contributed to the observed absence of stroke reduction. The median percent-time on warfarin when INR was 2 to 3 was 54.5% overall, but it was lower in Blacks at 47.8% while the other groups had a rate of about 54%.6)
In Japan, in order to prevent stroke in AF, lower INR (1.6-2.6) was recommended for elderly patients15) and with a mean daily dose of warfarin of 2.68±0.95 mg, INR was 1.99±0.24. The INR did not correlate with increasing age.16) Moreover, warfarin was used extensively in patients with AF whose stroke risk was relatively low with half of them having CHADS2 scores of 0 to 1.17) In Japan, lower INR values were recommended and the dose of warfarin was lower than in Korean patients.
This study showed that the dosage of oral anticoagulants that was needed to achieve an optimal INR level was 3.71 mg in Korean patients. The proportion of patients with optimal INR was lower than in other countries. An effort to maintain optimal INR therefore will be required.
There were several limitations in our study. This study had the inherent limitation of its retrospective nature. Various methods of patient recruitment were used in different hospitals; hence generalizing among hospitals may be problematic. The relationship between INR level and rates of major adverse cardiac events was not studied. It is clear that much additional work will be required and it is hoped that this study will stimulate further investigation. However, findings of this study should help reduce future cardiovascular disease events and better understand AF in Korea.
In conclusion, in Korean patients with AF, less than half of the cases on oral anticoagulant reached the therapeutic range of INR. Mean dosage of VKA was 3.66±1.59 mg, and the dosage of oral anticoagulant to achieve optimal INR level was 3.71 mg, which decreased with increasing age.
Figures and Tables
Fig. 1
Average INR level according to age group. The mean INR level of older patients was slightly higher than that of younger patients. INR: international normalized ratio.

Fig. 2
Average dosage of oral anticoagulant according to age group. There was significant difference in dosage of oral anticoagulant according to age group. OAC: oral anticoagulant.
Fig. 3
Average dosage of oral anticoagulant according to INR group. The dosage of oral anticoagulant in the lower INR group was higher than that in higher INR group. INR: international normalized ratio.
Fig. 4
Proportion of INR level in patient with AF who taken oral anticoagulants. The proportion of individuals achieving an optimal INR level (2-3) was only 42.4%. INR: international normalized ratio, AF: atrial fibrillation.
Fig. 5
Proportion of optimal INR level (2-3) according to age group. The proportion of individuals achieving optimal INR level was higher among younger women and older men. INR: international normalized ratio.

Acknowledgments
This study was performed with the support of the Korean Society of Circulation in celebration of the 50th Anniversary of the Korean Society of Circulation.
References
1. Singer DE, Albers GW, Dalen JE, et al. Antithrombotic therapy in atrial fibrillation: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008. 133:6 Suppl. 546S–592S.
2. Fuster V, Rydén LE, Cannom DS, et al. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 Guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in partnership with the European Society of Cardiology and in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. J Am Coll Cardiol. 2011. 57:e101–e198.
3. Lip GY, Agnelli G, Thach AA, Knight E, Rost D, Tangelder MJ. Oral anticoagulation in atrial fibrillation: a pan-European patient survey. Eur J Intern Med. 2007. 18:202–208.
4. Ansell J, Hirsh J, Poller L, Bussey H, Jacobson A, Hylek E. The pharmacology and management of the vitamin K antagonists: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004. 126:3 Suppl. 204S–233S.
5. Lee KS, Choi SJ, Park SH, Kim HL, Min H, Park HY. Prevalence of atrial fibrillation in middle-aged people in Korea: the Korean Genome and Epidemiology Study. Korean Circ J. 2008. 38:601–605.
6. Shen AY, Chen W, Yao JF, Brar SS, Wang X, Go AS. Effect of race/ethnicity on the efficacy of warfarin: potential implications for prevention of stroke in patients with atrial fibrillation. CNS Drugs. 2008. 22:815–825.
7. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation: a major contributor to stroke in the elderly: the Framingham Study. Arch Intern Med. 1987. 147:1561–1564.
8. Laupacis A, Boysen G, Connolly S, et al. Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation: analysis of pooled data from five randomized controlled trials. Arch Intern Med. 1994. 154:1449–1457.
9. Kim YH. Rhythm control versus rate control of atrial fibrillation: pharmacologic and non-pharmacologic therapy. Korean Circ J. 2003. 33:553–558.
10. van Walraven C, Hart RG, Singer DE, et al. Oral anticoagulants vs aspirin in nonvalvular atrial fibrillation: an individual patient meta-analysis. JAMA. 2002. 288:2441–2448.
11. Hylek EM, Go AS, Chang Y, et al. Effect of intensity of oral anticoagulation on stroke severity and mortality in atrial fibrillation. N Engl J Med. 2003. 349:1019–1026.
12. Waldo AL, Becker RC, Tapson VF, Colgan KJ. NABOR Steering Committee. Hospitalized patients with atrial fibrillation and a high risk of stroke are not being provided with adequate anticoagulation. J Am Coll Cardiol. 2005. 46:1729–1736.
13. Stansbury JP, Jia H, Williams LS, Vogel WB, Duncan PW. Ethnic disparities in stroke: epidemiology, acute care, and postacute outcomes. Stroke. 2005. 36:374–386.
14. van Walraven C, Jennings A, Oake N, Fergusson D, Forster AJ. Effect of study setting on anticoagulation control: a systematic review and me-taregression. Chest. 2006. 129:1155–1166.
15. Yasaka M, Minematsu K, Yamaquchi T. Optimal intensity of international normalized ratio in warfarin therapy for secondary prevention of stroke in patients with non-valvular atrial fibrillation. Intern Med. 2001. 40:1183–1188.
16. Miura T, Nishinaka T, Terada T, Yonezawa K. Relationship between aging and dosage of warfarin: the current status of warfarin anticoagulant therapy for Japanese outpatients in a department of cardiovascular medicine. J Cardiol. 2009. 53:355–360.
17. Atarashi H, Inoue H, Okumura K, Yamashita T, Kumagai N, Origasa H. J-RHYTHM Registry Investigators. Present status of anticoagulation treatment in Japanese patients with atrial fibrillation: a report from the J-RHYTHM Resistry. Circ J. 2011. 75:1328–1333.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download